Adeela Asad1*, Taimoor Hassan2, Sidra Kouser3, Muhammad Ammar4, Sarah Kafeel5
1Senior Lecturer, Rawal Institute of Health Sciences, Islamabad, Pakistan![]()
2Lecturer, Isra University Islamabad, Pakistan![]()
3Student, Schellhammer Business School, Marbella University, Spain![]()
4Clinical Physiotherapist, Rand Health Rehabilitation Center, Islamabad, Pakistan![]()
5Assistant Professor, Isra University Islamabad, Pakistan![]()
ABSTRACT
Background of the study: Mechanical pain of musculoskeletal origin, known as nonspecific LBP (NSLBP), has symptoms that change depending on the type of physical activity [1]. About 85% of her LBP patients present in primary care settings are NSLBP patients.
Methodology: Randomized control trial (RCT) conducted between between January 2020 and October, 2021, Rawal General and Dental Hospital and Al-Nafees, the hospital in Islamabad. Thirty patients were included in the study. Two participants were discontinued. There were two groups of patients i.e., 15 patients in the KT group and 13 patients in the DN group diagnosed of NSCLBP by orthopedic surgeon and referral to outpatient physiotherapy clinic. The Sample size was calculated using the OpenEpi scale. The Consent form was filled out by the participants before the initiation of the study. Pain Rating Scale, Roland-Morris Disability Index Questionnaire (RMDQ) and Global patient rating scale (PGR) were assessed at baseline, two weeks post-intervention and four weeks post-treatment.
Results: Before treatment, there were no differences between the groups for PNRS, RMDQ and PGR. Both DN and KT produced significant improvements in all baseline measures (PNRS, RMDQ and PGR) after two weeks and four weeks of treatment (p<0.05). Considerable improvements were observed in all variables in both groups after treatment. However, Statistical analysis ANOVA showed no significant differences in almost all measures between groups. (p>0.05).
Conclusion: Kinesio-taping is as effective as DN in managing back pain. When treating back pain, adding DN or KT to your exercise program can make a significant contribution to your treatment.
Keywords: Dry needling, athletic tape, low back pain, disability evaluation, analogue pain scale, physical therapy specialty.
Introduction
Mechanical pain of musculoskeletal origin, known as nonspecific LBP (NSLBP), has symptoms that change depending on the type of physical activity1. About 85% of her LBP patients present in primary care settings are NSLBP patients2. Nonspecific lower back pain syndrome (NSLBP) is characterized by pain, muscle tightness, or stiffness under the rib arches and in the folds under the buttocks, with or without leg pain3,4. LBP is primarily considered a physical disability5. It is believed that 80-90% of patients with acute LBP recover completely within 6 weeks6,8. However, 10–20% of people experience chronic LBP7,9,10. 10-20% of patients with CLBP are responsible for approximately 70–80% of health and social costs7,11,15. Chronic low back pain places a significant socioeconomic burden on healthcare systems in developed nations and is a major contributor to long-term disability and absenteeism16,13,17. One of the most common reasons people go to doctor is non-specific chronic low back pain (NSCLBP), which limits activity in people under the age of 45 in developed countries17. The main objectives of conservative management of LBP are to teach patients how to manage their pain, lessen pain, and improve activities of daily living (ADLs)8 .Kinesio Tape is made to resemble the characteristics of the skin. The stretchability of the tape is intended to resemble the elasticity of the skin closely, and its thickness is comparable to that of skin. During three to five days, the tape is still remains on the skin and works. You can wear the elastic strands since the cotton fibers allow quick drying and evaporation18. When used correctly, the connective area can be used to relax weak muscles and relax overworked muscles. The application of the tape varies according to specific goals, such as improving active range of motion, relieving pain, regulating deformity, or improving lymphatic circulation18 .Kinesio taping (KT) is a conservative therapy for pain control in treating musculoskeletal disorders that has recently gained popularity. The K-Tape technique has two concepts with different tensions when applied. Light (15-25%) pulling of the attachment-to-muscle method inhibited muscle function, while mild-to-moderate (25-50%) stretching of the attachment-to-muscle attachment method inhibited muscle function, and muscle function was impaired. Attachment points, muscle function, is activated18,19. For the treatment of musculoskeletal pain, including LBP, dry needling (DN), a relatively new method used by doctors around the world, is widespread and receiving attention20,21. Direct insertion of acupuncture needles into the fascial trigger points is a minimally invasive procedure20,22. It was done to check for trigger points, either latent or active. The study team not using local anaesthesia. We selected these muscles for a variety of reasons. Active Trigger Points are a common occurrence in the gluteus medius, quadratus lumborum, and deeper multifidus, which is one of the underlying stabilizing factors but is also a significant source of pain. Patients with multifidus and erector spinae were placed face down while the gluteus medius and quadratus lumborum tests were conducted on them while they were in the lateral decubitus position. The multifidus, quadratus lumborum, and gluteus medius were positioned at a 90° angle, and the erector spinae were placed at a 45° angle. After identifying the trigger points, the skin was washed with alcohol and pierced with a needle. The injection method described by Travel and Simons for TP was used with fine 0.25–0.40 mm and 0.30–0.60 mm stainless steel needles23. Keep the needle in place for 20 minutes. After 10 minutes, rotate the needle to stimulate again. Six treatment sessions were performed twice a week. A physical therapist (SG) licensed in dry acupuncture at TP administered the antidote24.
Rationale of the Study
The present study aimed was to determine the effect of kinesio-taping vs dry needling in the treatment of chronic nonspecific low back pain (NSCLBP).
Methodology
Study Design
The Randomized clinical trial. Randomization was done by the lottery method. The Non-probability convenient sampling technique was used. The study was single-blinded (Assessor blinded).
Total Sample Size
The study included 30 participants with back pain. Two patients were discontinued. The sample was calculated by the OpenEpi tool software. The Sample size was (n1): 15 patients in the conventional group (KT group) and (n2):13 participants in the interventional group (DN group).
Duration
Between January 2020 and October 2021.
Setting
The data was collected from Rawal General and Dental Hospital and Al-Nafees Hospital in Islamabad.
Data Collection Tool
Questionnaires provide subjective ratings for patients and objective measures for clinicians. Data collection was performed using a wide range of demographics, the Roland Morris Disability Index questionnaire to measure the rate of improvement in disability after treatment, and a numerical pain rating scale to measure pain.
Data Analysis
Data were analyzed using SPSS 20. After evaluation, independent tests, repeated measures, Chi-square tests and analysis of variance (RMANOVA) were used to analyze the data. Both qualitative and quantitative variables underwent frequency and percentage analysis. Quantitative variables underwent mean and standard deviation analysis. Chi-square tests were used to investigate the connection between disability and various variables.
Inclusion Criteria
Aged 18 to 75 years had mechanical low back pain lasting >2 months, potential trigger points in the lumbar paraspinal muscles, the tight palpable band with palpable nodules in muscles indicating the reduced range of motion and pain.
Exclusion Criteria
Participants suffering from any of the contraindications to Kinesio-tape or needle phobia, Pregnancy and parturition, any psychological disorder, acute or chronic radiating LBP resulting from fracture or instability.
Data Collection Procedure
Each participant underwent a pre-intervention evaluation before being randomly assigned to either the dry needling with physiotherapy intervention group or the kinesio taping group, and outcome measurements were taken before the intervention, that is, baseline assessment. After the intervention of two weeks and the four weeks of treatment. After treatment, patients were assessed post-interventionally. For KT participants, all the inspections were performed two weeks after KT removal. Kinesio bandages and dry needling were applied as additional treatment during the procedure. In the conventional group (KT group) uses Kinesio taping and the interventional group (DN group) used dry needling with conventional physical therapy. Exercises include Stretching and strengthening your back and abdominal muscles. Over four weeks, the participant completed three sets of counselling exercises, consisting of 30-second holds and a 30-second three-fold break for each stage. A set of strength training (10 repetitions of 5 seconds rest) was performed 3 times a week for more than 4 weeks. Following a pre-intervention evaluation, each participant was randomly assigned to receive kinesio taping or dry needling as part of a physical therapy intervention. The outcomes were recorded through baseline evaluation before intervention, two weeks into intervention, and four weeks into treatment. Patients were evaluated post-intervention after receiving treatment. All assessments for the KT participant were completed two weeks after the KT was removed. Participants were divided into two groups the KT group (Conventional physical therapy treatment with kinesio taping and the DN group (conventional physical therapy treatment with dry needling were given. There was a 12-session treatment schedule that lasted for four weeks. Three sessions were held each week. For four weeks, both groups received intervention sessions three times a week. During 4 weeks, 3 recommended training sets including 30 second hold and 3 30 second rest were performed. A set of strength training (10 repetitions of 5 seconds) is performed 3 times a week for more than 4 weeks.
Results
This study comprised 28 patients. The patients were assessed pre, mid and post-treatment through the Roland-Morris questionnaire, Numeric pain rating Scale and Patient Global Rating Scale to observe the improvement after physical therapy sessions. The patients in both groups were similar in terms of the sessions they underwent and outcome measures of baseline values.
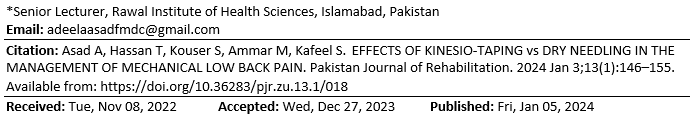
Table 1: Demographic Data
The demographic data was collected on the self-made questionnaire, which includes the data about the distribution of age, gender, height, weight and body mass index.v
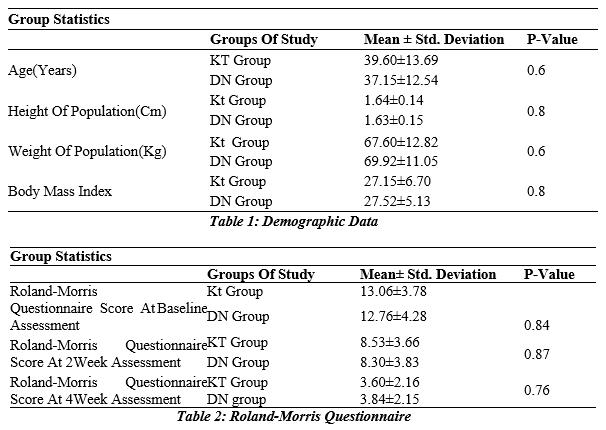
The table shows that the mean Roland-Morris questionnaire score at baseline was 13.06 ± 3.78 in the KT group compared to 12.76 ± 4.28 (p-value 0.84) in the DN group. Moreover, his mean Roland-Morris questionnaire score at 2 weeks in the KT group was 8.53 ± 3.69, whereas in the DN group it was 8.30 ± 3.83 (p-value 0.87). Similarly, at the 4-week assessment, his KT group mean was 3.60±2.16, whereas in DN group it was 3.84 ± 2.15 with (p-value 0.76). The means of the two groups did not statistically differ.
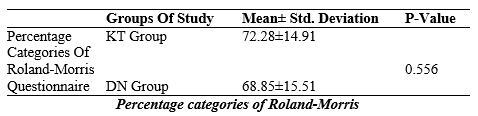
This table shows that in the KT group the mean of Percentage categories of Roland-Morris questionnaire score was 72.28 ± 14.91 whereas in DN group it was 68.85 ± 15.51. The means of the two groups did not differ statistically (p-value, 0.556).
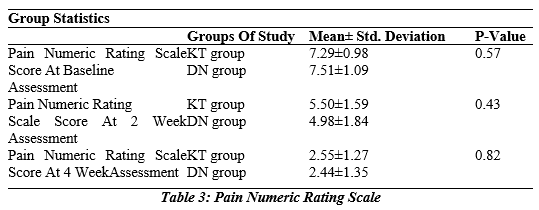
According to this table, the mean Pain Numeric Rating scale score at baseline assessment for the KT group was 7.29±0.98, while it was 7.51±1.09 for the DN group with a (p-value of 0.57). In addition, the mean Pain Numeric Rating scale score in the KT group at the 2-week assessment was 5.50±1.59 while it was 4.98±1.84 in the DN group with a (p-value of 0.43). Similar to this, the mean at 4 weeks was 2.55±1.27 for the KT group and 2.44±1.35 for the DN group with a (p-value of 0.82). The means of the two groups did not statistically differ.
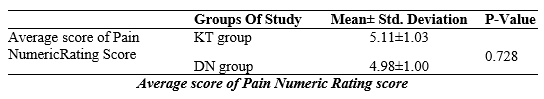
This table shows that in the KT group the mean of Average score of Pain Numeric Rating score was 5.11 ± 1.03 whereas in DN group it was 4.98 ± 1.00. The means of the two groups did not statistically differ from one another (p-value, 0.72).
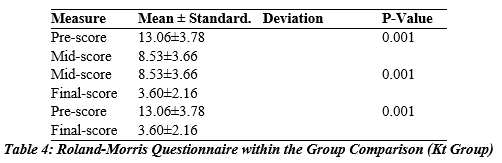
The table shows that in the KT group the mean pre-point score was 13.06 ± 3.78 compared to the midpoint score which was 8.53 ± 3.66. A statistically significant difference exits between the preliminary and average means (P < 0.001). Similarly, comparing a median of 8.53 ± 3.66 with a mean final score of 3.60 ± 2.16, there is a significant difference between mean and final scores (P < 0.001). Additionally, the comparison of mean pre-score and endpoint score was 13.06±3.78 and 3.60±2.16 respectively, between the pre-final score mean and the final score mean, there was a significant difference (P<0.001).
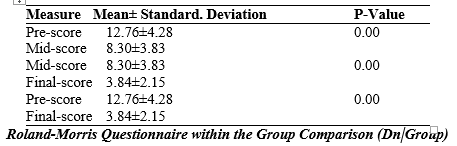
The table shows that in the DN group the mean pre-point score was 12.76 ± 4.28 compared to the midpoint score which was 8.30 ± 3.83. A statistically significant difference exits between the preliminary and average means (P < 0.001). Similarly, comparing a median of 8.30 ± 3.83 with a mean final score of 3.84 ± 2.15, there is a significant difference between mean and final scores (P < 0.001). Furthermore, the comparison of mean prescore and endpoint score was 12.76±4.28 and 3.84±2.15 respectively, a statistically significant difference between the mean of the pre- and post-test scores was discovered (P<0.001).
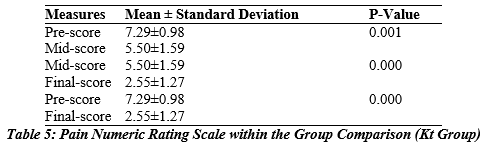
The table shows that the mean pre-point score was 7.29 ± 0.98 in the KT group compared to the midpoint score, which was 5.50 ± 1.59. A statistically significant difference exits between the preliminary and average means (P < 0.001). Similarly, comparing a mean value of 5.50 ± 1.59 with a mean final score of 2.55 ± 1.27, there is a significant difference between mean and final scores (P < 0.001). Additionally, comparison of mean pre-score and finish-points The score was 7.29±0.98 and 2.55±1.27 respectively, between the pre-final score mean and the final score mean, there was a significant difference (P<0.001).
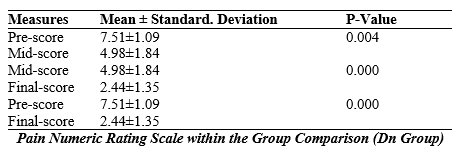
The table shows that the DN group had a mean pre-assessment of 7.51 ± 1.09 compared to a mean of 4.98 ± 1.84. A statistically significant difference exits between the preliminary and average means (P < 0.004). Similarly, comparing a mean value of 4.98 ± 1.84 with a mean final score of 2.44 ± 1.35, difference between the mean and final scores is statistically significant (P<0.001). Additionally, a significant difference between the mean pre-score and final score was discovered when comparing their respective means, which were 7.51±1.09 and 2.44±1.35, respectively (P<0.001).
Discussion
The aim of this study was to compare physical therapy exercise interventions with the kinesio taping and the dry needling in the treatment of CLBP based on changes in clinical outcomes (pain, disability).In our study, combining DN and KT with postural and stretching exercises was effective in relieving pain and reducing disability compared to baseline. There was no significant difference. Improved function may result from pain relief, and continued substantial improvement may be associated with enhanced muscle tone and elasticity after treatment. González-Iglesias et al25 observed significant improvements in pain and ROM in whiplash patients in the KT group compared to the placebo KT group. We also found that KT, like others, can positively affect pain, disability, and ROM. Using KT may have produced positive patient responses, reduced exercise anxiety, and improved ROM. This is because KT traction lifts the epidermis, relieving pressure on mechanoreceptors under the skin and reducing nociceptive stimulation. Ligament tension also provides compatibility, including pain preventive measures, thus lowering pain levels25. Recent research was conducted by Paoloni et al. We conducted a study to look at how exercise and her KT combined affected pain and ADL in a CLBP patient26. Our LBP reduction findings were in line with Paoloni et al.’s. Her pain was significantly reduced after four weeks of combined exercise therapy and KT, as determined by a pain scale. In contrast to Paoloni et al.’s study, the KT group showed a significant decline in disability as determined by the RMDQ. The shorter grades in our study (34.8 years) compared to Paoloni et al.’s study (62 years old) may cause the decrease in disability26. We came to the conclusion that the results of the Roland-Morris Disability Questionnaire were significant by contrasting our research with earlier studies. A study where the Roland-Morris Disability Questionnaire significantly decreased in both groups on day five compared to baseline (all P<0.001).We found no discernible differences between the two groups regarding pain and disability related to ADL and trunk ROM extension and flexion. Both patient groups saw similar reductions in pain and disability, even though both groups improved more. Highly recommended for those with chronic low back pain to consider DN application at TP as a crucial form of therapy. Kalichman and Vulfsons endorsed DN27. This because the treatment is affordable, simple to learn, low-risk, and minimally invasive. DNs are valid following the initial consultation. A program of 5 or 6 sessions held every two days typically allows for observing symptom development27. Analyses of pain’s nature and frequency have been conducted and reduced clinical efficacy, TPs, and TP sensitivity. The fact that there was no overlap in the confidence intervals for pain intensity, pain quality, number of TPs, or TP sensitivity supports our conclusion. This study’s pre- and post-treatment phases show that DN appears to be more successful in reducing pain and disability; there was no statistically significant difference among the post-treatment groups. The 95% confidence intervals overlap and no difference was found. In a study by Tllez-Garca et al DN and DN combined with neuroscience training were contrasted28. In their study, the authors only engaged the gluteus medius and quadratus lumborum’s active TP through DN. Although our study’s application method differs from that of other studies, the impact of DN on pain and disability was comparable. The improvement in pain with the DN application and, or the absence of pain-induced fear of exercise may be to blame for the decrease in pain and disability.
CONCLUSION
Kinesiotaping is an effective method as DN in treating mechanical back pain. During the management of Mechanical back pain, the addition of DN or KT to the exercise program can make substantial contributions to the treatment.
AUTHORS’ CONTRIBUTION:
The following authors have made substantial contributions to the manuscript as under:
Conception or Design: Adeela Asad
Acquisition, Analysis or Interpretation of Data: Adeela Asad, Sidra Kouser, Muhammad Ammar, Sarah kafeel
Manuscript Writing & Approval: Adeela Asad
All authors acknowledge their accountability for all facets of the research, ensuring that any concerns regarding the accuracy or integrity of the work are duly investigated and resolved.
ACKNOWLEDGEMENTS: None declared
INFORMED CONSENT: None declared
CONFLICT OF INTEREST: The author (s) have no conflict of interest.
FUNDING STATEMENTS: None declared
ETHICS STATEMENTS: The protocol of the present study was registered by the local ethics committee of ASRC Isra university, Islamabad approval code F.1/IUIC-IIRS/ASRC-055/2020 /registered in Clinical Trial .gov IRB NO. NCT04976582.
References
- AlBahel F, Hafez AR, Zakaria AR, Al-Ahaideb A, Buragadda S, Melam GR. Kinesio taping for the treatment of mechanical low back pain. World Appl Sci 2013;22(1):78-84.
- Casser HR, Seddigh S, Rauschmann M. Acute lumbar back pain: investigation, differential diagnosis, and Deutsches Ärzteblatt International. 2016 Apr;113(13):223.
- Manchikanti L, Singh V, Falco FJ, Benyamin RM, Hirsch JA. Epidemiology of low back pain in Neuromodulation: Technology at the Neural Interface. 2014 Oct 1;17:3-10.
- Da Silva T, Mills K, Brown BT, Herbert RD, Maher CG, Hancock Risk of recurrence of low back pain: a systematic review. journal of orthopaedic & sports physical therapy. 2017 May;47(5):305-13.
- Dunn KM, Campbell P, Jordan KP. Long-term trajectories of back pain: cohort study with 7-year follow-up. BMJ 2013 Dec 1;3(12):e003838.
- Evans R, Haas M, Schulz C, Leininger B, Hanson L, Bronfort G. Spinal manipulation and exercise for low back pain in adolescents: a randomized Pain. 2018 Jul;159(7):1297.
- Haig AJ. 3.4 Physical and rehabilitation medicine–Clinical scope: Physical and rehabilitation medicine The Journal of the International Society of Physical and Rehabilitation Medicine. 2019 Jun 1;2(5):41.
- El-Tallawy SN, Nalamasu R, Salem GI, LeQuang JA, Pergolizzi JV, Christo PJ. Management of musculoskeletal pain: An update with emphasis on chronic musculoskeletal pain. Pain and 2021 Jun;10(1):181-209.
- Oliveira CB, Maher CG, Pinto RZ, Traeger AC, Lin CW, Chenot JF, van Tulder M, Koes BW. Clinical practice guidelines for the management of non-specific low back pain in primary care: an updated European Spine Journal. 2018 Nov;27(11):2791-803.
- Pergolizzi JV, LeQuang JA. Rehabilitation for low back pain: A narrative review for managing pain and improving function in acute and chronic conditions. Pain and therapy. 2020 Jun;9(1):83-
- Balderson BH, Pruitt SD, Von Korff M. Strengthening self-management of low back pain in primary care: An evolving
- Miyamoto GC, Lin CW, Cabral CM, van Dongen JM, van Tulder MW. Cost-effectiveness of exercise therapy in the treatment of non-specific neck pain and low back pain: a systematic review with meta-analysis. British journal of sports 2019 Feb 1;53(3):172-81.
- Naik Prashant P, Anand H, Khatri Subhash M. Comparison of muscle energy technique and positional release therapy in acute low back pain–RCT. Physiotherapy and Occupational Therapy. 2010:32.
- Wu A, March L, Zheng X, Huang J, Wang X, Zhao J, Blyth FM, Smith E, Buchbinder R, Hoy D. Global low back pain prevalence and years lived with disability from 1990 to 2017: estimates from the Global Burden of Disease Study Annals of translational medicine. 2020 Mar;8(6)
- Foster NE, Anema JR, Cherkin D, Chou R, Cohen SP, Gross DP, Ferreira PH, Fritz JM, Koes BW, Peul W, Turner JA. Prevention and treatment of low back pain: evidence, challenges, and promising The Lancet. 2018 Jun 9;391(10137):2368-83.
- de Luca K, Briggs AM, French SD, Ferreira ML, Cross M, Blyth F, March L. Disability burden due to musculoskeletal conditions and low back pain in Australia: findings from GBD 2019. Chiropractic & manual 2022 Dec;30(1):1-1.
- Stanisławska I, Mincewicz M, Cabak A, Kaczor R, Czarny-Działak M, Witek B, Łyp M. Epidemiological aspects of low back pain. InAdvances in Biomedicine 2019 (pp. 47-52). Springer,
- Uzunkulaoğlu A, Aytekin MG, Ay S, Ergin The effectiveness of Kinesio taping on pain and clinical features in chronic non-specific low back pain: A randomized controlled clinical trial. Turkish journal of physical medicine and rehabilitation. 2018 Jun;64(2):126.
- Atici Y, Aydin CG, Atici A, Buyukkuscu MO, Arikan Y, Balioglu MB. The effect of Kinesio taping on back pain in patients with Lenke Type 1 adolescent idiopathic scoliosis: A randomized controlled Acta orthopaedica et traumatologica turcica. 2017 May 1;51(3):191-6.
- Hu HT, Gao H, Ma RJ, Zhao XF, Tian HF, Li L. Is dry needling effective for low back pain?: A systematic review and PRISMA-compliant meta-analysis. 2018 Jun;97(26).
- Padanilam SJ, Dayton SR, Jarema R, Boctor MJ, Tjong Dry Needling for the Treatment of Musculoskeletal Ailments With Trigger Points. Video Journal of Sports Medicine. 2021 Jul;1(5):26350254211023776.
- Dunning J, Butts R, Mourad F, Young I, Flannagan S, Perreault T. Dry needling: a literature review with implications for clinical practice guidelines. Physical therapy reviews. 2014 Aug 1;19(4):252-65.
- Simons DG, Travell J, Simons LS. Myofascial pain and dysfunction: the trigger point manual: volume 1.
- Tüzün EH, Gildir S, Angın E, Tecer BH, Dana KÖ, Malkoç M. Effectiveness of dry needling versus a classical physiotherapy program in patients with chronic low-back pain: a single-blind, randomized, controlled Journal of physical therapy science. 2017;29(9):1502-9.
- Gibbons Practical Guide to Kinesiology Taping for Injury Prevention and Common Medical Conditions. Lotus Publishing; 2020 Nov 30.
- Paoloni M, Bernetti A, Fratocchi G, Mangone M, Parrinello L, Del Pilar Cooper M, Sesto L, Di Sante L, Santilli V. Kinesio Taping applied to lumbar muscles influences clinical and electromyographic characteristics in chronic low back pain patients. Eur J Phys Rehabil 2011 Jun 1;47(2):237-44.
- Tüzün EH, Gildir S, Angın E, Tecer BH, Dana KÖ, Malkoç M. Effectiveness of dry needling versus a classical physiotherapy program in patients with chronic low-back pain: a single-blind, randomized, controlled Journal of physical therapy science. 2017;29(9):1502-9.
- Téllez-García M, de-la-Llave-Rincón AI, Salom-Moreno J, Palacios-Ceña M, Ortega-Santiago R, Fernández-de-Las-Peñas C. Neuroscience education in addition to trigger point dry needling for the management of patients with mechanical chronic low back pain: a preliminary clinical trial. Journal of bodywork and movement 2015 Jul 1;19(3).
The Ziauddin University is on the list of I4OA, I4OC, and JISC.
This is an open- access article distributed under the terms of the Creative Commons Attribution License (CC BY 4.0).
