ABSTRACT
BACKGROUND AND OBJECTIVES
Normally, aerobic exercises are considered as the therapeutic medium for improving cardiopulmonary parameters. The objective of this review is to evaluate the impact of aerobic resistance training on pulmonary parameters.
DATA SOURCES
Pubmed, Google Scholar, Science Direct, Biomed-Central (BMC), Pubmed-Europe, Medline, EMBASE and Pedro
ELIGIBILITY CRITERIA
Studies investigating role of resistive exercise training on pulmonary parameters including FVC, FEV1, VO2, TLCO etc, either alone or in combination with other exercise regimes, are included.
REVIEW METHODS
Data was extracted according to a standardized assessment form according to inclusion criteria. Risk of bias was evaluated according to the Cochrane risk of bias guidelines and qualitative analysis was performed.
RESULTS
Out of 13 selected studies, 4 studies supported the view that resistive exercises have significant role in improving the pulmonary parame-ters. There was a low risk of bias found among the studies that were selected and included in the review.
CONCLUSION
The review concludes that there is a low evidence for resistive exercises in improving the pulmonary parameters. However, more researches are needed to be conducted on the subject in future.
KEYWORDS
Resistance Exercise, Resistive training, FEV1, FVC, spirometric values, respiration, pulmonary parameters, cardiopulmonary endurance
Saima Ali
Physiotherapist
Aga Khan University Hospital
Muhammad Ather Hashmi
Lecturer
Ziauddin College of Rehabilitation Sciences
Ziauddin University
Jaza Rizvi
Lecturer
Ziauddin College of Rehabilitation Sciences
Ziauddin University
[Ali S, Hashmi MA, Rizvi J. Effect Of Resistance Training On Respiratory Parameters – A Systematic Review. Pak. j. rehabil. 2018;7(1):4-14]
Aerobic and anaerobic physical activity is evident for having curative as well as preventive effects on cardiovascular and respiratory systems by enhanc-ing respiratory parameters, aerobic strength and oxygen consumption1-3. Predominantly, aerobic exercise are opted for cardiopulmonary endurance consisting of long duration and short intensity, as recommended by American College of Sports Medicine (ACSM)4,5. Factually, the positive effects of aerobic exercise in intensifying respiratory strength, pulmonary ventilation, oxygen consump-tion, enhancing lungs volumes and capillary diame-ter; and more specifically, its role in improving respi-ratory indices like Force Vital Capacity (FVC), Force expiratory volume in one Second (FEV1) and maxi-mal voluntary ventilation (MVV); have been estab-lish by the evidence of existing literature6-10.
Anaerobic or resistance exercise, due to have focus on muscular strength and endurance too, are becoming an essential component of pulmonary rehabilitation program11,12. However, sports like basketball, water polo and rowers have been suggested to be significant in improving functions of pulmonary system and athletes involved in these sports have demonstrated statistically improved vital capacity (VC), force vital capacity (FVC) and force expiratory volumes in one minute (FEV1), com-paring to those of sedentary but healthy individu-als13. Despite of all these evidences suggest that strengthening of small and fat free muscles is proved to be beneficial for controlling dyspnea and enhancing functional capacity in patient with COPD14.
Resistance training of respiratory muscles is thought to be beneficial in improving strength as well as pulmonary parameters15. Moreover, one multidisci-plinary review identifies musculature of pelvic floor as an important contributor in respiration, which plays a crucial role in generating intra-abdominal pressure16.
Although, one study strongly recommend the potential effect of resistance training on FEV1 even if it is not consider to be the direct significance of resistance training but probably due to the improvement in lung physiology and functions as a consequence of pulmonary rehabilitation. Resis-tance training is considered to be an important treatment intervention in patient with COPD as it has a strong effect in boosting muscular strength and ultimately optimizing functional status17.
Moreover, it has been suggested in a research that effect of resistance training in lower extremity is more influential in increasing minute ventilation (VE), O2 uptake, and decreasing dyspnea as com-pared to aerobic exercise of upper and lower extremities18.
Interestingly, a research conducted among the non-active healthy males in Iran evaluated the relationship of resistance training as well as high intensity interval training exercise regimes with respi-ratory indices and inflammatory markers and concluded that the FEV1, FVC and other spiromet-ric ratios significantly increased in the experimental groups comparing to the control group that receive no exercise19.
Furthermore, a study done in 2017 on heart failure patients that significantly proved the fact that effect of combined aerobic and resistance training plus non-invasive ventilation is more influential in controlling dyspnea and quality of life than com-bined aerobic and resistance training, 6 minute walk test, FEV1 and FVC showed no improvement when compared between these two groups20.
Beside these, other regimes of exercise are also conducted to check their effects on respiratory parameters. Therefore, a research was conducted to find out the relationship between the pilates exercise and respiratory parameters in obese sedentary women21.
The current systematic review is aimed to derive a qualitative analysis of the recent available studies inquiring whether resistive exercises improve the respiratory parameters or have no effects on them.
Eligibility criteria and Information Sources
The systemic review was conducted in accordance with the guidelines provided by PRISMA (Preferred Reporting Items for Systemic Review and Meta-Analysis). An electronic search with related keywords was conducted on various databases including Cochrane, Pubmed, Google Scholar, Science Direct, Biomed-Central (BMC), Pubmed-Eu-rope, Medline, EMBASE and PEdro.
Search of Articles
Strategies acquired for literature searching include MeSH-terms and keywords using Boolean logic such as Pulmonary Function Test, Respiratory Parameters AND Resistance training, Respiratory Muscle Train-ing, EXERCISE THER. The literature search was customized for the articles published in the duration between 2013 -2018 without any specification of language. However, all full texted articles accessed, were either in English originally or English translated versions were included in the review.
Study Selection
Apparently, 46 articles were retrieved in all out of which 13 articles were selected according to the inclusion criteria. The researches investigating the effects of resistance training on respiratory parameters such as Forced Vital Capacity (FVC), Forced Expiration volume in first second (FEV1), Vital Capacity (VC), Minute ventilation (MV), Maximal Voluntary Ventilation (MVV), Maximum Oxygen consumption (VO2max), Maximum Pulmonary Inspiration (PImax), Maximum Pulmonary Expiration (PEmax) and Transfer factor for carbon monoxide (TLCO), among the healthy as well as in diseased individuals, were included without gender segrega-tion.
Study Charactersitics
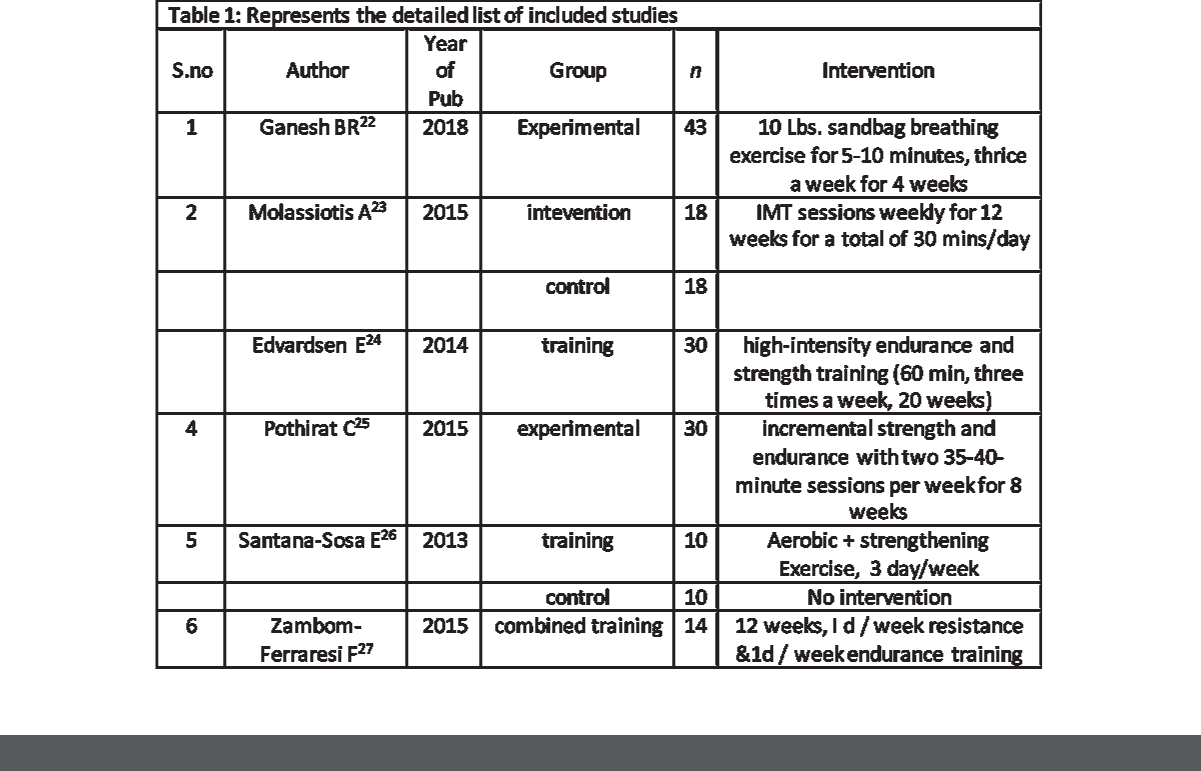
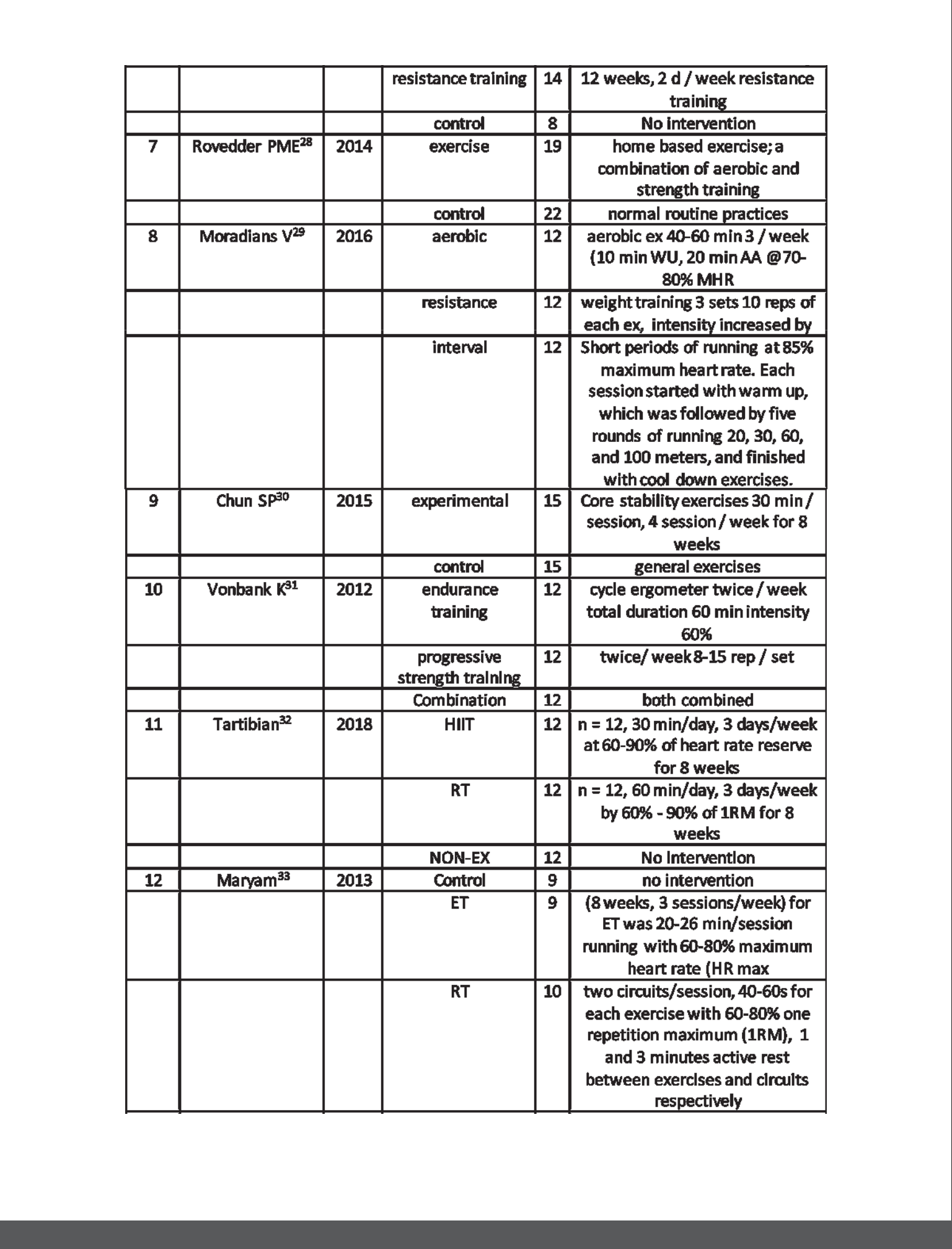
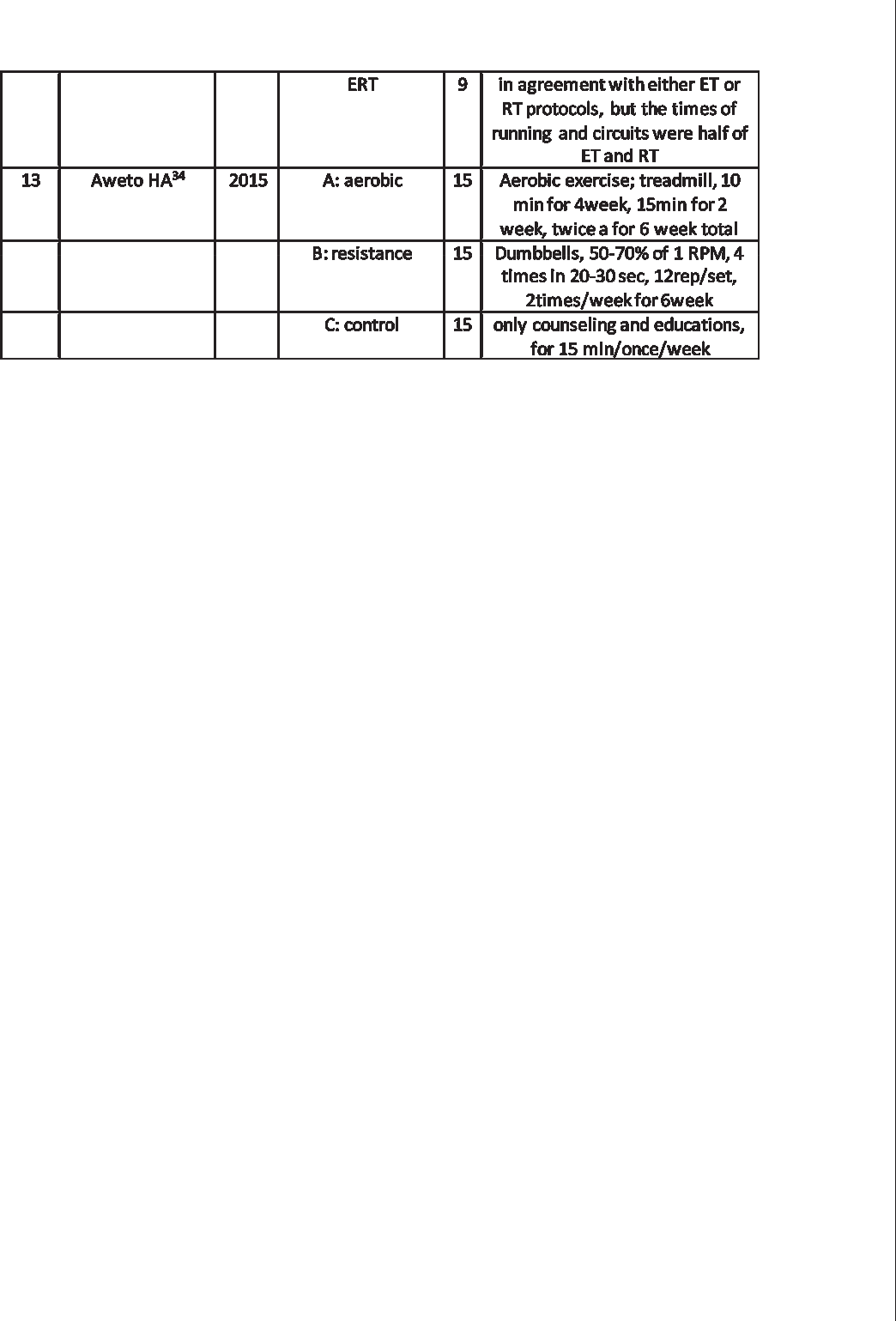
The characteristics of the researches, included in the review, include 2 quasi-experimental studies while the remaining 11 were Randomized controlled trials (RCTs). 9 of these studies independently designated an experimental group for resistive exercises as intervention while remaining 4 reported to have applied resistive exercise training in combination with other exercise regimes as demonstrated in figure 1.
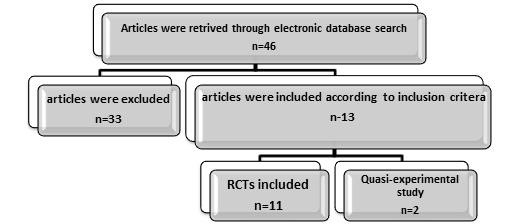
Figure: 1 Flow diagram representing study selection procedure and characteristics
Data Extraction and Management
Data was extracted and quality was assessed in accordance with inclusion and exclusion criteria considering standardized protocols. A standardized assessment form was constructed in order to main-tain validity and accuracy of data, extracted from the research articles. Furthermore, information was included as the name of the first author, year of publication, targeted population, sample size and its distribution in groups; and type of exercise regime as intervention as represented in table 1.
Selection of studies included
Originally, 46 research articles were extracted though an electronic search on various databases like Cochrane, Pubmed, Google Scholar, Science Direct, Biomed-Central (BMC), Pubmed-Europe, Medline, EMBASE and PEdro. All of these researches were published between 2013 and 2018. However, 13 studies were selected including 2 quasi-experi-mental and 11 randomized controlled trials after screening. Data was extracted and quality assess-ment was conducted in accordance with the standardized protocols. Meta-analysis and publica-tion bias evaluation could not be performed due heterogeneity in outcome measures of the studies included in the systemic review.
Synthesis of Results
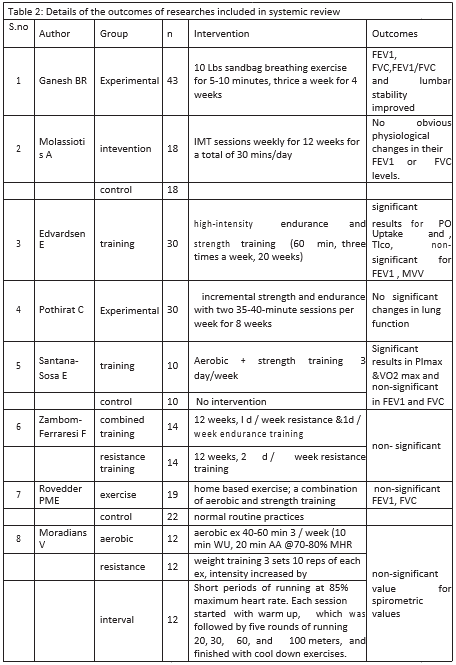
Outcome measures were assessed for each study along with the interventions applied to each study group in order to investigate the impact of resistance exercise training on respiratory parame-ters. Out of total 13 researches, included in the systematic review, 4 studies demonstrated signifi-cant impact of resistance training on respiratory parameters such as FEV1, FVC, FEV1/FVC ratio, POuptake, TLCO and MVV. However, the remaining 9 researches revealed non-significant outcomes for the intervention. Furthermore, among the 4 studies showing significant result, 2 of them indicated signifi-cant positive changes in POuptake, TLCO and VO2 only, while insignificant for FEV1, FVC, FEV1/FVC ratio. The remaining 2 studies supported the effica-cy of resistance training in improving spirometric parameters, specifically FEV1, FVC and FEV1/FVC ratio, as illustrated in table 2.
Risk of Bias and overall study quality
The risk of Bias and study quality was assessed according to standard checklist as represented in table 3 and diagrammatically in figure 2
Selection Bias
Random Sequence Generation
Random sequence generation for 11 studies (Tartib-ian, 2018, Moradians V, 2016, Molassiotis A, 2015, Zambom-Farraresi, 2015, Edvardsen, 2014, Roved-der PME, 2014, Sanatana-Sosa, 2013, Maryam, 2013, Vonbank K, 2012 and Aweto AH, 2015) demonstrat-ed low risk of bias. However, 2 studies (Ganesh BR, 2018 and Chun SP, 2015) showed unknown and only one (Pothriat C, 2015) indicated a high risk of bias.
Allocation concealment
Allocation Concealment for 11 studies (Tartibian, 2018, Moradians V, 2016, Molassiotis A, 2015, Zambom-Farraresi, 2015, Edvardsen, 2014, Roved-der PME, 2014, Sanatana-Sosa, 2013, Maryam, 2013, Vonbank K, 2012 and Aweto AH, 2015) demonstrat-ed low risk of bias. However, 2 studies (Ganesh BR, 2018 and Chun SP, 2015) showed unknown and only one (Pothriat C, 2015) indicated a high risk of bias.
Performance Bias
Blinding of participants and personnel
Blinding of participant and personnel was performed by 4 studies (Tartibian, 2018, Zambom-Farraresi, 2015, Edvardsen, 2014, Roved-der PME, 2014) and demonstrated low risk of bias. Conversely, 7 studies (Ganesh BR, 2018, Moradians V, 2016, Chun SP, 2015, Pothriat C,2015, Maryam, 2013, Vonbank K, 2012, and Aweto HA, 2015) showed unknown and 2 studies (Molassiotis A, 2015 and Sanatana-Sosa, 2013) indicated a high risk of bias.
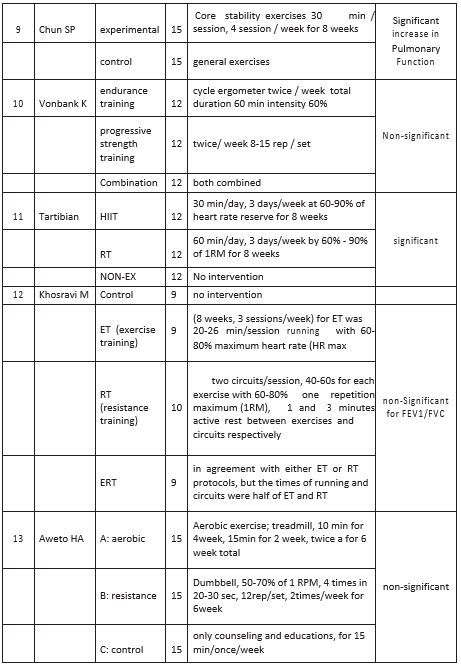
Detection Bias
Blinding of Outcome Assessment
Blinding of outcome Assessment was performed by 4 studies (Tartibian, 2018, Zambom-Farraresi, 2015, Sanatana-Sosa, 2013, performed by 4 studies (Tarti-bian, 2018, Zambom-Farraresi, 2015, Sanatana-So-sa,’ 2013, Rovedder PME, 2014) and demonstrated low risk of bias. Conversely, 7 studies (Ganesh BR, 2018, Moradians V, 2016, Chun SP, 2015, Pothriat C, 2015, Maryam, 2013, Vonbank K, 2012, and Aweto HA, 2015) showed unknown and 2 studies (Molassio-tis A, 2015 and Edvardsen, 2014) exhibited a high risk of bias.
Attrition Bias
Incomplete Outcome Data
None of the studies presented incomplete outcome data. All 13 studies (Tartibian, 2018, Zambom-Farra-resi, 2015, Sanatana-Sosa, 2013, Rovedder PME, 2014, Ganesh BR, 2018, Moradians V, 2016, Chun SP, 2015, Pothriat C, 2015, Maryam, 2013, Vonbank K, 2012, and Aweto HA, 2015, Molassiotis A, 2015 and Edvardsen, 2014) indicated low risk of bias.
Reporting Bias
Selective Reporting
Selective reporting for all 13 studies (Tartibian, 2018, Zambom-Farraresi, 2015, Sanatana-Sosa, 2013, Rovedder PME, 2014, Ganesh BR, 2018, Moradians V, 2016, Chun SP, 2015, Pothriat C, 2015, Maryam, 2013, Vonbank K, 2012, and Aweto HA, 2015, Molas-siotis A, 2015 and Edvardsen, 2014) indicated low risk of bias.
This systematic review has explored the impact of anaerobic resistance training exercise regime on various respiratory parameters including Forced Vital Capacity (FVC), Forced Expiration volume in first second (FEV1), Vital Capacity (VC), Minute ventilation (MV), Maximal Voluntary Ventilation (MVV), Maximum Oxygen consumption (VO2max), Maximum Pulmonary Inspiration (PImax), Maximum Pulmonary Expiration (PEmax) and Transfer factor for carbon monoxide (TLCO). However, meta-anal-ysis could not be performed due to the heteroge-neity of the outcome measures, interventions and targeted populations of the studies included in this systematic review.
The convergence of the findings of this systematic review revealed a low evidence of resistive exercise training regimes having a profound impact in improving respiratory parameters. Moreover, the studies demonstrating significant impact of resistance training on pulmonary system, also included those in which resistive training and aero-bic were used in combination. Probably, the heterogeneous nature of target population of different researches included in the systematic review has stipulated the differences in result outcomes, since different pulmonary parameters respond distinctly to the same intervention.
Interestingly, a recently conducted meta-analysis, concluded with the effectiveness of exercise training (i.e. the combination of aerobic and anaer-obic/ resistance exercise training) in improving the pulmonary function of individuals suffered with chronic obstructive pulmonary disease (COPD) 35. In addition to this the study also deduced that exercise training has more profound effect alone than in combination with other regimes of treat-ment interventions35. The distinctive feature of this study was the systematic characterization of outcome measures that might be the reason of clear results.
Another systematic review and meta-analysis has deduced more specifically the positive impact of resistance exercise training in COPD patients. The review postulated results inquiring 7 outcomes including 2 primary and 5 secondary outcome measures. The prominent significant enhancement was demonstrated in FEV1 with p-value of 0.04 and annulled the possibility of adversity in including resistance training in pulmonary rehabilitation regime36.
Another challenging concept has been discussed in a research study that if there is a significant differ-ence in the effects of high and low intensity upper and lower limb extension exercise considering various cardiovascular outcome measures like minute ventilation (MV), Oxygen Uptake (VO2 peak) and heart rate (HR). Subsequently, it revealed the absence of any relationship between intensity of exercise and acute cardiorespiratory changes in COPD patients. However, it does not discussed long-term effects for this intervention37. Meanwhile another study studied the impact of number and position of limbs engaged in the short bout resistive exercise on similar pulmonary param-eters including FEV1, MV, VO2peak and saturation of oxygen and concluded no significant impact of number of limbs engaged in exercise38.
Finally, the findings of systematic review conducted to investigate the effects of resistive exercise alone or in combination with aerobic regimes on respira-tory parameters, concluded that there is a low evidence for the impact of resistance exercises in improving lung function and respiratory parame-ters. However, the indication of significant results of resistive exercises in improving lung function is a suggestive of future need of further researches to be conducted on this subject.
| REFERENCES | review of available evidence. Clin Rehabil. | |||||||
| 2009;23(5):445-62. | ||||||||
| [1] | Hillsdon MM, Brunner EJ, Guralnik JM, Marmot | [15] Larson JL, Kim MJ, Sharp JT, Larson DA. Inspirato- | ||||||
| MG. Prospective study of physical activity and | ry muscle training with a pressure threshold | |||||||
| physical function in early old age. Am J of Prev | breathing device in patients with chronic | |||||||
| Med. 2005;28(3):245-50. | obstructive pulmonary disease. Am Rev Respir | |||||||
| [2] | Badaam Khaled M, Munibuddin A, Khan ST, | Dis. 1988;138(3):689-96. | ||||||
| Choudhari SP, Doiphode R. Effect of traditional | [16] Kim E, Lee H. The effects of deep abdominal | |||||||
| aerobic exercises versus sprint interval training | muscle strengthening exercises on respiratory | |||||||
| on pulmonary function tests in young sedentary | function and lumbar stability. J Phys Ther Sci. | |||||||
| males: a randomized controlled trial. JCDR. | 2013;25(6):663-5. | |||||||
| 2013;7(9):1890. | [17] O’Shea SD, Taylor NF, Paratz JD. Progressive | |||||||
| [3] | Doijad VP, Kamble P, Surdi AD. Effect of Yogic | resistance exercise improves muscle strength | ||||||
| Exercises on Aerobic Capacity (VO^ sub 2^ | and may improve elements of performance of | |||||||
| max). International Journal of Physiology. | daily activities for people with COPD: a system- | |||||||
| 2013;1(2):47. | atic review. Chest. 2009; 136(5):1269-83. | |||||||
| [4] | Saravanan S, Umesh T M, Rakesh. Aerobic | [18] Probst VS, Troosters T, Pitta F, Decramer M, Goss- | ||||||
| training for health and fitness. J Arts Cult.2011; | elink R. Cardiopulmonary stress during exercise | |||||||
| 2(1-3):65. | training in patients with COPD. Eur. Respir. J. | |||||||
| [5] | American College of Sports Medicine. Guide- | 2006; 27(6):1110-1118 | ||||||
| lines for exercise testing and prescription. 3rd | [19] Tartibian B, Khayat SM. Respiratory Indexes and | |||||||
| ed. Philadelphia: Lea and Febiger, 1988:168-169 | Inflammatory Marker Change by Different | |||||||
| [6] | Guyton and Hall. Textbook of medical physiolo- | Exercise Training. Iran J Allergy Asthma Immunol. | ||||||
| gy. Eleventh edition Noida: Published by Elsevi- | 2018; 17(2):227. | |||||||
| er; 2008:1061. | [20] Bittencourt HS, Cruz CG, David BC, Rodrigues-Jr | |||||||
| [7] | Park J, Han D. Effects of high intensity aerobic | E, Abade CM, Junior RA, Carvalho VO, dos Reis | ||||||
| exercise on treadmill on maximum-expiratory | FB, Gomes Neto M. Addition of non-invasive | |||||||
| lung capacity of elderly women. J PHYS THER | ventilatory support to combine aerobic and | |||||||
| SCI. 2017;29(8):1454-7. | resistance training improves dyspnea and quali- | |||||||
| [8] | Khashaba AS. Effect of levels of physical activity | ty of life in heart failure patients: a randomized | ||||||
| on pulmonary function of male Saudi university | controlled | trial. | Clin | Rehabil. | ||||
| students. J Sports Sci. 2015;5(5):209-12. | 2017;31(11):1508-15 | |||||||
| [9] | Azad A, Gharakhanlou R, Niknam A, Ghanbari | [21] Küçükçakır N, Altan L, Korkmaz N. Effects of | ||||||
| A. Effects of aerobic exercise on lung function in | Pilates exercises on pain, functional status and | |||||||
| overweight and obese students. Journal of | quality of life in women with postmenopausal | |||||||
| respiratory disease, thoracic surgery, intensive | osteoporosis. | J | Bodyw | Mov | Ther. | |||
| care, tuberculosis. 2011;10(3):24-31. | 2013;17(2):204-11 | |||||||
| [10] | Mottram C. Ruppel’s Manual of Pulmonary | [22] Ganesh BR, Gada Y, Dhargalkar S, Rajpurohit D. | ||||||
| Function Testing10: Ruppel’s Manual of Pulmo- | Effect Of Sandbag Breathing Exercise On Respi- | |||||||
| nary Function Testing. Elsevier Health Sciences; | ratory Parameters And Lumbar Stability In | |||||||
| 2013. | Asymptomatic Individuals-An Experimental | |||||||
| [11] | Gloeckl R, Marinov B, Pitta F. Practical recom- | Study. Int. J. Curr. Res. Med. Sci. 2018; 4(2):75-80. | ||||||
| mendations for exercise training in patients with | [23] Molassiotis | A, | Charalambous | A, Taylor P, | ||||
| COPD. Eur Respir Rev. 2013;22(128):179. | Stamataki Z, Summers Y. The effect of resistance | |||||||
| [12] | Nici L, Donner C, Wouters E, Zuwallack R, | inspiratory muscle training in the management | ||||||
| Ambrosino N, Bourbeau J, Carone M, Celli B, | of breathlessness in patients with thoracic | |||||||
| Engelen M, Fahy B, Garvey C. American thorac- | malignancies: a feasibility randomised trial. | |||||||
| ic society/European respiratory society state- | Support Care Cancer. 2015;23(6):1637-45. | |||||||
| ment on pulmonary rehabilitation. Am J Respir | [24] Edvarsen E, Skjonsberg OH, Holme I, Nordsletten | |||||||
| Crit Care Med. 2006;173(12):1390-413. | L, Borchenius F, Anderssen SA. High intensity | |||||||
| [13] | Mazic S, Lazovic B, Djelic M, Suzic-Lazic J, Djord- | training following lung cancersurgery: a | ||||||
| jevic-Saranovic S, Dumric T. Respiratory param- | randomized controlled trial. Thorax. 2014;0: 1-7. | |||||||
| eters in elite athletes – does sport have an | [25] Pothirat C, Chaiwong W, Phetsuk N. Efficacy of | |||||||
| influence? Revista Portuguesa de Pneumologia | a simple and inexpensive exercise training | |||||||
| (English Edition). 2015;21(4):192-197. | program for advanced chronic obstructive | |||||||
| [14] | Langer D, Hendriks EJ, Burtin C, Probst V, Van der | pulmonary disease patients in community | ||||||
| Schans CP, Paterson WJ, Verhoef-de Wijk MC, | hospitals. J Thorac Dis. 2015;7(4):637. | |||||||
| Straver RV, Klaassen M, Troosters T, Decramer M. | [26] Santana-Sosa E, Gonzalez-Saiz L, Groeneveld IF, | |||||||
| A clinical practice guideline for physiotherapists | Villa-Asensi JR, de Aguero Barrio MG, Fleck SJ, | |||||||
| treating patients with chronic obstructive | López-Mojares LM, Pérez M, Lucia A. Benefits of | |||||||
| pulmonary disease based on a systematic | combining | inspiratory | muscle | with | whole | |||
muscle training in children with cystic fibrosis: a randomised controlled trial. Br J sports Med. 2014;48(20):1513-1517.
- Zambom-Ferraresi F, Cebollero P, Gorostiaga EM, Hernández M, Hueto J, Cascante J, Rezusta L, Val L, Anton MM. Effects of Combined Resis-tance and Endurance Training Versus Resis-tance Training Alone on Strength, Exercise Capacity, and Quality of Life in Patients With COPD. . J Cardiopulm Rehabil Prev. 2015;35(6):446.
- Rovedder PM, Flores J, Ziegler B, Casarotto F, Jaques P, Barreto SS, Dalcin PD. Exercise programme in patients with cystic fibrosis: a randomized controlled trial. Respir Med. 2014;108(8):1134-40.
- Moradians V, Rahimi A, Moosavi SA. Effect of eight-week aerobic, resistive, and interval exercise routines on respiratory parameters in non-athlete women. Tanaffos. 2016;15(2):96.
- Kim KY, Chun SP, Kang TG, Kim GD.Effects of Core Stability Training on Postural Control Ability and Respiratory Function in Chronic Stroke Patients. Healthcare and Nursing. 2015;88(1):181-186
- Vonbank K, Strasser B, Mondrzyk J, Marzluf BA, Richter B, Losch S, Nell H, Petkov V, Haber P. Strength training increases maximum working capacity in patients with COPD–randomized clinical trial comparing three training modali-ties. Respir Med. 2012;106(4):557-63.
- Tartibian B, Khayat SMA. High-Intensity Interval Training / Resistance Exercise Lead to Greater Lung Function: Improvement of FEV1/ FVC% and FEF25-75%. Iran J Allergy Asthma Immunol. 2018;17(1):224-224Khosravi M, Tayebi SM, Safari
- Single and concurrent effects of endurance and resistance training on pulmonary function. Iran J Basic Med Sci. 2013;16(4):628
- Aweto HA, Akodu AK, Adedara AC, Olawale OA. A comparative study of the effects of aero-bic and resisted exercises on selected cardio-pulmonary parameters in patients with asthma. African Journal of Physiotherapy and Rehabili-tation Sciences. 2015;7(1-2):52-60.
- Salcedo PA, Lindheimer JB, Klein-Adams JC, Sotolongo AM, Falvo MJ. Effects of Exercise Training on Pulmonary Function in Adults with Chronic Lung Disease: a meta-analysis of Randomizes Controlled Trails. Arch Phys Med Rehabil.2018;99(12):2561-2569
- Liao W, Chen J, Chen X, Lin L, Yan H, Zhou Y et.al. Impact of Resistance training in subjects with COPD: A Systematic Review and Meta-Analysis. Respcare.2015;60(8):1130-1145
- Robles P, Araujo T, Brooks D, Zabjek K, Janau-dis-Ferrwira T, Marzolini S. et.al. Cardiorespiratory Responses to Short Bouts of Resistance Training Exercises in Individuals with Chronic Obstructive Pulmonary Disease; a Comparison of Exercise Intensities. J Cardiopulm Rehabil Prev. 2017;37(5):356-362.
- Robles P, Araujo T, Brooks D, Zabjek K, Janau-dis-Ferreira T, Marzolini S, et.al. Does limb parti-tioning and positioning affect acute cardiore-spiratory responses during strength exercises in patients with COPD? Respiro RESPIROLOGY. 2017;22(7):1336–1342.
