Umarah Khadim1, Shumaila Zubair2, Rabia Zubair3*
1MS-SLP student, Faculty of Rehabilitation and Allied Health Sciences, Riphah International University, Lahore, Pakistan![]()
2 Deputy Director, Assessing Psychologist in Federal Public Service Commission, FPSC, Islamabad, Pakistan![]()
3*Assistant Professor, Faculty of Rehabilitation and Allied Health Sciences, Riphah International University, Lahore, Pakistan![]()
ABSTRACT
Background of the Study: The aim of the present research was to examine the assessment practices of Speech-Language Pathologists for Cognitive Communication Disorders after Traumatic Brain Injury.
Methodology: It was a cross-sectional survey method, a convenient sampling technique. Research was carried out from January 2021 to June 2021. The sample size was n=21, out of which n= 9 (42.8%) participants, each from Rawalpindi and Islamabad n= 3 (14.4%) participants from Lahore filled in their responses. Medium; being Online, the questionnaire was distributed either through email, WhatsApp or Facebook MessengerApp. SLPs who were undergraduates or who had no experience working with TBI clients were excluded. Questionnaire included 12 items. Responses of research participants were recorded using Google Forms and presented in the form of n (%). The data were analyzed using descriptive analysis, and chi-square analysis was performed to confirm the association between settings, city of practice and years of experience through Statistical Package of Social Sciences (SPSS) Version 22.0.
Results: Speech-Language Pathologists reported that they routinely assessed (62% each) Receptive and Expressive communication. However; less than half of the participants routinely evaluated domains like verbal pragmatic skills (43.3%), functional communication (33.3%) and phonemic awareness (33.3%). SLPs assessed their clients by employing tests like MoCA (55.62%), Quick Aphasia Battery (18.75%), Cognitive Assessment (LOTCA Protocol) (14.35%) and a combination of Formal (48%) and Informal (52%) clinical interviews.
Conclusion: Informal discourse assessment is incorporated more frequently as compared to informal discourse evaluation in assessment practices of Speech-Language pathologists of Pakistan for cognitive communication impairment followed by traumatic brain injury.
Keywords: Brain injuries, cognitive dysfunction, language therapy, rehabilitation, speech therapy, traumatic.
Introduction
Traumatic Brain Injury, apart from being fatal and resulting in casualties worldwide, also poses serious consequences to the survivors1. Traumatic Brain Injury’s sequel being distorted and impaired communication skills, owing to the disparities in the evaluation protocols of Speech Language Pathologists for Cognitive Communication Impairments2.Speech-Language Pathologists (SLPs) offers essential support in rehabilitating a patient after Traumatic Brain Injury (TBI). Speech-Language Pathologists perform bedside evaluation and management strategies in acute settings which specifically focuses on the management of dysphagia3. Furthermore SLP’s contribution in rehabilitating a patient with cognitive communication difficulties is paramount which involves incorporation of assessment and management procedures for cognitive communication disorders4. As rehabilitating such patients after TBI can be characterized broadly, so it also requires specialized skills for dealing with such patients. This includes the knowledge about the baseline of patient’s communication impairment and how it impedes their daily life participation5. Cognitive skills constitute processes like problem solving, memory, attention, problem solving and executive functions like setting and planning of goals, consciousness about oneself, action initiation and inhibition, monitoring and evaluation of oneself. TBI might cause cognitive-communication impairments. Cognitive-communication impairments (CCI) are the lapses and shortfalls of communication which are related to linguistic functions like Semantics, syntax, meta-linguistic skills) in addition to the non-linguistic functions (i.e. Memory, Perception, Attention)6. Another term Cognitive communication Disorders (CCD) is also employed which labels a set of communication features which includes problems with audition (hearing and listening), comprehension, speaking, writing, reading and pragmatic aspects of communication7.
TBI is a significant community health issue globally, and which has contribution in morbidity as well as mortality8. TBI results from damage to the brain/head, wherein these damages are categorized as being penetrating/piercing (for example a bullet wound) or a close head injury (for example a wound that results from a sudden rushing/braking forces in car), contingent at if the protective layers of brain/spinal cord (meninges) remain intact or otherwise. The former type of head injuries mostly causes localized lesions. The latter type of injury may cause localized abrasions or lesions, in addition to penetrated injuries to axons (like ripping and shearing of the nerves), or both of above. It is worth mentioning that the injury may happen and disturb any part of the brain, however, there are definite zones of brain which are extra susceptible to damage than the others, in the event of a closed head injury9. An estimation was made that around five hundred thousand people bear head injuries every year (200/100,000 population)10. In Pakistan major causes of TBI are reported to be road traffic accidents (38.8%) followed by falls (32.7%) and gunshots (0.15%), However 25.6% patients who reported to hospital emergency after TBI were aged between 0-10 years. The second largest group constituted of 20.1% of the patients who reported to the hospital emergency on account of TBI were between 21-30 years and the third largest group 19.5% reported to emergency after TBI was aged between 31-40 years11. Speech and Language Pathologists (SLPs) perform a vital part in rehab and restoration towards normalcy in the persons after TBI. Evaluation and mediation by the SLP embarks in the dire site with a view to emphasis principally on the management of communication impairments, scrutinize, observe and supervise the communication capabilities and loop holes during rehab regimen12. SLPs have an utmost imperative support to offer in the rehabilitation of cognitive skills, which includes but is not limited to assessment and management of CCDs13. Recuperation post-TBI is a specialized regimen which necessitates top-notch expertise and clinical decision-making skills, additionally a complete understanding of the patient’s shortfalls in communication and as to what ways this affects his quality of life14. In a recent cross-sectional survey conducted, 96% of the professionals administered cognitive assessments out of which only 9.6% administered standardized assessments and owing to the unavailability of resources the rest used informal evaluation strategies. Mini mental state examination (MMSE) was reported to be frequently employed by SLPs, while assessment protocols like Lowenstein Occupational Therapy Cognitive Assessment (LOTCA) was seldom employed, although it is of high importance for assessing cognition, as well as daily living activities15.
The current research was conducted to determine the assessment procedures and protocols of SLPs for cognitively impaired communicative disorders resulting due to traumatic brain injury in Pakistan. The study provided a baseline information of the evaluation methods of SLPs intervening with cognitive impairments. It gives foundation for the development of some culture fair test for the evaluation of cognitive communication impairment after TBI. Moreover, it will help in improving the professional efficacy of professionals who are managing cognitively impaired communicative disorders resulting due to traumatic brain injury in Pakistan.
Methodology
This was a cross-sectional survey conducted to approach SLPs working in private and government hospitals, rehabilitation centers and clinics of Rawalpindi, Islamabad and Lahore. The questionnaire was shared with n=150 participants between the time period of Jan 2021 – June 2021. Yet only n=21 participants filled in their responses out of which n=9 (42.8%) SLPs from Rawalpindi, n=9 (42.8%) SLPs from Islamabad and n=3 (14.4%) SLPs from Lahore having two or more than two years of clinical experience with cognitive impairment followed by Traumatic brain injury, recorded their responses as being the research participants. Data was collected through non-probability convenient sampling technique. The research medium being online, questionnaire was dispersed either through email, WhatsApp or Facebook messenger Ap. SLPs who were undergraduate or who had no experience working with Traumatic Brain injury clients were not included in the study.
Data Collection Tool:
Assessment procedures and protocols of SLPs administering for cognitively impaired communicative disorders resulting due to traumatic brain injury in Pakistan was assessed through a questionnaire that was adopted and comprised of 12 items16. The initial seven items were comprised of demographics of the participant’s i.e. geological placements, clinical work setting and total work experience in years. A 5-point category rating scale using fixed anchor points was incorporated to determine SLPs perception of how often they evaluated aspects of language and communication (receptive and expressive language, pragmatic skills, discourse, word finding ability, vocabulary, high level language, problem solving, reading, decoding, reading comprehension, written language and functional communication). Fixed anchor points were used as they have been recommended as more reliable and making quantitative comparisons17.
Statistical analysis:
The statistical Package for social sciences (SPSS) version 22 was used for statistical analysis. Statistical significance was set at p=0.05 and was performed on the basis of intention to treat analysis. For descriptive statistics frequency tables and bar charts were used. Chi-square analysis was performed to confirm the association between settings, city of practice and years of experience.
Results
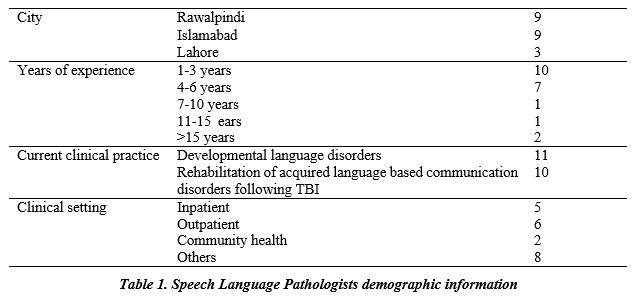
A total of n=21 responses were received from the Speech and Language Pathologists working in Rawalpindi, Lahore and Islamabad, viz, n=9 each from Rawalpindi (42.8%) and Islamabad (42.8%) and n=3 (14.4%) from Lahore. Among the respondents, n=10 (47.7%) have been practicing as Speech and Language Pathologists (SLPs) from 1-3 years, n=7 (33.3%) from 4-6 years, n=1 (4.8%) from 7-10 years, n=1 (4.8%) from 11-15 years and n=2 (9.6%) from more than 15 years. Out of 21 respondents, n=11 (52%) SLPs are currently practicing in the regimen of Language impairments due to Developmental Delays in Children, whereas n=10 (48%) of the
SLPs current clinical practice is Rehabilitation of Acquired Language-based Communication Disorders in children following a Traumatic Brain Injury (TBI). n=5 (24%) of the respondent SLPs work at the Inpatient Hospitals (acute/rehab), while n=6 (29%) of the SLPs work at the Outpatient/Community Rehabs. n=2 (9%) of the respondents work setting is Community Health and the remaining n=8 (38%) of the respondents work in ‘other’ settings like they are doing private practice, or are school based (academic), and tele-practice etc. Demographic information is listed in Table 1.
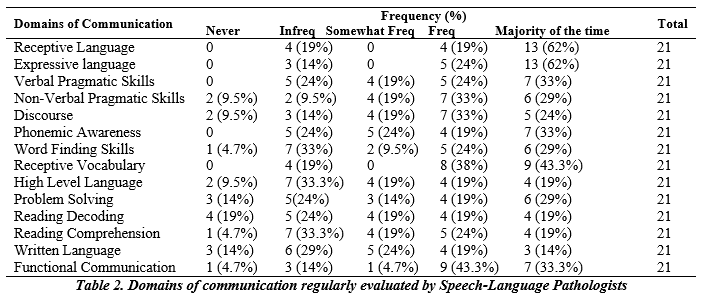
Receptive and Expressive Language areas n=13 (62% each) are reported to have been assessed Majority of the time by the SLPs. n=9 (43.3%) SLPs assess Receptive Vocabulary during majority of the time. n=7 (33.3%) SLPs assess Functional Vocabulary during majority of the time with the client. Domains of communication regularly evaluated by Speech-Language Pathologists is listed in Table 2.
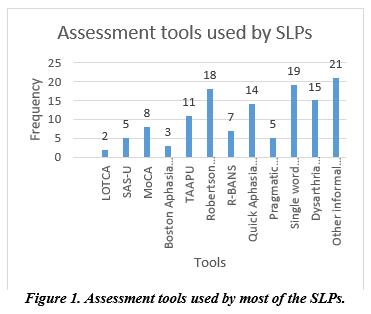
Chi-square analysis was conducted to confirm the association between clinical settings, city of practice and years of experience. It was reported that there was no significant difference between years of experience and city where SLPs practice. It was also found out that SLPs having work experience between 1-6 years’ work in both areas of developmental language disorders (n=11) and acquired communication disorder (n=10). In figure 1, participants highlight up to 4 assessments that are used which help practitioners to identify strengths and weaknesses and also that help these SLPs to formulate goals and intervention programs, multiple assessments were listed. Amongst these, Dysarthria Profile, Informal Assessments, MoCA, R-Bans, SAS-U, TAAPU, Receptive Languages, Cognitive Assessments (using LOTCA Protocol), and Quick Aphasia Battery were the most common assessments listed.
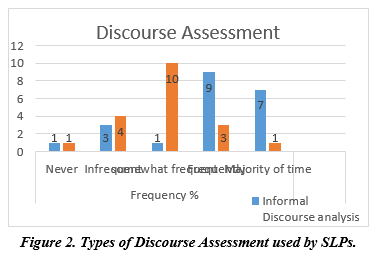
In figure 2 it is shown that n=9 (43%) of the respondent SLPs employ an Informal Discourse Analysis on frequent basis, while n=7 (33.3%) of the SLPs use this at majority of the clinical time with their clients. However, it is somewhat frequent for n=10 (48%) of the respondent SLPs to employ Formal Discourse Analysis on their clients.
Discussion
The current study results suggest that majority SLPs reported assessing Receptive and Expressive Language (62% each) among their clients to assess the communication followed by Receptive Vocabulary, Verbal Pragmatic Skills, Phonemic Awareness and Functional Communication. Domains of Communication which are reflected to be impactful to TBI, such as word finding skills, higher level language, and literacy were not regularly evaluated by the respondent SLPs. Aphasia Assessment was reported to be employed for the evaluation of communication disorders by a portion of respondent SLPs. In an International survey (n=779), 27.7% of the respondent SLPs reported to have been using Aphasia Assessment in their clinical practice18. Boston Aphasia Battery was found to have been employed by the respondent SLPs. In the more recent literature, in the United States and Australia, more and more assessments have been concentrated for CCDs after a mild TBI. Contrary to this, SLPs in the UK report to employ the Ross Information Processing Assessment and Boston Diagnostic Aphasia Battery etc19. Informal assessments like Clinical Interview has been stated to be used by the respondent SLPs (52%) in the current study. Similarly, previous researches have shown the evidence that SLPs who were probed regarding evaluation trials pertaining to Aphasia and TBI both, SLPs have been incorporating informal evaluation protocols and trials (73.5%) which were majorly based on data gathered from client and its care takers responses20. A considerable number of respondent SLPs reported to have used the Robertson Dysarthria Profile (29.3%) in their evaluations for the cognitive communicative impairments. A research reported that use of Robertson Dysarthria Profile for the assessment of the client has proven to be effective for speech improvements20. Moreover, a survey conducted in UK reports that out of 119 SLTs, 35.3% of them used Robertson Dysarthria Profile for the assessment and treatment of their clients with primary progressive Dysarthria followed by TBI21. Standardized tests like the Montreal Cognitive Assessment (MoCA) was reported to be frequently used by the respondent SLPs (55.62%) for assessment of Cognitive Communication Disorders among their clients. A study wherein 47 geriatric rehabilitation program patients participated, there was considerable correlation in comparison to the MoCA and other cognitive status tests. The sensitivity and specificity of the MoCA was found to be 80% and 30%, respectively. The attention sub-scale of the MoCA was also uniquely predictive of rehab success22. Repeatable Battery for the Assessment of Neuropsychological Status (RBANS) was also employed by a number of respondent SLPs (20.05%) for assessing the cognitive impairments of their clients. A study conducted on 112 adolescents to examine the utility of RBANS in identifying and quantifying neurocognitive impairments. The test appeared to be sensitive in detecting the neurocognitive impairments23. In a recent study conducted in Pakistan, wherein assessment practices of the SLPs were assessed, TAAPU was found to be a reliable and valid measure for Pakistani population and is linguistically appropriate24. Use of Cognitive Assessment (following LOTCA Protocol) has been reported by the SLPs (14.35%) with their clients. In a research study conducted in 2002, wherein many different approaches/tests to assess the functional outcome of stroke patients were studied. The results proved that LOTCA was a better assessment tool than the others in predicting functional status after a stroke or TBI25. Short Acculturation Scale in Urdu (SAS-U) is used by the respondent SLPs for the assessment purpose of patients with TBI in present study n=5 (23%). The scale is translated in Urdu and many other languages. It has 12 items with questions that refer to preference of language in different settings; language preferences while using media and ethnicity preferences in social relations and friends. SAS-U has been validated and translated, and is widely cited and used in research in Pakistan26. N=19 (90%) of the respondent SLPs reported that they had been employing single word naming test protocol for the assessment of communication difficulties and discourse assessment with patients followed by TBI. This is supported by evidence that confrontational naming tasks may be more sensitive to subtle language difficulties occurring after TBI27. The results also revealed that the respondents employ Informal Discourse Analysis frequently and majority of the times at the clinics. In contrast, the formal discourse Analysis is done somewhat frequently by less than fifty percent of the Speech-Language Pathologists. In an international study the use of informal language/cognitive measures were not picked up as a favored mode of evaluation by Speech-Language Pathologists in the United Kingdom and United States, Canada, where less than 3%-5% use them, respectively. However, on the contrary, SLPs near to almost 10% had stated using these evaluation procedures in the Australia/New Zealand group16. It is also supported that cognitive communication difficulties challenges on individual’s pragmatics as well as academics. Hence for managing these challenges patients with TBI should be incorporated with assessment and intervention plan of discourse impairments28. Potential limitation of this study is that multiple varieties of diversified assessment tools/practices were mentioned by respondents which includes both formal and informal methods. However, there is a need to harmonize the assessment procedures to assess and treat cognitive communication disorders. In addition, most of the evaluation tests used by Speech-Language Pathologists are not in native language, but English and thereby, may not be culturally appropriate. Self-translated and self-adapted tools by SLPs which pose a question mark at the psychometric properties of the tool as well as the assessment procedures and findings. There is a need to develop tools in native language and include domains related to assessment of memory and cognitions, which form integral part of assessment procedure in the event of traumatic brain injury.
Conclusion
Informal discourse assessment is incorporated more frequently as compared to informal discourse evaluation in evaluating strategies of SLPs of Pakistan for cognitively impaired communicative difficulties resulting due to the traumatic brain injury.
AUTHORS’ CONTRIBUTION:
The following authors have made substantial contributions to the manuscript as under:
Conception or Design: Rabia Zubair
Acquisition, Analysis or Interpretation of Data: Rabia Zubair, Umarah Khadim
Manuscript Writing & Approval: Rabia Zubair, Shumaila Zubair
All authors acknowledge their accountability for all facets of the research, ensuring that any concerns regarding the accuracy or integrity of the work are duly investigated and resolved.
ACKNOWLEDGEMENTS: None
INFORMED CONSENT: Yes.
CONFLICT OF INTEREST: The author (s) have no conflict of interest.
FUNDING STATEMENTS: None declared
ETHICS STATEMENTS: Ethical Concerns: The survey was conducted after approval from research ethical committee of Riphah International University (with ref # RIPHAH/RCRS/REC/Letter-00505).
References
- Maas AI, Menon DK, Adelson PD, Andelic N, Bell MJ, Belli A et al. Traumatic brain injury: integrated approaches to improve prevention, clinical care, and research. The Lancet Neurology. 2017;16(12):987-1048.
- Nematov SQ, Kamolova YM, Abdullayev IN. Speech therapy for adults. Science and Education. 2022;3(10):48-53.
- Short J, McCormack J, Copley A. The current practices of speech-language pathologists in providing information to clients with traumatic brain injury. International journal of speech-language pathology. 2014;16(3):219-30.
- Ackley K, Brown J. Speech-Language Pathologists’ Practices for Addressing Cognitive Deficits in College Students With Traumatic Brain Injury. American Journal of Speech-Language Pathology. 2020;29(4):2226-41.
- Maggio MG, De Luca R, Molonia F, Porcari B, Destro M, Casella C et al. Cognitive rehabilitation in patients with traumatic brain injury: A narrative review on the emerging use of virtual reality. Journal of Clinical Neuroscience. 20194;61:1-4.
- Chung CS, Pollock A, Campbell T, Durward BR, Hagen S. Cognitive rehabilitation for executive dysfunction in adults with stroke or other adult non‐progressive acquired brain damage. Cochrane Database of Systematic Reviews. 2013(4).
- Togher L. Cognitive communication disorders after traumatic brain injury. The handbook of psycholinguistic and cognitive processes: Perspectives in communication disorders. 2011:603-
- Khellaf A, Khan DZ, Helmy A. Recent advances in traumatic brain injury. Journal of neurology. 2019;266(11):2878-89.
- Iaccarino C, Carretta A, Nicolosi F, Morselli C. Epidemiology of severe traumatic brain injury. Journal of neurosurgical sciences. 2018;62(5):535-41.
- Khan A, Prince M, Brayne C, Prina AM. Lifetime prevalence and factors associated with head injury among older people in low and middle income countries: a 10/66 study. PLOS one. 2015;10(7):e0132229.
- Hardin KY, Kelly JP. The role of speech-language pathology in an interdisciplinary care model for persistent symptomatology of mild traumatic brain injury. InSeminars in Speech and Language. Thieme Medical Publishers. 2019;40(1):65-78.
- Duff MC, Proctor A, Haley K. Mild traumatic brain injury (MTBI): Assessment and treatment procedures used by speech-language pathologists (SLPs). Brain Injury. 2002;16(9):773-87.
- Beaulieu CL, Dijkers MP, Barrett RS, Horn SD, Giuffrida CG, Timpson ML et al. Occupational, physical, and speech therapy treatment activities during inpatient rehabilitation for traumatic brain injury. Archives of physical medicine and rehabilitation. 2015;96(8):S222-34.
- Franz S, Muser J, Thielhorn U, Wallesch CW, Behrens J. Inter-professional communication and interaction in the neurological rehabilitation team: a literature review. Disability and rehabilitation. 2020;42(11):1607-15.
- Imtiaz A. SIGNIFICANCE OF COGNITIVE ASSESSMENT IN RELATION TO OCCUPATIONAL THERAPY PRACTICE, AN EXPLORATORY STUDY FOR PAKISTAN OCCUPATIONAL THERAPY GUIDELINES. Pakistan Journal of Rehabilitation. 2021;10(1):17-25.
- Frith M, Togher L, Ferguson A, Levick W, Docking K. Assessment practices of speech-language pathologists for cognitive communication disorders following traumatic brain injury in adults: An international survey. Brain Injury. 2014;28(13-14):1657-66.
- Ridolfi M, Kaya A, Berkvens R, Weyn M, Joseph W, Poorter ED. Self-calibration and collaborative localization for uwb positioning systems: a survey and future research directions. ACM Computing Surveys (CSUR). 2021;54(4):1-27.
- Henry ML, Grasso SM. Assessment of individuals with primary progressive aphasia. InSeminars in speech and language,Thieme Medical Publishers. 2018;39(3): 231-41..
- Kelly M, McDonald S, Frith MH. A survey of clinicians working in brain injury rehabilitation: Are social cognition impairments on the radar?. Journal of Head Trauma Rehabilitation. 2017;32(4):E55-65.
- Bayat M, Sabeti M, Rao KS, Nami M. The clinical outcome of concurrent speech therapy and transcranial direct current stimulation in dysarthria and palilalia following traumatic brain injury: A case study. NeuroRegulation. 2020;7(3):118.
- Haas E, Ziegler W, Schölderle T. Developmental courses in childhood dysarthria: Longitudinal analyses of auditory-perceptual parameters. Journal of Speech, Language, and Hearing Research. 202;64(5):1421-35.
- Sweet L, Van Adel M, Metcalf V, Wright L, Harley A, Leiva R, Taler V. The Montreal Cognitive Assessment (MoCA) in geriatric rehabilitation: psychometric properties and association with rehabilitation outcomes. International psychogeriatrics. 2011;23(10):1582-91.
- Holzer L, Chinet L, Jaugey L, Plancherel B, Sofia C, Halfon O et al. Detection of cognitive impairment with the Repeatable Battery for the Assessment of Neuropsychological Status (RBANS) in adolescents with psychotic symptomatology. Schizophrenia Research. 2007;9
- Noveen S, Babur MN, Sabeen Z, Khatoon R. PHARMACEUTICAL SCIENCES.
- Zwecker M, Levenkrohn S, Fleisig Y, Zeilig G, Ohry A, Adunsky A. Mini-Mental State Examination, cognitive FIM instrument, and the Loewenstein Occupational Therapy Cognitive Assessment: relation to functional outcome of stroke patients. Archives of physical medicine and rehabilitation. 2002;83(3):342-5.
- Chan DN, So WK. Measuring Acculturation of Pakistani Women: A Psychometric Evaluation of Urdu Version of the Short Acculturation Scale. Asia-Pacific Journal of Oncology Nursing. 2019;6(4):349-55.
- King KA, Hough MS, Walker MM, Rastatter M, Holbert D. Mild traumatic brain injury: Effects on naming in word retrieval and discourse. Brain Injury. 2006;20(7):725-32.
- Lê K, Mozeiko J, Coelho C. Discourse analyses: Characterizing cognitive-communication disorders following TBI. The ASHA Leader. 2011;16(2):18-21.
The Ziauddin University is on the list of I4OA, I4OC, and JISC.
This is an open- access article distributed under the terms of the Creative Commons Attribution License (CC BY 4.0).
