ABSTRACT
OBJECTIVE
To compare the effectiveness of mobilization and self-exercises in the management of adhesive capsulitis of shoulder
STUDY DESIGN
Randomized Control Trial
SAMPLE SELECTION
30 patients of adhesive capsulitis of shoulder from physiotherapy department of tertiary care hospitals of Karachi were selected through simple random sampling technique.
PROCEDURE
Treatment was continued for 5 days per week for the period of 3 weeks followed by assessment. Patients were randomly divided into two equal groups. Group A was treated with midrange mobilization while group B performed self-exercises. Both groups received TENS and hot pack prior to the exercises. Mean ± SD, frequencies and percentages were used for descriptive analysis. ROM via goniome-try and pain intensity through VAS was analyzed by paired t-test within the groups and by independent t-test between the groups, using SPSS. P-value of less than 0.05 was considered significant.
RESULTS
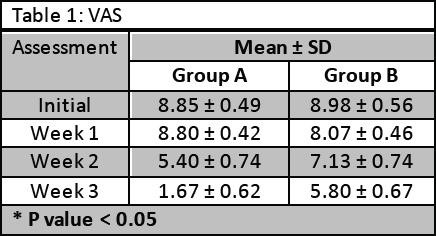
60% were females (n=18) and 40% were males (n=12) with mean age of 50.17±6.37 years. Significant improvement (p-value <0.05) in pain and shoulder ROM was observed among patients of Group A as compared to Group B. Pain intensity was decreased to 1.67 ± 0.62 in group A, whereas ROMs in these patients were also better than other group.
CONCLUSION
Joint mobilization is more effective than self-exercises in reducing pain and increasing ROM of patients of adhesive capsulitis of shoul-der.
KEYWORDS
Adhesive Capsulitis, Mobilization, Self-exercises, VAS, ROM, Frozen Shoulder
Muhammad Usman Khan
Assistant Professor
Ziauddin College of Rehabilitation Sciences
Ziauddin University
Ghazala Noor Nizami
Assistant Professor
Ziauddin College of Rehabilitation Science
Ziauddin University
Ali Farhad
Assistant Professor
Ziauddin College of Rehabilitation Sciences
Ziauddin University
[Khan MU,Nizami GN, Farhad A. Comparison of Effectiveness of Mobilization & Self-exercises in Adhesive Capsulitis of Shoulder. Pak. j. rehabil. 2018;7(1):35-41]
Adhesive capsulitis is generally recognized as Frozen Shoulder. It is one of the common musculo-skeletal problems of shoulder, causing the pain and restricted range of motion (ROM) of shoulder in all directions leading to painful stiffness of shoulder1. In 1872, Duplay identified this condition and named as Scapulo-humeral Periarthritis. Later, in 1934, the term Frozen Shoulder was used by Codman, he found that the frozen shoulder is of unknown etiology and characterized by painful and progressive restriction of movement of shoulder, with normal x-ray2. Term Adhesive capsulitis was later coined by Naviesarin 1945, describing the involvement of shoulder joint capsule. Adhesive capsulitis or Frozen Shoulder can be Primary or idiopathic in origin. Furthermore, it can be secondary due to intrinsic, extrinsic or systemic origin3.
Globally, 2-4% of the population of age between 40-65 years was suffering from adhesive capsulitis, among them 18-20% were diabetic4,5. Mostly people in sixth decade of their life get affected from adhesive capsulitis and the chances of onset before 40 years are rare. In Asian population, 15.6% patients have adhesive capsulitis and the peak age was 60–64 years6. Moreover it is more common in females than males4,5. Its incidence in females is estimated to increase by 8% for every ten years7.
It can occur in both shoulders or the other shoulder can be involved after the years of first one8. The patients suffering from long term diabetes mellitus have more chances of adhesive capsulitis. Adhe-sive capsulitis is characterized into three stages, painful stage, frozen stage and recovery stage9,10. The radiographic appearance is usually normal in adhesive capsulitis, but it shows decreased capsu-lar size on arthrography. Patients have complaints of sleep disturbance due to severe pain at night, pain associated with or without movement, limited activities of daily living and range of motion11. In early stage, frozen shoulder is usually appear similar to other problems of shoulder, like trauma, rotator cuff tear or contusion, subacromial bursitis, or even neuropathies9. Shoulder pain can lead to severe disability because of pain and stiffness. Some studies stated that almost 40% of the individuals suffered from these symptoms for about 3 years12. Frozen shoulder is usually associated with other systemic and non-systemic pathologies; the most common comorbid with an incidence of 10-36% is diabetes mellitus13. Other comorbid may be hypo-thyroidism, hyperthyroidism, stroke, pulmonary disor-ders, cardiac diseases, Parkinson’s, surgeries that can affect the ROM of shoulder joint for coronary artery bypass graft (CABG), angioplasty or angiog-raphy through hand, neurological surgery or radial neck dissection and sometimes fracture of clavicle. It is also common in patients suffering from breast and cervical cancers9.
Regimens for the treatment of adhesive capsulitis have been highlighted in researches. Over the past 3 decades, many treatment options have been debated in literatures, ranging from traditional phys-ical therapy, use of electro physical agents, non-steroidal anti-inflammatory drugs (NSAIDs), steroids, hydrotherapy, phototherapy, contrast therapy, manipulation under anesthesia and differ-ent surgical processes14-17. Rehabilitation plan com-prising of exercises, stretching, massage and use of electro-physical modalities have been shown to alleviate pain and found effective in gaining ROM in all planes. Exercises include Codman’s pendulum exercises, active and passive ROM exercises, self-as-sisted exercise by using other hand and wand, self-stretching exercise by finger ladder or wall climbing, pulley exercises, shoulder wheel exercis-es18.
Superficial and deep heating modalities are consid-ered as conventional therapies that also come under the umbrella of electro-physical agents. Literature shows that relaxation of muscles can be achieved by applying moist heating pad, and also helps in the reduction in resistance thus promote ROM19,20. Moreover, application of Transcutaneous Electrical Nerve Stimulation (TENS) also helps in stimulating the mechanoreceptors and leading to the reduction in pain20. A study conducted in 2013 by Doner et al, suggested that use of both hot pack and TENS are effective in reduction of pain and improvement of ROM of patients of adhesive capsulitis of shoulder21.
To treat the pain and stiffness of shoulder joint, passive mobilization techniques have also been used21-22. A study done in 2014, showed the improve-ment in glenohumeral joint range of motion with mobilization and active exercises, resulting in decrease in pain8. A study conducted by Johnson et al, debated regarding the posterior joint mobili-zation and anterior mobilization to improve external rotation of shoulder and found that posterior joint mobilization is more effective23. ROM measurements of flexion, abduction, and extension, medial and lateral rotations of shoulder can be performed by conventional goniometer keeping the patient lying or seated, or by using Kinect24.
Adhesive capsulitis can resolve on its own within 1-3 years or 20-50% patients suffer ROM restrictions for up to 10 years22. Many clinical trials have been conducted to compare different treatment tech-niques, including both conservative and operative methods14. Those clinical trials have different results14. A review conducted by Giovanni Maria D’Orsi et al stated that the best treatment for the adhesive capsulitis is still not confirmed14. As, there are numerous treatment approaches for the relief of adhesive capsulitis it is difficult to recognize the most beneficial and effective method. However, need of more clinical trials are needed to find the better conservative method for the management of adhesive capsulitis of shoulder. The purpose of the current study was to compare the effectiveness of mobilization and self-exercises in the manage-ment of adhesive capsulitis of shoulder.
Study Design
Experimental study design, Randomized Control Trial (RCT)
Study Setting
The study was conducted in physiotherapy depart-ment of tertiary care hospitals of Karachi, Pakistan.
Sample Size and Sampling Technique
30 patients were selected through simple random sampling technique and were divided into two groups equally.
Inclusion Criteria
Both male and female patients between age of 40 and 65 years with the diagnosis of adhesive capsuli-tis of shoulder were included in this study. These patients have limited shoulder ROM and painful stiff joint for at least 3 months22,25.
Exclusion Criteria
Patients who have been diagnosed with any condi-tion involving shoulder, such as, osteoarthritis, rheu-matoid arthritis, biceps tendonitis, calcified tendon-itis, impingement syndrome, rotator cuff tear or neuropathy were not included in the study. Patients having adhesive capsulitis of shoulder after any trauma or stroke were also not included in the study. Patients having any other severe health problem, such as, uncontrolled hypertension or uncontrolled diabetes, or injection with corticosteroids or history of surgery in the affected shoulder in the preceding 4 weeks were also excluded22, 25.
Intervention
The consent was taken from participants before the start of the study. Patients were asked about history of chief complaints, and previous medical history. Physical examination along with assessment tests of the shoulder were conducted on both sides. More-over examinations of sternoclavicular joint, acro-mioclavicular joint, scapulothoracic joint and cervi-cal spine were also performed.
The subjects were randomly distributed in Group A and B after obtaining informed consent. Initial assessment was done as soon as patient gets enrolled in the research. The treatment was then continued for 5 days a week for 3 weeks and reeval-uation was done on weekly basis for next 3 weeks. Pain intensity was measured by 10-cm visual analogue scale (VAS)7. Shoulder range of motions
(ROM) were measured by goniometer9,24. ROM measurements of abduction, flexion, internal and external rotations of shoulder were performed. For measuring abduction, the angle between the humerus and lateral chest wall was measured by Goniometer. ROM measurement of the flexion, medial rotation and lateral rotation were done when patient was kept in supine position. For medial and lateral rotation ROM measurement, the shoul-der was kept 90o abducted and elbow was flexed 90o.
Thirty patients were randomly divided into two groups. Each group consisted of 15 participants. The patients of Group A were treated with Mobiliza-tion exercises and patients of Group B were treated with Self-exercises. The frequency of the treatment session of all patients was five days a week for three weeks.
Group A: TENS and hot pack were applied prior to the mobilization exercises. TENS was applied through convention mode for 15 minutes and hot pack was also applied for 15 minutes. Mobilization exercises included mid-range rhythmic oscillations in the supine position with stabilized scapula. Inferior oscillatory glides were given to improve shoulder abduction, posterior oscillatory glides to improve flexion and internal rotation and anterior oscillatory glides to increase extension and external rotation of shoulder joint26.
Group B: Patients performed the given self-exercise program, after the application of TENS and hot pack. TENS was applied through convention mode for 15 minutes and hot pack was also applied for 15 minutes. Self-exercises include Codman’s pendu-lum exercises, self-assisted flexion exercises (self-as-sistance by other hand and wand exercises), self-stretching exercise by finger ladder or wall climbing, pulley exercises, shoulder wheel exercises. Data Collection Tool
Assessment forms were used to record data. Shoul-der ROMs were measured by goniometer and intensity of pain was assessed through 10-cm Visual Analogue Scale (VAS).
Ethical Consideration
The consent of the participants was taken before recruiting them into the study. The ethical consider-ations were taken after keeping in mind the recom-mendations of Belmont report related to human subjects. Participants were given equal opportunity to withdraw from the study without giving any reason. All the subjects recruited in the study were given full autonomy and the data recorded were kept confidential. Moreover it was in the priority to perform the trial without any prejudice and to be the best in the interest of the participants
Duration of the Study
10 months
Data Analysis Strategies
Descriptive data was analyzed by Mean, Standard Deviation (SD), frequencies and percentages. ROM and pain intensity were statistically assessed by paired t-test within the groups and by independent t-test between the groups, using SPSS. P-value of less than 0.05 was considered significant.
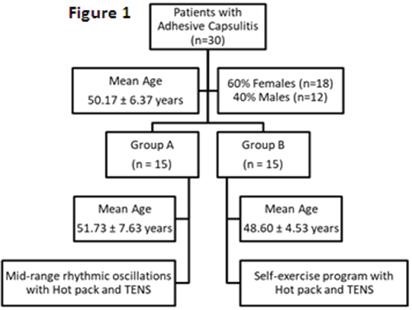
The normality of the data was identified using Kurto-sis, skewness and the Q-Q index in order to identify the nature of the test applied on the data. The result shows that the data was normally distributed and parametric test was applied to find out the level of significance among and within the groups. Among all the participants recruited in the study, 60% were females (n=18) and 40% were males (n=12), age ranging between 41 to 65 years, and the mean age was calculated as 50.17± 6.37 years. The mean age of participants of Group A was 51.73 ± 7.63 years, whereas, of Group B was 48.60 ± 4.53 years. The data was collected on a span of 3 weeks of treat-ment; initial readings of pain intensity on VAS and of ROM through goniometer were recorded and then weekly reevaluated. Summary is shown in Figure 1.
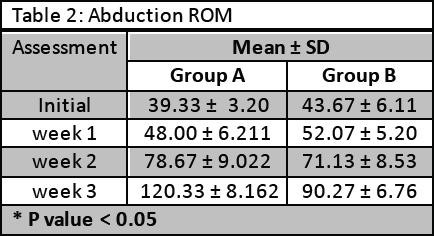
The abduction ROM was measured in degrees by goniometer and it has been found that the tech-nique applied to patients of group A was more useful and significant in improving the ROM (p < 0.05). Data was shown in Table 2.
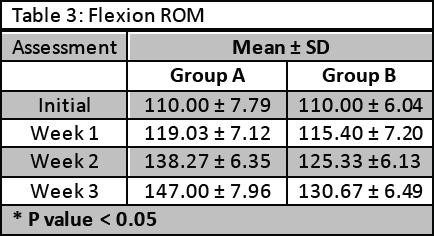
The flexion ROM was measured in degrees by goniometer and results showed that ROM was significantly improved in patients of group A (P < 0.05). Whereas, flexion ROM was also improved in patients of group B. Results are shown in Table 3.
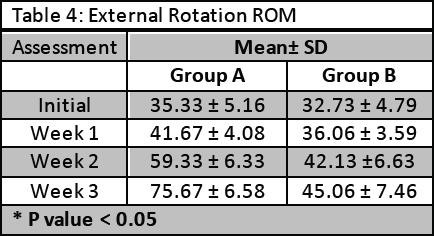
The external rotation ROM was measured in degrees by goniometer and results showed that ROM was significantly improved in patients of group A (p < 0.05). Results are shown in Table 4.
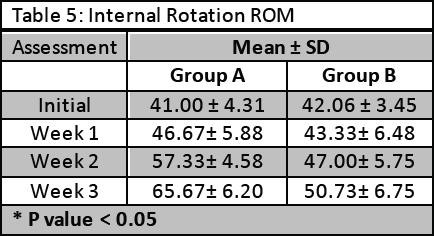
The internal rotation ROM was measured in degrees by goniometer and results showed significant improvement in group A (p < 0.05). Data was shown in Table 5.
In this study, two treatment methods were applied on patients of adhesive capsulitis. Participants of a group received mid-range rhythmic mobilization exercises, whereas, participants of another group performed self-exercises. This study found little improvement in pain scores after self-exercises that were focused on self-assistive stretching exercises including self-assisted flexion exercises with the help of other hand and wand, pulley and wheel exercis-es, and exercise by finger ladder or wall climbing. Griggs SM et al also evaluated the effects of stretch-ing exercises among the patients of adhesive capsulitis and found significant improvement in pain score27. 90% patients reported a satisfactory outcome from this treatment.
A RCT was done by Tanaka K et al and its title sounds similar to this study. It compared the effects of joint mobilization and self-exercises among patients having reduced glenohumeral joint mobili-ty28. There was a difference in the methodology of the study. This study focused in the mid-range mobi-lization, whereas, they have applied end range mobilization. Furthermore, the participants of that study were also assessed according to the frequen-cy of treatment in a week.
Younghoon Kim and Gyu Chang Lee evaluated the immediate effect of angular joint mobilization on pain, ROM, and disability in a 53 years woman having adhesive capsulitis of the shoulder29. They have given the 12 sessions for 6 weeks and found improvement in shoulder pain, ROM, and disability. Results of ours study also showed improvement in pain and ROM after mobilization.
A study done by Yang et al concluded that the group having end-range mobilization have better results that the group having mid-range mobilization along with other techniques and modalities30. Our study focused on mid-range mobilization technique in patients of one group.
A study that was conducted by Amanat et al, found that oscillatory mobilization and sustained stretch mobilization were equally effective in improving different ROM, pain and shoulder pain disability index31. Whereas, abduction was more improved through oscillatory mobilization. Our study showed that both methods of mobilization and exercises have improved the pain level and ROM of patients.
A study conducted by Doner et al compared two treatment methods. One group received hot pack, TENS and passive stretching exercises21. These passive stretching exercises included 30 seconds sustained stretch. Whereas, participants of one group of our study performed the stretching exercis-es by themselves. They used their other arm for assistance in flexion.
Chen et al conducted a study on 90 patients of shoulder pain and stiffness. One group received joint mobilization also with the advice and exercise, while other group had only advice and exercise32. Researchers concluded that addition of mobiliza-tion was not more effective than the method adopted for the other group. Their result did not match with the result of this study.
More clinical trials with different treatment combi-nations are needed to further evaluate the best management strategy for the patients of adhesive capsulitis of shoulder. The sample size of participants in each group of our study was small. Hence, it is required to conduct a study with larger sample size to identify the impact of the treatment on a broad-er aspect with greater precision.
It was concluded from the study that both the man-agement strategies, that were mobilization and self-exercise approach for shoulder pain and range of motion were found to be effective in reducing the level of pain on Visual Analog Scale and improving Functional Range of Motion after three week of interventional strategy, however the impact of mobilization along with conventional approach of physical intervention were found to be more effective in improving the outcome measures used in this study
- Nagy MT, Macfarlane RJ, Khan Y, Waseem M. The frozen shoulder: myths and realities. Open Orthop J. 2013;7:352-355
- Jadhav U, Gotecha D. Arthroscopic 360 degrees capsular release for treatment of adhesive capsulitis– A study of 40 cases. Int. j. orthop. sci. 2017;3(1):649-654
- Kelley MJ, Shaffer MA, Kuhn JE, Michener LA, Seitz AL, Uhl TL, et al. Shoulder pain and mobility deficits: adhesive capsulitis. J Orthop Sports Phys Ther. 2013;43(5):A1-31.
- Uppal HS, Evans JP, Smith C. Frozen Shoulder: A systematic review of therapeutic options. World J Orthop. 2015;6(2):263-268
- Clayton RA, Court-Brown CM. The epidemiolo-gy of musculoskeletal tendinous and ligamen-tous injuries. Injury. 2008;39(12):1338-1344
- Malavolta EA, Gracitelli MEC, Pinto GMR, da Silveira AZF, Assunção JH, Ferreira Neto AA. Asian ethnicity: a risk factor for adhesive capsu-litis? Rev Bras Ortop. Dec 2017. Available online from: www.sciencedirect.com/science/arti-cle/pii/S0102361617301510
- Struyf F, Meeus M. Current evidence on physical therapy in patients with adhesive capsulitis: what are we missing? Clin Rheumatol. 2014;33(5):593-600.
- Shivakumar HB, Chanappa TS, Balasaravanan R, Swathi KR. A comparative study between the efficacy of high grade mobiliization with active exercises versus capsular stretching with active exercises on patients with adhesive capsulitis. J Med Dent Sci. 2014;3(14):3831
- Manske RC, Prohaska D. Diagnosis and man-agement of adhesive capsulitis. Curr Rev Musculoskelet Med. 2008;1(3-4):180–189
- Dias R, Cutts S, Massoud S. Frozen shoulder. BMJ. 2005;331(7530):1453-1456.
- Frozen shoulder: what can a physical therapist do for my painful and stiff shoulder? J Orthop Sports Phys Ther. 2013;43(5):351
- Park SW, Lee HS, Kim JH. The effectiveness of intensive mobilization techniques combined with capsular distension for adhesive capsulitis of the shoulder. J Phys Ther Sci. 2014;26(11):1767-1770
- Inayat F, Ali NS, Shahid H, Younus F. Prevalence and determinants of frozen shoulder in patients with diabetes: A single center experience from Pakistan. Cureus. 2017;9(8):e1544.
- D’Orsi GM, Via AG, Frizziero A, Oliva F. Treatment of adhesive capsulitis: A review. Muscles Ligaments Tendons J. 2012;2(2):70–78.
- Musil D, Sadovský P, Stehlík J, Filip L, Vodicka Z. Arthroscopic capsular release in frozen shoulder syndrome. Acta Chir Orthop Traumatol Cech. 2009;76(2):98-103
- Hannafin JA, Chiaia TA. Adhesive capsulitis. A treatment approach. Clin Orthop Relat Res. 2000;(372):95-109.
- Neviaser AS, Hannafin JA. Adhesive capsulitis: a review of current treatment. Am J Sports Med. 2010;38(11):2346-2356
- Page MJ, Green S, Kramer S, Johnston RV, McBain B, Chau M, Buchbinder R. Manual therapy and exercise for adhesive capsulitis (frozen shoulder). Cochrane Database Syst Rev. 2014;(8):CD011275.
- Bleakley CM, Costello JT. Do thermal agents affect range of movement and mechanical properties in soft tissues? A systematic review. Arch Phys Med Rehabil. 2013;94(1):149-163.
- Page MJ, Green S, Kramer S, Johnston RV, McBain B, Buchbinder R. Electrotherapy modali-ties for adhesive capsulitis (frozen shoulder). Cochrane Database Syst Rev. 2014;(10):CD011324.
- Doner G, Guven Z, Atalay A, Celiker R. Evalution of Mulligan’s technique for adhesive capsulitis of the shoulder. J Rehabil Med. 2013 ;45(1):87-91 Vermeulen HM, Rozing PM, Obermann WR, le
- Cessie S, Vliet Vlieland TP. Comparison of high-grade and low-grade mobilization tech-niques in the management of adhesive capsuli-tis of the shoulder: randomized controlled trial. Phys Ther. 2006;86(3):355-368.
- Johnson AJ, Godges JJ, Zimmerman GJ, Ouna-nian LL. The effect of anterior versus posterior glide joint mobilization on external rotation range of motion in patients with shoulder adhe-sive capsulitis. J Orthop Sports Phys Ther. 2007;37(3):88-99
- Lee SH, Yoon C, Chung SG, Kim HC, Kwak Y, Park HW, Kim K. Measurement of shoulder range of motion in patients with adhesive capsulitis using a Kinect. PLoS One. 2015;10(6):e0129398
- Yang JL, Chang CW, Chen SY, Wang SF, Lin JJ. Mobilization techniques in subjects with frozen shoulder syndrome: randomized multiple-treat-ment trial. Phys Ther. 2007 ;87(10):1307-1315.
- Agarwal S, Raza S, Moiz JA, Anwer S, Alghadir AH. Effects of two different mobilization tech-niques on pain, range of motion and functional disability in patients with adhesive capsulitis: a comparative study. J Phys Ther Sci. 2016;28(12):3342-3349.
- Griggs SM, Ahn A, Green A. Idiopathic adhesive capsulitis. A prospective functional outcome study of non-operative treatment. J Bone Joint Surg Am. 2000;82-A(10):1398-1407.
- Tanaka K, Saura R, Takahashi N, Hiura Y, Hashimoto R. Joint mobilization versus self-exer-cises for limited glenohumeral joint mobility: randomized controlled study of management of rehabilitation. Clin Rheumatol. 2010;29(12):1439-1444.
- Kim Y, Lee G. Immediate effects of angular joint mobilization (a new concept of joint mobiliza-tion) on pain, range of motion, and disability in a patient with shoulder adhesive capsulitis: A case report. Am J Case Rep. 2017;18:148-156.
- Yang JL, Jan MH, Chang CW, Lin JJ. Effective-ness of the end-range mobilization and scapu-lar mobilization approach in a subgroup of subjects with frozen shoulder syndrome: a randomized control trial. Man Ther. 2012;17(1):47-52
- Amanat S, Sajjad AG, Kausar F, Mehmood Q, Hussain SA. Comparison of manual therapy techniques in adhesive capsulitis. JIIMC. 2017;12(4):173-176
- Chen JF, Ginn KA, Herbert RD. Passive mobilisa-tion of shoulder region joints plus advice and exercise does not reduce pain and disability more than advice and exercise alone: a randomised trial. Aust J Physiother. 2009;55(1):17-23.
