ABSTRACT
BACKGROUND AND AIM
low back pain decrease range of motion at lumber region. Manual therapy had significant effect on range of motion. Mobilization is performed in specific position of joint. The aim of this study was to compare lumber segmental mobilizations in prepositions versus prone lying in chronic low backache.
METHODOLOGY
A 6 month randomized controlled trial was conducted. We excluded 22 patients because of exclusion (neurological sign, pregnancy, spinal surgery and systemic disease) criteria we conveniently selected a sample of 40 patients between age of 25-45and having low back pain past 6 months and placed into two groups by lottery method. In group A segmental mobilization was done in preposition and in group B segmental mobilization was done in prone lying. The data collection tools were visual analog scale, Pressure Pain Threshold, Oswestry disability index and Goniometer. Data was analyzed by SPSS and statistical test were applied at 95% level of significance determine the effects of both the treatments regimes and compared with each other.
RESULTS
By comparing both groups the pre visual analog scale mean in group A and group B was7.75±0.72, 8.10±0.64 respectively (p 0.112) and post visual analog scale mean in group A and group B was 3.50±0.52, 4.90±0.72 respectively (p 0.00). The pre pressure pain threshold mean in group A and group B was 4.00±0.92,4.15±0.81 respectively (p0.59) and the post pressure pain threshold mean in group A and group B was 2.20±0.41, 2.75±0.64 respectively (p 0.00). The Pre Oswestry Low Back Pain Disability mean in group A and group B was 39.80±2.63, 39.85±2.21 respectively (p 0.95) and the Post Oswestry Low Back Pain Disability mean in group A and group B was 22.30±1.42, 29.45±1.64 respectively (p 0.00).
CONCLUSION
Segmental mobilization in pre-position has significantly better than that of in prone position in improving low backache in terms of pain, disability, pressure threshold and spinal ranges.
KEY WORDS
Lumbar Manipulation, back pain, Visual Analog Pain Scale, Range of Motion, Articular, Mechanical Low Back Pain
Faria Qasim
Consultant physiotherapist Physical therapy department
Latif hospital,Lahore.
ORCID ID: 0000-0003-2166-4351
Syed Shakeel Ur Rehman
Professor of Physical Therapy RCR&AHS
Riphah International University Lahore
ORCID ID: 0000-0002-6682-9896
Muhammad Sanaullah
Senior Lecturer RCR&AHS
Riphah International University Lahore
ORCID ID: 0000-0001-8315-4256
[Qasim F, Rehman SSU, Sanaullah M. Effects of Lumbar Segmental Mobilization in Preposition versus Prone Lying in Chronic Low Back Pain
Pak.j.rehabil. 2022; 11(1):55-61]
DOI: 10.36283/pjr.zu.11.1/008
INTRODUCTION
Low back pain (LBP) involve nerves, muscle and lumber vertebrae. The LBP is divided into acute, sub-acute and chronic on the basis of duration of pain1. If LBP is of less than 6 weeks duration than it is acute type, if LBP is 6-12 weeks duration than it is sub-acute type and chronic LBP is of 12 weeks or more duration2.
The low back pain percentage changes in age groups. Overall percentage is 17-30% worldwide. In Pakistan the low back pain percentage is 12-33%3,4.
There are many classification models for LBP like status index, patient’s response model, prognostic index model. There are many pain generators at lower back such as joints, ligaments, muscles, dura mater, gray rami, bones and thorac-o-lumber fascia 5.
The McCarthy and colleagues introduce three diagnostic categories. 1st diagnostic categories is identification of problems with nerve root involvements, 2nd is identification of problems with serious pathology, 3rd is identification of cases with non-specific LBP6.
Treatment for LBP is either non-surgical or surgical. Non-surgical treatment included physiotherapy and drugs. Surgical treatment included laminectomy, nerve block etc. in physiotherapy modalities, mobilization, manipulation and exercises are used to treat low back pain7.
The symptomatic effects of mobilization is biomechanical and neurophysiological8. The most adopted mechanism for decreasing pain by mobilization is pain modulating center in brain is activated and that center contain descending periaqueductal grey (dPAG)9. In posterior anterior (PA) mobilization sympathy-o-excitatory response increase which lead to hypoalgesia. Moreover, in unilateral lumber mobilization peripheral sympathetic nervous system changes detected in skin conduction study 10, 11.
The use of passive procedures to enhance the movement in a specific direction is plausible if this movement positively influences the concordant sign of the patient12. For instance, with the exclusion of an isolated L5–S1dysfunction, if a patient benefits from repeated end range exercises of extension the patient may benefit from repeated passive accessory type of mobilization to the spine at a preposition end-range extension because both the actions create a similar 3 point movement of the spine later, prepositions that target the movements of side flexion and extension, or nerve tension may be helpful prior to apply unilateral posteroanterior or central posteroanterior method. Each technique is only applied if the effects of the technique are similar to what happens during the specific concordant active physiological type of movement13.
Segmental mobilization in pre-position had more significant effects. A study was conducted on 134 patients to determine effects of traction on lumber pain in modified preposition. The results showed that pain improved in 52.1% patients by traction in modified pre-position while 8.1% patient showed improvement in conventional position. This study supports the mobilization or traction in pre-position had better results14.
There was no research conducted on mobilization in preposition so in this study lumbar segmental mobilization in preposition was compared with prone lying in chronic low back pain.
METHODS
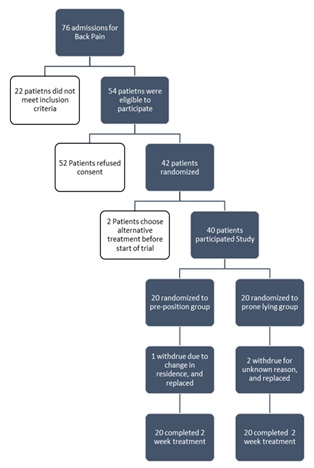
A 6 month randomized controlled trial was conducted at department of physiotherapy General hospital, Lahore and THQ, Kot momin Punjab Pakistan. Out of 76 admissions for back pain 54 patients were eligible to participate. 12 patients refused consent, from remaining 42 patients 2 chose alternative treatment. 40 patients participated in study by Non probability convenient sapling techniques and were placed in two groups by Lottery method and accessor was blind. In group A segmental mobilization was done in preposition. For preposition patient will be placed on side lying with lower leg straight and upper leg side flex. Therapist will pull patient upper arm which is at lower side to rotate the spine up to pain free range. Therapist thigh will be close to patient pelvic and forearm will be at patient rib cage. With other hand therapist apply mobilization. In group B segmental mobilization was done in prone lying. The data collection tools were visual analog scale (VAS) is a 10cm straight line 0 mean no pain and 10 mean unbearable pain15. Pressure Pain Threshold (PPT) is 0-6 scale assessor applying specific amount of pressure. The 0 relates very high irritable pain and 6 refers to high threshold with no provocation16. Oswestry disability index (ODI) is a 10 question scale with 50 maximum point, higher the score mean disability increased 17 and Goniometer for range of motion (ROM)18. Data was analyzed by SPSS and statistical test were applied at 95% level of significance determine the efficacy of both the treatments regimes. Independent t test was used to compare groups as data was normally distributed in shapiro wilk test.
All 40 patients were treated for 2 weeks at 4 days per week, for single session 45 minutes. In Group A the patients were first treated with hot pack,19physiological rotation & TENS,20 for 10 minutes and then segmental mobilization were done in preposition at 6-8 glides per session from T12 to L5. In Group B the patients were first treated with hot pack, physiological rotation & TENS for 10 minutes and then segmental mobilization was done in prone lying at 6-8 central poster-o-anterior or unilateral poster-o-anterior glides per session from T12 to L5. Patients were treated for 2 weeks and data was collected before start of 1st session (pre) and end of last session (post).
ETHICAL CONCERNS
Ethical review committee Riphah International University Lahore approve research with Ref NO. RCR&AHS/REC/MS-OMPT/023. The consent was taken from patients before treatment on Urdu and English consent form.
RESULTS
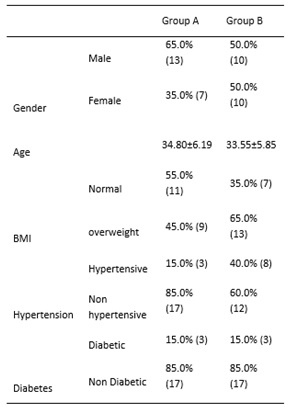
The baseline characteristics of all 40 participants were documented in table I. The normal BMI in group A was 55.0% and in group B was 35%. The hypertensive patients in group A were 15% and in group B were 40%. The diabetic patients in group A were 15% and group B were 15%.
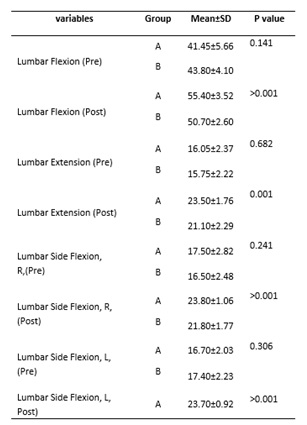
In table II The mean difference for VAS in group A was 4.25±0.21 and in group B was 3.20±0.08. The mean difference for pressure pain threshold in group A was 1.8±0.51 and in group B was 1.4±0.17. The mean difference for joint play gliding in group A was 1.75±0.1 and in group B was 1.15±0.27. The mean difference for ODI in group A was 17.5±1.21 and in group B was 10.4±0.57. Table I: Base line characteristics of all 40 patients of chronic low back pain. Table III: ROM changes at two weeks of all 40 patients of chronic low back pain.
In table III the mean difference for lumber flexion in group A was 13.95±2.14 and in group B was 6.9±1.5. The mean difference for lumber extension in group A was 7.45±0.61 and in group B was 5.35±.07. The mean difference for right flexion in group A was 6.3±1.7t and in group B was 5.3±0.71. The mean difference for left flexion in group A was 7±1.11 and in group B was 4.1±0.14.
DISCUSSION
This study showed that mobilization in preposition had significant effect (p<0.01) than mobilization in prone lying on Visual analog scale (VAS), oswestry disability index (ODI) pressure pain threshold (PPT) and lumber range of motion.
Mobilization in preposition is less researched. This study provide evidence that segmental mobilization in preposition of lumber region can give effective results.
Dickey said that in physiological motion there is strong association between accessory vertebral movement and pain. They said that distraction and compression intervertebral movements had strong association with pain. The vertebral mobilization cause compression and distraction at vertebral joint and in this study there was improvement of pain by either in preposition or in prone position but there was greater effect (1 point) in preposition than in prone position21.
Table II: changes in pain, pressure pain threshold and physical disabilities at two weeks of all 40 patients of chronic low back pain.
A study added core-stability exercises with lumber segmental mobilization for low back pain. The assessment tools were ODI and VAS. The mean difference for VAS was 5 and for ODI was 20. In this study mobilization also had effect on pain and disability in LBP. This study assessment tools were ODI, VAS, PPT and goniometry. The mean difference for VAS in group treated with mobilization in preposition was 4.20±0.21 for ODI was 17.5±1.2122.
Saira et al compare McKenzie treatment with Mulligan SNAG,s in prone position for low back pain. Mean difference in VAS for mulligan group was 6.20±2.22 and for McKenzie group was 7.39±1.35. The mean difference in ODI for mulligan group was 66.7±2.35 and for McKenzie group was 67.58±2.08. The mean difference in lumber extension for mulligan group was 27.99±2.34 and for McKenzie group was 32.25±3.04. In this study PPT assessment tools was also added. Mobilization in both position had significant effects but in preposition there was more improvement as mean difference for pain was 4.20±0.21, for disability was 17.5±1.21 and for lumber extension was 7.45±0.61.23.
Ain SQ et al study mulligan mobilization effects on low back pain. Assessment tools were ODI, NPRS and goniometer. There was improvement in lumber flexion 9.75±0.45, lumber extension 7.15±0.78, lumber left side flexion 6.45±0.73, pain 4.30±0.04and ODI16.4±1.3. In this study PPT was also used as assessment tool. The improvement in pain and disability was almost same but range of motion was more improve with mobilization in preposition as compare to mulligan mobilization24.
Creighton DS et al study cervical traction mobilization in preposition in painful cervical range of motion. The mean difference for cervical left rotation was 7.78 and for cervical right rotation was 7.92. There was significant improvement in range of motion. In our study when applied mobilization in preposition at lumber region the mean difference for lumber right flexion was 6.3 and for lumber left flexion was 7. This mean also in our study when apply mobilization in preposition at lumber region there is significant improvement in range of motion 25.
CONCLUSION
It is concluded that segmental mobilization in pre-position has better effects than prone position in patients with chronic low back pain in terms of pain, disability, pressure pain threshold and lumber range of motion.
AKNOWLEDMENT
I am very thankful to my supervisor prof. Shakeel Ur Rehman. Riphah International University Lahore. The cooperation of General hospital, Lahore and THQ, Kot momin to allow me for data collection.
REFERENCE
- Tüzün EH, Gildir S, Angın E, Tecer BH, Dana KÖ, and Malkoç M. Effectiveness of dry needling versus a classical physiotherapy program in patients with chronic low-back pain: a single-blind, randomized, controlled trial. Journal of physical therapy science. 2017; 29(9):1502-9.
- Garcia JB, Hernandez-Castro JJ, Nunez RG, Pazos MA, Aguirre JO, Jreige A, Delgado W, Serpentegui M, Berenguel M, Cantisani AF. Prevalence of low back pain in Latin America: a systematic literature review. Pain Physician, ISSN: 21501149, 15333159, Vol. 17, No. 5 (2014); pp. 379-391. 2014.
- Qaseem A, Wilt TJ, McLean RM, Forciea MA. Noninvasive treatments for acute, subacute, and chronic low back pain: a clinical practice guideline from the American College of Physicians. Annals of internal medicine. 2017 Apr 4; 166(7):514-30.
- Urits I, Burshtein A, Sharma M, Testa L, Gold PA, Orhurhu V, Viswanath O, Jones MR, Sidransky MA, Spektor B, Kaye AD. Low back pain, a comprehensive review: pathophysiology, diagnosis, and treatment. Current pain and headache reports. 2019 Mar; 23(3):1-0.
- Jeong UC, Kim CY, Park YH, Hwang-Bo G, Nam CW. The effects of self-mobilization techniques for the sciatic nerves on physical functions and health of low back pain patients with lower limb radiating pain. Journal of physical therapy science. 2016; 28(1):46-50.
- Das SM, Dowle P, Iyengar R. Effect of spinal mobilization with leg movement as an adjunct to neural mobilization and conventional therapy in patients with lumbar radiculopathy: Randomized controlled trial. J Med Sci Res. 2018; 6(1):11-9.
- Oliveira CB, Maher CG, Pinto RZ, Traeger AC, Lin CW, Chenot JF, van Tulder M, Koes BW. Clinical practice guidelines for the management of non-specific low back pain in primary care: an updated overview. European Spine Journal. 2018 Nov; 27(11):2791-803.
- Wirth B, Gassner A, de Bruin ED, Axén I, Swanenburg J, Humphreys BK, Schweinhardt P. Neurophysiological effects of high velocity and low amplitude spinal manipulation in symptomatic and asymptomatic humans: a systematic literature review. Spine. 2019 Aug 1; 44(15):E914-26.
- Makovac E, Venezia A, Hohenschurz-Schmidt D, Dipasquale O, Jackson JB, Medina S, O’Daly O, Williams SC, McMahon SB, Howard MA. The association between pain-induced autonomic reactivity and descending pain control is mediated by the periaqueductal grey. bioRxiv. 2020 Jan 1.
- Abdelgawaad AS, Babic D, Siam AE, Ezzati A. Extraforaminal microscopic assisted percutaneous nucleotomy for foraminal and extraforaminal lumbar disc herniations. The Spine Journal. 2018 Apr 1; 18(4):620-5.
- Emery RD. Manual therapy treatment for lumbar stenosis and accompanying radiating pain(Doctoral dissertation, Florida Gulf Coast University).
- Kim JE, Cho JE, Do KS, Lim SY, Kim HJ, Yim JE. Effect of cupping therapy on range of motion, pain threshold, and muscle activity of the hamstring muscle compared to passive stretching. Journal of the Korean Society of Physical Medicine. 2017; 12(3):23-32.
- Cook C. Orthopedic manual therapy. Upper Saddle River, NJ: Prentice Hall; 2011 Nov 21.
- Creighton D, Schweiger A, Cubr S. Immediate Effects of Side Lying Manual Lumbar Traction in Patients with Painful Active Lumbar Motion. Journal of International Academy of Physical Therapy Research. 2017; 8(1):1071-6.
- Alghadir AH, Anwer S, Iqbal A, Iqbal ZA. Test–retest reliability, validity, and minimum detectable change of visual analog, numerical rating, and verbal rating scales for measurement of osteoarthritic knee pain. Journal of pain research. 2018; 11:851.
- Cheatham SW, Kolber MJ, Mokha GM, Hanney WJ. Concurrent validation of a pressure pain threshold scale for individuals with myofascial pain syndrome and fibromyalgia. Journal of Manual & Manipulative Therapy. 2018 Jan 1; 26(1):25-35.
- Lee CP, Fu TS, Liu CY, Hung CI. Psychometric evaluation of the Oswestry Disability Index in patients with chronic low back pain: factor and Mokken analyses. Health and quality of life outcomes. 2017 Dec; 15(1):1-7.
- Jairakdee Y, Chansirinukor W, Sitti T. Effect of releasing quadratus lumborum muscle on hip and knee muscle length in asymptomatic individuals. Journal of Bodywork and Movement Therapies. 2021 Apr 1; 26:542-7.
- Sundaram MS. Comparing the effects of pilates and conventional core stabilization exercise with moist hot pack in females with low back pain. 2017I June 3 (2), 283 -289.
- Ebadi S, Ansari NN, Ahadi T, Fallah E, Forogh B. No immediate analgesic effect of diadynamic current in patients with nonspecific low back pain in comparison to TENS. Journal of bodywork and movement therapies. 2018 Jul 1; 22(3):693-9.
- Dickey JP, Pierrynowski MR, Bednar DA, Yang SX. Relationship between pain and vertebral motion in chronic low-back pain subjects. Clinical Biomechanics. 2002 Jun 1; 17(5):345-52.
- Ahmed R, Shakil-ur-Rehman S, Sibtain F. Comparison between specific lumber mobilization and core-stability exercises with core-stability exercises alone in mechanical low back pain. Pakistan journal of medical sciences. 2014 Jan; 30(1):157.
- Waqqar S, Shakil-ur-Rehman S, Ahmad S. McKenzie treatment versus mulligan sustained natural apophyseal glides for chronic mechanical low back pain. Pakistan Journal of Medical Sciences. 2016 Mar; 32(2):476.
- Ain SQ, Rehman SS, Maryam M, Kiani SK. Effects of Sustained Natural Apophyseal Glides with and without thoracic posture correction techniques on mechanical back pain: a randomized control trial. JPMA. 2019 Nov.
- Creighton DS, Marsh D, Gruca M, Walter M. The application of a pre-positioned upper cervical traction mobilization to patients with painful active cervical rotation impairment: A case series. Journal of back and musculoskeletal rehabilitation. 2017 Jan 1; 30(5):1053-9.
