Rabia Khan1*, Shahnila Anum2, Ghousia Shahid3, Farhan Ishaque4, Muhammad Usman5, Sobia Hassan6
1*Assistant Professor Bahria University College of Physical Therapy, Karachi, Pakistan![]()
2Consultant Physical Therapist Private Clinic Karachi, Pakistan![]()
3Assistant Professor Bahria University College of Physical Therapy, Karachi, Pakistan![]()
4Assistant Professor Dow Institute of Physical Medicine and Rehabilitation, Karachi, Pakistan![]()
5Assistant Professor Bahria University College of Physical Therapy, Karachi, Pakistan![]()
6Assistant Professor Faculty of Health Sciences Iqra University North Campus Karachi, Pakistan![]()
ABSTRACT
Background of the Study: To compare patellar taping and mobilization plus conventional therapy for reducing knee pain in patients with patellofemoral pain syndrome (PFPS).
Methodology: Controlled trial with 50 participants divided into two groups who received different treatments for 6 weeks: Group A had patellar taping and iliotibial band stretching, while Group B had patellar mobilization and quadriceps strengthening. Participants received three treatment sessions weekly for six weeks. The VAS was used to conduct pre and post-test pain evaluations for groups A and B.
Results: Knee pain decreased in PFPS patients receiving patellar taping (Group A) or mobilization (Group B) using VAS (p<0.05). All treatments are effective for PFPS. The VAS scores after 6 weeks of post A and post B treatments assessed. After 6 weeks of taping, mean = 0.76±0.83. After 6 weeks, mean and SD = 1.20±1.12 from patellar mobilization. No significant difference between means (p = 0.12, α ≤ 0.05). Insignificance.
Conclusion: The result of the study indicated that after 6 weeks of treatment for both patellar taping and patellar mobilization were effective in decreasing pain in PFPS.
Keywords: Syndrome, mobilization, taping, visual analogue scale, pain, rehabilitation.
Introduction
Patellofemoral pain syndrome is familial musculoskeletal disorder of the knee joint in an adolescents and young adult in 25% of general population globally1. It is characterized by anterolateral knee pain related to abnormalities in the patellofemoral joint2. PFPS most common between the ages of 15 and 30 among females3. Symptoms of PFPS may aggravated by some activities like running, squatting, climbing causes extra load on knee which causes excessive foot pronation a weak vastus medialis obliques (VMO)4. Females were more affected than male with patellofemoral pain syndrome which effects their activity of daily living5. Dis-alignment femoro-tibial bone, muscle weakness, overuse of the joint, patellar prior traumatic injury (fracture, dislocation) is considered as the causative factor in PFPS. Patellar taping, patellar mobilization, stretching of the lower extremity muscles are the best option for the treatment of PFPS7. The common presentation of PFPS is pain on the back of the patella which is associated with the knee positions resulting as an excessive mechanical stress on knee cap or patella8. PFPS can be treated conservatively and non-conservatively. Conservative treatment can be done through analgesics, braces or physical therapy which includes quadriceps strengthening, taping, manual mobilization and use of electro modalities for pain management9. Low association of Foot pronation present in patients of PFPS10. If foot pronation presented in PFPS patients it can be corrected through orthoses, studies showed beneficial effect of foot orthoses for excessive foot pronation in PFPS11. Knee braces were also a best choice for the correction of mal alignments of biomechanical forces on knee due to PFPS12. Biomechanical corrections in patients of PFPS can be corrected through close chain kinetic strengthening exercises13. Mobilization is considered as a best choice for any pain management, patellar mobilization had remarkable effect on pain reduction in patellofemoral syndrome through superior patellar mobilization which causes strengthening of VMO through increased knee extension14,15. Multiple types of taping protocols were existed for the treatment of PFPS, whose aim is to correct the biomechanics of lower limb. The McConnel patellofemoral joint taping technique commonly used for PFPS. Different evidence supports the beneficial effects of taping on PFPS16.Orthoses and other physical therapy interventions plays an important role in the management of PFPS17. The study was aimed to compare the efficacy of patellar taping and mobilization conjunct with conventional therapy in decreasing pain of knee joint in subject with patellofemoral pain syndrome (PFPS).
Methodology
A randomized control trial study was conducted in which diagnosed patients of patellofemoral pain syndrome were included. Total 50 participants were divided in to two groups. Participants of Group A Patellar were treated with taping technique along with iliotibial band stretching, (n=25) and Group B participants were received patellar mobilization technique with quadriceps Strengthening exercise, (n=25). Both groups were treated for 6 weeks. All Participants received three treatments sessions per week for 6 weeks totaling 18 sessions and, VAS was considered as measuring tool to check the efficacy of treatment in both groups. The pre & post- assessment of each participant of two groups were done through visual analogue scale.
Inclusion Criteria:
Male and female between the ages 25 to 35 years, Participants who had knee pain either unilaterally or bilaterally at least for past 3 months were included.
Exclusion Criteria:
Participants who had any history of fracture, traumatic pain, past surgical history and known arthritic disease were excluded from the study.
Data Analysis:
SPSS version 23.0 was used for analysis of data. Frequencies and percentages were calculated for categorical variables. The t-test was used for pre and post assessment.
Results
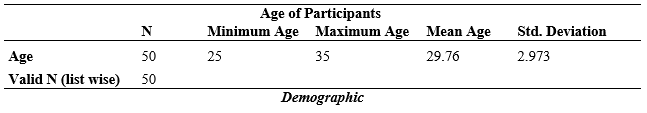
Table-1: The mean age 29.76 were reported among 50 participants where minimum age was 25 years and maximum age was 35 years.
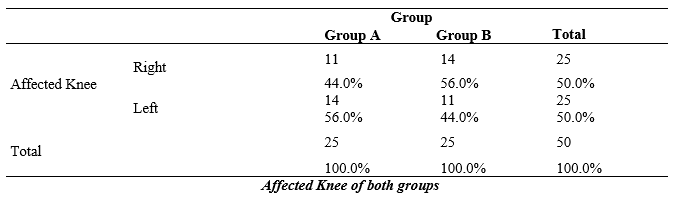
Table-2: In group A out of 25 participants 11(44.0%) were found to had right knee affected while 14(56.0%) reported on left side. Unlike group A in group B 11(44.0%) participants had left knee affected and 14(56.0%) had right affected knee.
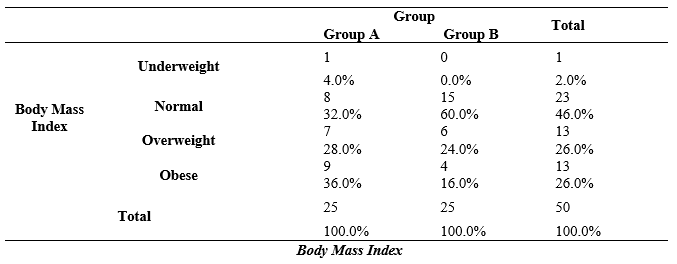
Table-3: In group A most of the participants were fall under obese category of BMI with the percentage of 36.0% (9), while in group B majority of participants were reported in normal category of BMI with the percentage of 60.0% (15).
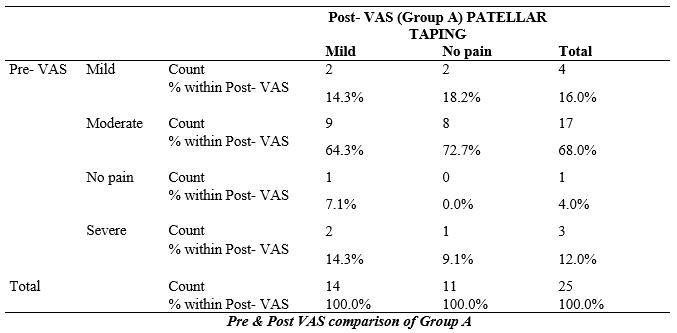
Table-4: In patellar taping group total 4 respondent were had mild pain in Pre-VAS after treatment 2 respondents reported no pain while 2 still fall in category of mild pain. Out of 25 participants 17 were had moderate pain in pre assessment which significantly reduced to categories of mild pain (9) and no pain (8) after treatment. Out of 25 respondents in group A 3 participants reported to had severe pain before treatment which in turn reduced to mild (2) and no pain (1) category of VAS in post treatment assessment.
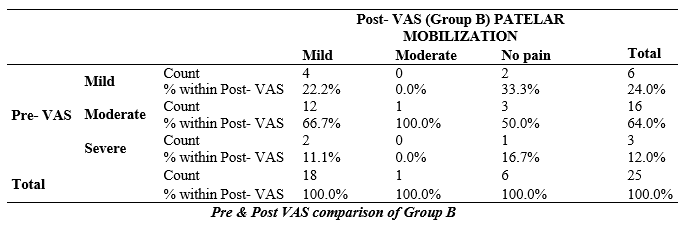
Table-5: Out of 25 participants o reported no pain, 6 reported mild pain, 16 had moderate pain and 3 claimed to have severe pain respectively in pre assessment, after treatment 6 reported no pain, 18 fall under category of mild pain, only 1 reported to had moderate pain while no respondent claimed to have severe pain.
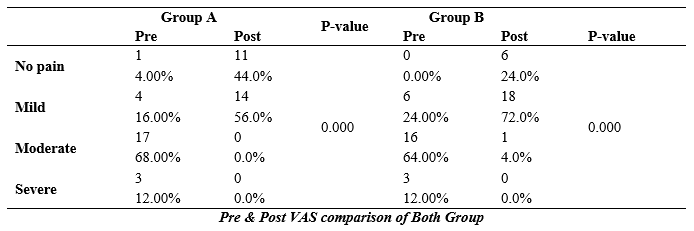
Table-6: Final results showed a statically significant reduction in pain among both groups participants through pre and post analysis of pain by VAS.
Discussions
According to this present result that there is significant improvement in pain and in patient with Patellofemoral Pain Syndrome (PFPS) at the end of 6 weeks in both groups via patellar mobilization along quadriceps strengthening exercise group A, Patellar taping with iliotibial band stretching group B. Both of the two treatment groups obtained successfully outcomes as measured by significant reduction in VAS at the two ends of two follow up. There is significant difference in intensity of pain as per VAS between two groups. In this study efforts were made to compare the effectiveness of patellar mobilization along quadriceps strengthening exercise versus patellar taping with iliotibial band stretching in the treatment of Patellofemoral Pain Syndrome (PFPS).
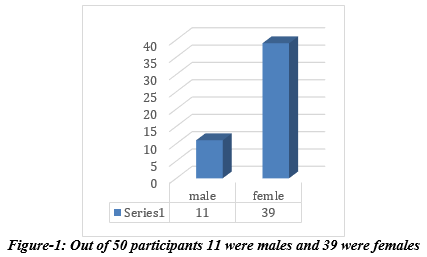
Fatimah et al18 concluded in their study that female was more affected than male, same results were found in present study. (Fiq-1).In present study it was concluded that effect of patellar mobilization in comparison to taping had no significant difference on pain unlike result was concluded in systematic review in which they concluded that reduction in pain through patellar mobilization had significant value19.Alarab A, etal20 reported a case study of 32-year-old female suffering from patellofemoral pain syndrome. Patient received a treatment of patellar mobilization along with isometric knee exercises. Results showed magnificent decrease in pain using VAS as a measuring tool. Same result was observed in present study in which mobilization technique showed significant reduction in pain. In present study it was stated that females are more likely to had patellofemoral pain in comparison to male likewise results were concluded in other studies too in which they stated that more patients of patellofemoral pain were females21,22. Benjamin, et.al reported in their meta-analysis that young adults were more effected with patellofemoral pain.in present study mean age was reported as 297. BMI had significant effect on the treatment of patellofemoral pain syndrome. Ferreira.et.al24 and Arrebola.et.al25 stated that increased BMI had significant effect on body composition which ultimately affect the treatment of patellofemoral pain. In present study it was concluded that pre and post comparison of VAS on pain in both groups had highly significant value unlike result was noted in another study in which they stated that participants who had patellar mobilization in comparison to taping had more significant value24. Systemic review was done by Logan CA etal27 in which they reviewed 5 RCTs where they concluded that taping had significant effect along with traditional exercise therapy in reduction of pain in PFPS same result was observed in present study.
Conclusion
The result of the study indicated that after 6 weeks of treatment for both patellar taping and patellar mobilization were effective in decreasing pain in PFPS.
Limitations
In present study we did not focus on the severity of patellofemoral pain which might had significant effect on treatment. Also, the sample size was limited.
AUTHORS’ CONTRIBUTION:
The following authors have made substantial contributions to the manuscript as under:
Conception or Design: Rabia Khan, Shahnila Anum
Acquisition, Analysis or Interpretation of Data: Rabia Khan, Ghousia Shahid
Manuscript Writing & Approval: Rabia Khan, Ghousia Shahid, Farhan Ishaque, Muhammad Usman, Sobia Hassan
All authors acknowledge their accountability for all facets of the research, ensuring that any concerns regarding the accuracy or integrity of the work are duly investigated and resolved.
ACKNOWLEDGEMENTS: I would like to express my sincere gratitude to all those who contributed to the completion of this article. Special thanks to my research supervisor for providing valuable guidance and support throughout the research process.
INFORMED CONSENT: All the data was collected under ethical constraints. After institutional approval from the same institute, informed consent was taken from all participants before the commencement of the study. The study followed the declaration of Helsinki.
CONFLICT OF INTEREST: There is no conflict of interest among researchers.
FUNDING STATEMENTS: No agency or foreign funding was involved. All expenses were bared by the researchers.
ETHICS STATEMENTS: The study has been approved.
References
- Mujahid Z, Afzal W, Ahmad A, Gilani SA, Akram F, Ashiq A. Prevalence of patellofemoral pain disorder or anterior knee pain in both genders ages between 18-35. Rawal Medical Journal. 2019;44(1):86-8.
- Jayasena DJ, Scalzitti DA, Palmer G, Immerman A, Courtney CA. The effects of joint mobilization on individuals with patellofemoral pain: a systematic review. Clinical rehabilitation. 2018;32(6):722-33.
- Boling M, Padua D, Marshall S, Guskiewicz K, Pyne S, Beutler A. Gender differences in the incidence and prevalence of patellofemoral pain syndrome. Scandinavian journal of medicine & science in sports 2010;20(5):725-30.
- Verschueren J, Tassignon B, De Pauw K, Proost M, Teugels A, Van Cutsem J et al. 029 Does acute fatigue negatively affect the lower extremity injury risk profile? A systematic and critical review. British Journal of Sports Medicine 2021;55(Suppl 1): A12.
- Butt A, Niazi R, Jamil A, Mehrvi N. Prevalence of patellofemoral pain syndrome in females and its impact on daily activities. Rawal Medical Journal. 2022;47(2): 385.
- Lim EH, Kim ME, Kim SH, Park KN. Effects of posterior X taping on movement quality and knee pain intensity during forward-step-down in patients with patellofemoral pain syndrome. Journal of Sports Science & Medicine 2020;19(1):224.
- Pelletier A, Sanzo P, Kivi D, Zerpa C. The effect of patellar taping on lower extremity running kinematics in individuals with patellofemoral pain syndrome. Physiotherapy theory and practice 2019;35(8): 764-72.
- Onsen LT, Koh JL. Principles of Prevention and Rehabilitation for the Patellofemoral Joint. InThe Patellofemoral Joint 2022:45-55.
- Kuwabara A, Cinque M, Ray T, Sherman SL. Treatment Options for Patellofemoral Arthritis. Current Reviews in Musculoskeletal Medicine 2022:1-7.
- Kedroff L, Holmes MN, Amis A, Newham DJ. Effect of patellofemoral pain on foot posture and walking kinematics. Gait & Posture 2019;70:361-9.
- Bonacci J, Hall M, Saunders N, Vicenzino B. Gait retraining versus foot orthoses for patellofemoral pain: a pilot randomised clinical trial. Journal of Science and Medicine in Sport 2018;21(5):457-61.
- Uboldi FM, Ferrua P, Tradati D, Zedde P, Richards J, Manunta A, Berruto M. Use of an elastomeric knee brace in patellofemoral pain syndrome: short-term results. Joints 2018;6(02): 85-9.
- Sisk D, Fredericson M. Update of risk factors, diagnosis, and management of patellofemoral pain. Current Reviews in Musculoskeletal Medicine 2019;12(4):534-41.
- Jayaseelan DJ, Scalzitti DA, Palmer G, Immerman A, Courtney CA. The effects of joint mobilization on individuals with patellofemoral pain: a systematic review. Clinical rehabilitation. 2018;32(6): 722-33.
- Alsulaimani BH. Effectiveness of patellar mobilization in patellofemoral pain syndrome. MOJ Orthop Rheumatol 2019;11(1):31-3.
- Clifford AM, Dillon S, Hartigan K, O’Leary H, Constantinou M. The effects of McConnell patellofemoral joint and tibial internal rotation limitation taping techniques in people with Patellofemoral pain syndrome. Gait & Posture. 2020;82:266-72.
- Sisk D, Fredericson M. Taping, bracing, and injection treatment for Patellofemoral pain and patellar tendinopathy. Current Reviews in Musculoskeletal Medicine 2020;13(4):537-44.
- Fatimah I, Waqqar S. Effects of tibiofemoral mobilization in patients of Patellofemoral pain syndrome. JPMA. The Journal of the Pakistan Medical Association 2021;71(11): 2506-10.
- Eckenrode BJ, Kietrys DM, Parrott JS. Effectiveness of manual therapy for pain and self-reported function in individuals with patellofemoral pain: systematic review and meta-analysis. journal of orthopaedic & sports physical therapy 2018;48(5): 358-71.
- Alarab A, Shamsiyeh BA, Abdo A, Seder A, Shameh RA, Amro A. Isometric Exercises and Mobilization Technique for Patellofemoral Syndrome: Case Report 2019. Acta Scientific Orthopaedics Volume 2019 Jul;2(7).
- Boling M, Padua D, Marshall S, Guskiewicz K, Pyne S, Beutler A. Gender differences in the incidence and prevalence of patellofemoral pain syndrome. Scandinavian journal of medicine & science in sports 2010;20(5): 725-30.
- Xu X, Yao C, Wu R, Yan W, Yao Y, Song K, Jiang Q, Shi D. Prevalence of patellofemoral pain and knee pain in the general population of Chinese young adults: a community-based questionnaire survey. BMC Musculoskeletal Disorders 2018;19(1):1-6.
- Smith BE, Selfe J, Thacker D, Hendrick P, Bateman M, Moffatt F, Rathleff MS, Smith TO, Logan P. Incidence and prevalence of patellofemoral pain: a systematic review and meta-analysis. PloS one 2018;13(1):e0190892.
- Ferreira AS, Mentiplay BF, Taborda B, Pazzinatto MF, de Azevedo FM, Silva DD. Exploring overweight and obesity beyond body mass index: A body composition analysis in people with and without patellofemoral pain. Journal of sport and health science 2021.
- Ferreira AS, Mentiplay BF, Taborda B, Pazzinatto MF, de Azevedo FM, de Oliveira Silva D. Overweight and obesity in young adults with patellofemoral pain: impact on functional capacity and strength. Journal of Sport and Health Science 2020.
- Hébert-Losier K, Hanzlíková I, Ghadikolaei SO, Janssen J, Selfe J, Richards J. An exploration of normative values in New Zealand to inform the Targeted Interventions for Patellofemoral Pain approach. Musculoskeletal Science and Practice 2021;54: 102399.
- Logan CA, Bhashyam AR, Tisosky AJ, Haber DB, Jorgensen A, Roy A, Provencher MT. Systematic review of the effect of taping techniques on patellofemoral pain syndrome. Sports Health 2017;9(5): 456-61.
The Ziauddin University is on the list of I4OA, I4OC, and JISC.
This is an open- access article distributed under the terms of the Creative Commons Attribution License (CC BY 4.0).
