Nadiyya Hamid1, Somia Faisal2*, Nabeela Safdar3, Hafiz Muhammad Asim4
1Student, Lahore College of Physical Therapy, Lahore Medical and Dental College Lahore, Pakistan![]()
2*Demonstrator, Lahore College of Physical Therapy, Lahore Medical and Dental College Lahore, Pakistan![]()
3Assistant Professor, Lahore College of Physical Therapy, Lahore Medical and Dental College Lahore, Pakistan![]()
4Lahore Medical and Dental College Lahore, Pakistan![]()
ABSTRACT
Background of the study: Tibia Vara is defined as a growth abnormality which leads to Varus malalignment of the lower limb. It is caused by excessive loading on the medial part of proximal tibia. Progressive Tibia Vara can result in a bowleg deformity which is most noticeable in posteromedial part of upper tibial physis. Other than that, it gives rise to in toeing of feet and lateral knee thrust, altering the normal biomechanics of an individual. This study aim to determine the frequency of Tibia Vara among obese adolescents (13-18years).
Methodology: A descriptive cross-sectional study was done using non probability convenient sampling. Total 214 obese adolescents of age range 13 to 18 years were recruited from different parks and schools of Lahore. Adolescents with BMI less than 30 and with history of fracture or dislocation in the lower limb were excluded from the study. Manual goniometer was used to assess tibia vara in obese adolescent which had an intra-rater reliability of 0.75.
Results: Out of 214 obese adolescents, 128 were male and 86 were female. The percentage of Tibia Vara in this population was found to be 38% (n= 82). Whereas; on the basis of gender, male participants presenting with Tibia vara was found to be 26% (n= 56) and the percentage of females reported with Tibia vara was only 12% (n= 26).
Conclusion: Tibia vara had been reported in 38% of the obese adolescents in Lahore, Pakistan. Whereas, on the basis of gender most frequently tibia vara was reported among male participants.
Keywords: Adolescents, juvenile, biomechanics, blount disease, obesity, sedentary lifestyle, slipped capital femoral epiphysis.
Introduction
Tibia Vara is defined as a growth abnormality which leads to an excessive inward angulation or medial angulation of the lower limb. It is caused by excessive loading on medial part of proximal tibial cartilage1,2. It is characterized on the basis of onset into three groups; infantile onset (< 3 years), juvenile onset (4 -10 years) & adolescent onset occur after 10 years of age 3-5 Progressive Tibia Vara can result in bowleg deformity, in-toeing of feet and lateral knee thrust, altering the normal biomechanics of an individual6,8. However; early onset Tibia Vara is reported to have a prevalence of 1/1200 live births in Caribbean 9 In the city of Karad, India the prevalence of Tibia Vara was found to be 11.33 %10. The metaphyseal-diaphyseal angle (MD) of tibia is used to assess the degree of bowing among tibia vara adolescence. The metaphyseal- diaphyseal angle (MD) of tibia is angle that is being created by intersecting line through the transverse plane of the proximal tibial metaphysis with line perpendicular to the long axis of the tibial diaphysis. The angle ranging from 9 to 16 degrees or more has a higher risk to progress to varus deformity. Moreover, the rate at which the tibial metaphyseal angle changes is a predictor of Blounts disease for physicians11,13. This deformity comprises of three components including Varus (deviation of distal portion towards the midline), Procurvatum (backward bending of the bone) and internal torsion of the tibia. Most likely the cause of Tibia Vara is excess compressive force on upper medial aspect of tibia altering the enchondral formation of bone. Therefore, it has been widely related to Obesity. Predisposing factors apart from obesity include large stature, early walking in children or combination of these factors14,17. Adolescent obesity which occurs in the age of 10-19 years is mostly caused by sedentary lifestyle and consumption of additional calories than the required amount18,20. Musculoskeletal problems known to be associated with adolescent obesity are Tibia Vara or Blount’s disease and Slipped Capital Femoral Epiphysis21,22. Other causes of tibia vara may include incomplete closure of the physic followed by a traumatic incident or infection. Basically, what happens in an obese individual is that the increased load and excess fat especially in the thigh region leads to progressive Varus deviation of tibia from its normal alignment. The compressive stress has more impact on tibia than on femur because comparatively the structure of tibia is three dimensionally weaker23.The stress on young bone resulting from excess adiposity, acts to produce changes which are associated with Blount’s disease. Moreover, the results of routine lab investigations in patients with Blount’s disease are usually within normal range which is how it can be differentiated from deformity caused by any other metabolic bone disease like Rickets24. The way to access Tibia Vara is mostly through Radiographs of the patients but alternatively, a Manual Goniometer can be used to determine degree of deformity25. The reliability of manual goniometer to measure degree of tibial torsion is found to be 0.7526. The aspect of Tibia vara in obese adolescents is under research and sufficient evidence is not yet available in Pakistan. Due to lack of symptoms and obesity obsecuring the severity of magnitude of deformity & general lack of awareness regarding this condition commonly delay the diagnosis. Therefore, the rationale of the current study is to help Physical therapists to consider the characteristics of Tibia vara in obese adolescents and assist them in early evaluation of this condition and to limit its progression.
Methodology
Study Design and Sampling Technique
A descriptive cross-sectional study conducted on 214 participants during the period of June 2020 to January 2021. The participants were recruited from the following parks and schools of Lahore (Central Park – NFC society, Fish Park – Wapda town, Pak-Turk Maarif International School and College for Boys, Lahore Grammar School Valencia branch and Mus’ab School system). Non-probability convenience sampling was used. Study had been approved by ethical board of Lahore College of physical therapy. Sample size calculated was 214 using World Health Organization (WHO) Sample Size Calculator. The sample size was calculated to be n=214 with 95% confidence interval, anticipated population proportion p=0.07527 and absolute precision d=0.05.
Study Participants and Selection Criteria
The study participants included were both male and female obese adolescents with age ranges from 13 to 18 years. Whereas, Individuals hesitating to expose their lower leg and individuals with history of fracture or dislocation in the lower limb were excluded from the study. Written informed consent from the child’s legal guardian was taken before data collection.
Data collection tool and Procedure
Manual goniometer was used to assess tibia vara in obese adolescent. Each subject was asked to stand on a flat surface (floor) with both feet slightly apart but at the same level. The individual was asked to stand in single leg stance (the foot of leg to be measured was kept in contact with the floor and foot of opposite leg on toes). Examiner sat directly behind the individual and detects a line dividing the back of leg to be measured into two equal halves, a line is drawn from upper two third of the posterior leg to top of the ankle. The angle between this drawn line and the ground is recorded as degree of Tibia Vara. The movable arm of goniometer was kept on that line while the stationary arm of goniometer was kept parallel to the floor. The angle formed was measured and subtracted from normal LDTA (lateral distal tibial angle) which is about 90 degrees28. This angle was referred to as the degree of Tibia Vara. If the value of angle is 9o or >9o than tibia vara is present. The same procedure was repeated for the other leg. Goniometric measure of this angle has a good intra-rater reliability of 0.7529.
Data Analysis Strategy
Data was analyzed through SPSS version 21. Mean and standard deviation as Descriptive statistics were used to demonstrate numerical variable and for categorical variable frequency and percentage was calculated.
Results
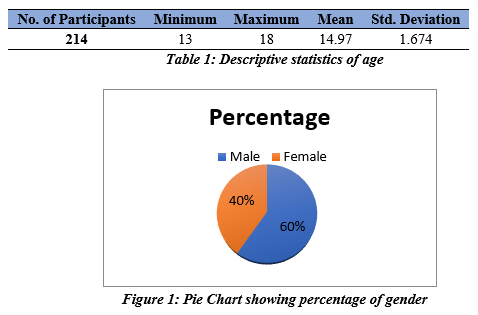
Out of 214 participants, the minimum age of participants was 13 years; maximum age 18 years with a mean age was of 14.97 and standard deviation (SD) of 1.674 as shown in table 1. Whereas, 59.8% (n=128) of the participants were males and 40.2% (n=86) were females as show in figure 1.
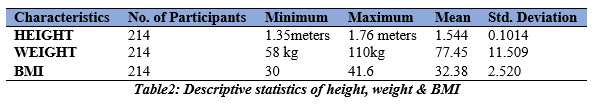
Descriptive statistics of height, weight and BMI of participants were shown in table 2. Out of 214 participants, the minimum height of the participants were 1.35 meters and the maximum height reported was 1.76 meters. Whereas, the mean and standard deviation of the height was (1.544±0.101). Similarly, the minimum weight of the participants was 58 kg and the maximum weight reported was 110 kg. Hence, the mean and standard deviation of the weight was (77.45±11.509). Likewise, the minimum BMI of the participants was found to be 30 and the maximum BMI reported was 41.6. Thus, the mean and standard deviation of the BMI was (32.38±2.520).
Out of 214 obese participants the percentage of participants in which tibia vara was found was only 38% (n = 82); whereas, in 62% (n = 132) of the obese adolescents’ tibia vara was not reported as shown in figure 2.
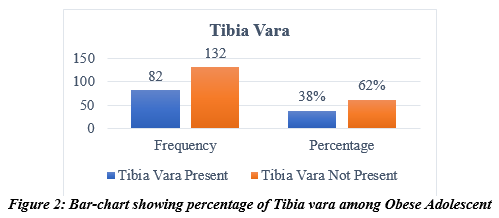
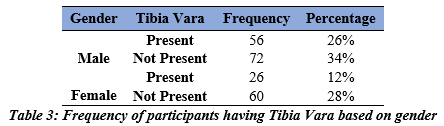
Whereas; on the basis of gender most frequently the tibia vara was reported among male participants. Hence, male participants presenting with Tibia vara was found to be 26% (n= 56) and the percentage of females reported with Tibia vara was only 12% (n= 26) as shown in table 3. However, tibia vara was not found among 34 % (n = 72) male participants and 28% (n = 60) of the female participants.
Discussion
The current study focused to determine the frequency of tibia vara among obese adolescents. The study was first of its kind to be conducted in Pakistan. Rahane et.al conducted research in 2020 to determine the incidence of Tibia Vara by using tibial torsion test among children and it was found to be present among majority of children. Moreover, it was also found that severity of Tibia Vara is more likely to increase if the lateral distal tibial angle ranges from 9-16 degrees10. However, the results of current study showed that Tibia vara had been reported in obese adolescents and percentage of Tibia vara was higher in males than in female’s obese adolescents.
Janoyer et al. in 2019 observed that some children’s whose tibia vara was found to be 9 degrees or more need attention and proper guidelines to limit this progression. They may also require surgical intervention in the future if the deformity gets worse and causes pain or hindrance in their activities of daily living23. Hence, the current study was conducted to early identify the presence of tibia vara among obese adolescent as obesity obscures the magnitude of the deformity and to create a general sense of awareness regarding this condition as early identification can limit its progression.
In 2019 MOHAMED, M., et al. conducted a study on adolescent and found that participants were hesitated to stand in single leg stance (SLS) to get their tibia vara assessed using goniometer. They had fear of losing balance and fall. Hence, they were asked to stand close to a wall or barrier to which they could hold on to during SLS. Moreover, he also found that very few obese children with shorter heights complained of pain on walking and a lateral thrust on weight bearing30. Similarly, in the current study a manual goniometer was used to measure the degree of tibia vara in both legs of the participants. Each subject was asked to stand on a flat surface with both feet slightly apart but at the same level. The individual was asked to stand in single leg stance. Examiner sat directly behind the individual and detects a line dividing the back of leg to be measured into two equal halves, a line is drawn from upper two third of the posterior leg to top of the ankle. The angle between this drawn line and the ground is recorded as degree of Tibia Vara. Hence, it was found to be reported in 82 participants out of 214.
Dunphy et al. conducted a study in 2016 and found that people who quite oftenly shift their weight on to one of their legs, pelvis of that particular side drops and contributes to increased weight on the medial compartment of knee. This frequent increased loading causes that leg to move in to adduction hence increased varus of the tibia which can be the reason of difference in measurements of tibia vara for both legs of the participants31. Whereas, the results of current study showed only the frequency of the Tibia Vara with both male and female obese adolescents showed varying degrees of Tibia vara in both their legs. However, the incidence of tibia vara on dominant leg was not reported but it can be supposed that individuals who tend to lean on to their left legs while standing adds more weight to that leg increases the likelihood of tibia vara on that leg.
Thus, beside obesity as a predisposing factor of tibia vara other factors also found to be associated with tibia vara which include short stature and early walking (walking before the age of ten months) in children. In a study conducted in 2020 Wongcharoenwatana et al observed that the younger children with short stature showed more defined bowed legs and hence varus deformity in the tibia as compared to older children because tibia vara usually results in stunted growth, thus the tibia fails to elongate further32.
A case study conducted by Mohammed Zayer reported the presence of unilateral tibia vara in child with history of early walking. The study reported that girl’s right knee exhibited a progressive varus deformity at the age of eight months, when she first learned to walk. There was no family history of bone diseases, trauma, infections, or pre- or postnatal abnormalities. Her right leg developed a significant varus deformity and medial tibial torsion at the age of one. Typical lesion in the right leg was seen on radiographs which occur due to fibrocartilaginous dysplasia33.
Furthermore, in 2020 Alsancak et al. carried out a cross-sectional study on children with tibia vara and reported that aberrant increases in knee internal rotation and hip external rotation, as well as ligamentous laxity and lateral knee thrust during the stance phase of gait, have been reported as contributing variables which leads to tibia vara. In addition to the proximal tibia, the distal and proximal femur, and the ankle are all affected by tibia vara to variable degrees. Femoral anteversion, on the other hand, is also increased34.
Generalizability of the study could be questioned; consequently, further studies should be done to find the association of infantile form (early onset) Tibia vara with obesity. Whereas, the gold standard for measurement of Tibia vara is through angles marked radiographically should be adopted.
Conclusion
Tibia vara had been reported in 38% of the obese adolescents in Lahore, Pakistan. Both male and female obese adolescents showed varying degrees of Tibia vara in both their legs. Whereas, on the basis of gender most frequently tibia vara was reported among male participants
AUTHORS’ CONTRIBUTION:
The following authors have made substantial contributions to the manuscript as under:
Conception or Design: Nadiyya Hamid
Acquisition, Analysis or Interpretation of Data: Somia Faisal
Manuscript Writing & Approval: Nabeela Safdar, Hafiz Muhammad Asim
All authors acknowledge their accountability for all facets of the research, ensuring that any concerns regarding the accuracy or integrity of the work are duly investigated and resolved.
ACKNOWLEDGEMENTS: The authors thank the Dean of Lahore College of Physical Therapy for his endless support and guidance.
INFORMED CONSENT: (dealing with studies involving human subjects).
CONFLICT OF INTEREST: None
FUNDING STATEMENTS: None
ETHICS STATEMENTS: The protocol of the present study was registered by the local ethics committee of Lahore College of Physical Therapy LCPT/DPT16/538.
References
- Murphy RF, Pacult MA, Barfield WR, Mooney III JF. Hemiepiphyseodesis for juvenile and adolescent tibia vara utilizing percutaneous transphyseal screws. Journal of Pediatric Orthopaedics. 2020 Jan 1;40(1):17-22.
- Khaled M, Said G, Abubeih H, El-Sherif E. Acute correction of adolescent tibia vara with biplanar medial opening wedge osteotomy without a graft. Current Orthopaedic Practice. 2019 Jan 1;30(1):47-9.
- Danino B, Rödl R, Herzenberg JE, Shabtai L, Grill F, Narayanan U, Gigi R, Segev E, Wientroub S. The efficacy of guided growth as an initial strategy for Blount disease treatment. Journal of children’s orthopaedics. 2020 Aug;14(4):312-7.
- Zein AB, Elhalawany AS, Ali M, Cousins GR. Acute correction of severe complex adolescent late-onset tibia vara by minimally invasive osteotomy and simple circular fixation: a case series with 2-year minimum follow-up. BMC Musculoskeletal Disorders. 2021 Dec;22(1):1-7.
- Vasiliadis AV, Maris A, Gadikoppula S. Tibia vara or Blount’s disease: Why an early diagnosis and treatment are important?. Clinics and Practice. 2020 Mar;10(1):15-6.
- Kawasaki M, Nagamine R, Chen W, Ma Y, Sakai A, Suguro T. Proximal tibia vara involves the medial shift of the tibial articular surface. Journal of Orthopaedic Surgery. 2020 Feb 17;28(1):2309499020902592.
- Othman M, Abdelwahab AM, Abdelfattah M. Treatment of severe early-onset Blount’s disease by simultaneous medial hemiplateau elevation and metaphyseal osteotomy using the Ilizarov fixator. International Journal of Orthopaedics. 2018;4(3):486-93.
- Bent MA, Stork NC, Nemeth BA. The diagnosis and management of common childhood orthopedic disorders: An update. Current problems in pediatric and adolescent health care. 2020 Oct 1;50(10):100884.
- Janoyer M. Blount disease. Orthopaedics & Traumatology: Surgery & Research. 2019 Feb 1;105(1):S111-21.
- Rahane P, Gijare S, Malwade M. Prevalence of Tibia Vara in School Going Obese Children in and Around Karad. Indian Journal of Public Health Research & Development. 2020 May 1;11(5).
- dos Santos Cerqueira F, Motta GA, de Faria JL, Pizzolatti IS, da Motta DP, Mandarino M, Kropf LA, dos Santos Cerqueira F. Controlled Double Gradual Opening Osteotomy for the Treatment of Severe Varus of the Knee—Blount’s Disease. Arthroscopy techniques. 2021 Sep 1;10(9):e2199-206.
- Soudy ES, Atia ME, El Alfy MN, Ali Basiony AA. Outcome of Dome-Shaped Proximal Tibial Osteotomy in Infantile Genu Varum. The Egyptian Journal of Hospital Medicine. 2021 Oct 1;85(2):3893-4897.
- Park BK, Park KB, Kwak YH, Jin S, Kim HW, Park H. A comparative evaluation of tibial metaphyseal-diaphyseal angle changes between physiologic bowing and Blount disease. Medicine. 2019 Apr;98(17).
- Vasiliadis AV, Maris A, Gadikoppula S. Tibia vara or Blount’s disease: Why an early diagnosis and treatment are important?. Clinics and Practice. 2020 Mar;10(1):15-6.
- Branum Griswold SG, Khoury J. Opening wedge osteotomy for the correction of adolescent tibia vara. The Iowa Orthopaedic Journal. 2018;38:141.
- Suwitri NP, Sidiartha IG, Dewi KA. Juvenile blount disease related to obesity In a 6-years-old girl. MEDICINA. 2018;49(2):212-6.
- Medidi RC, Rajeswari MR. A Case Report Of Blount’s Disease In Physiotherapeutic Perspective. Int J Physiother Res. 2019;7(4):3188-96.
- Di Bonito P, Valerio G, Pacifico L, Chiesa C, Invitti C, Morandi A, Licenziati MR, Manco M, Del Giudice EM, Baroni MG, Loche S. Impact of the 2017 Blood Pressure Guidelines by the American Academy of Pediatrics in overweight/obese youth. Journal of hypertension. 2019 Apr 1;37(4):732-8.
- Babio N, Becerra‐Tomás N, Nishi SK, López‐González L, Paz‐Graniel I, García‐Gavilán J, Schröder H, Martín‐Calvo N, Salas‐Salvadó J. Total dairy consumption in relation to overweight and obesity in children and adolescents: A systematic review and meta‐analysis. Obesity Reviews. 2022 Jan;23:e13400.
- Singh DR, Sunuwar DR, Dahal B, Sah RK. The association of sleep problem, dietary habits and physical activity with weight status of adolescents in Nepal. BMC Public Health. 2021 Dec;21(1):1-7.
- Maré PH, Thompson DM. Infantile Blount’s disease. SA Orthopaedic Journal. 2020 Sep;19(3):173-82.
- Lamoshi A, Chen M, Majumdar I, Harmon CM. Bariatric Surgery in Adolescents. Current Treatment Options in Pediatrics. 2020 Sep;6(3):140-54.
- Janoyer M. Blount disease. Orthopaedics & Traumatology: Surgery & Research. 2019 Feb 1;105(1):S111-21.
- AKRAM S, KHAN MA. Infantile Blount’s Disease: A case report of 3 years old female baby of Zhob, Pakistan.
- Mozafaripour E, Rajabi R, Minoonejad H. Anatomical Alignment of Lower Extremity in Subjects With Genu Valgum and Genu Varum Deformities. Physical Treatments-Specific Physical Therapy Journal. 2018 Apr 10;8(1):27-36.
- Ore V, Nasic S, Riad J. Lower extremity range of motion and alignment: A reliability and concurrent validity study of goniometric and three-dimensional motion analysis measurement. Heliyon. 2020 Aug 1;6(8):e04713.
- Mushtaq MU, Gull S, Abdullah HM, Shahid U, Shad MA, Akram J. Prevalence and socioeconomic correlates of overweight and obesity among Pakistani primary school children. BMC Public Health. 2011 Dec;11(1):1-0.
- Mozafaripour E, Seidi F, Minoonejad H, Mousavi SH, Bayattork M. Can lower extremity anatomical measures and core stability predict dynamic knee valgus in young men?. Journal of bodywork and movement therapies. 2021 Jul 1;27:358-63.
- Huang J, Tian F, Zhang Z, Shi W, Lin J, Chen L, Yang H. Reliability and concurrent validity of angle measurements in lower limb: EOS 3D goniometer versus 2D manual goniometer. Journal of orthopaedic translation. 2020 Sep 1;24:96-102.
- MOHAMED M, KAMAL AE, SHADY FM, EL-ADLY WY. Correction of Adolescent Tibia Vara by Ilizarov External Fixator. The Medical Journal of Cairo University. 2019 Jun 10;87(June):2005-11.
- Dunphy C, Casey S, Lomond A, Rutherford D. Contralateral pelvic drop during gait increases knee adduction moments of asymptomatic individuals. Human movement science. 2016 Oct 1;49:27-35.
- Wongcharoenwatana J, Kaewpornsawan K, Chotigavanichaya C, Eamsobhana P, Laoharojanaphand T, Musikachart P, Ariyawatkul T. Medial Metaphyseal Beak Angle as a Predictor for Langenskiöld Stage II of Blount’s Disease. Orthopaedic Surgery. 2020 Dec;12(6):1703-9.
- Zayer M. Tibia vara in focal fibrocartilaginous dysplasia: a report of 2 cases. Acta Orthopaedica Scandinavica. 1992 Jan 1;63(3):353-5.
- Alsancak S, Guner S, Kınık H. improved Gait parameters After orthotic treatment in children with infantile tibia Vara. Scientific Reports. 2020 Feb 21;10(1):1-7.
The Ziauddin University is on the list of I4OA, I4OC, and JISC.
This is an open- access article distributed under the terms of the Creative Commons Attribution License (CC BY 4.0).
