ABSTRACT
BACKGROUND AND AIM
Clinical rotation is perceived as a burden by students due to number of challenges in experimental environment that impedes their learning in clinical areas. This study aimed to determine the perception of physical therapy students regarding prerequisite for integrating skills and knowledge from the classroom to clinical setting.
METHODOLOGY
A cross sectional study was conducted at students of different colleges of Rehabilitation Sciences on 168 candidate of clinical years. The questionnaire was designed on five domains that included patient contacts, theory v/s practice gap, communication with clinical supervision, transition from pre-clinical to clinical and knowledge and skills. The data was measured on 5 points Likert scale and was statistically analyzed on IBM SPSS version 2.0
RESULTS
Around 45% students indicated that they hesitated in taking guidance or asking question from clinical supervisors however, 76.6% students reported that a structured orientation with the staff and environment should be given to the new assistants for smooth transition from pre-clinical to clinical. Moreover, more than half of the students (58%) reported difficulty in bridging theory and practicing the knowledge. Furthermore 65% students reported hesitency in taking history and performing physical examination
CONCLUSION
Multiple challenges perceived by the students during their clinical rotations that mainly include inadequate clinical supervision, difficulty in transition from preclinical to clinical, lack of knowledge and skills, gap between theory and practice which hindered their learning.
KEY WORDS
Internship, Perception, Physical Therapy, Knowledge, Clinical Skills, Physical Examination, Malpractice.
Dr. Tabish Fahim
Assistant Professor,
Physiotherapy Department, SOMAS, G D Goenka University Sohna, Haryana, India.
Dr. Shadab Uddin
Senior Lecture
Physical Therapy Department
College of Applied Medical Sciences, Jazan University,
Jazan, Saudi Arabia.
[Fahim T, Uddin S. Knowledge of Physiotherapy Students about Supervision Skills during the Clinical Rotation of Internship. Pak.j.rehabil. 2021;10(2):44-51] DOI: 10.36283/pjr.zu.10.2/007
This is an open-access article distributed under the terms of the Creative
Commons Attribution Licence (CC BY) 4.0 https://creativecommons.
INTRODUCTION
Clinical rotation is an attainment of professional expertise by using existent classroom knowledge into patient condition-based practice under supervision.1 The main focus of medical students is to excel in both basic sciences and clinical skills during their undergraduate studies. Therefore; they are directed to develop well-build knowledge of basic sciences in the initial two years and good clinical skills in the later years. During clinical rotations, students have exposure to different domains of clinical sciences that attributes to enhance their communication and hands-on skills. Moreover, the experience of treating diversified patients also contributes in the development of confidence and clinical competencies that finally help them to be a good practitioner.2 In addition to this, Clinical rotation is an important part of the medical curriculum as it is focused and aimed to relate basic sciences with clinical knowledge and also contributes in the adjustment of students in the hospital setting. Students are rotated in both outpatient and inpatient area that furnish their clinical and clinical decision making skills.3 Healthcare professionals enable the students and provide opportunities to incorporate the basic knowledge and clinical skills in making differential diagnosis and foster their critical thinking abilities.4 Therefore, Clinical rotation is considered to be a key domain of physical therapy curriculum connecting theoretical knowledge with the clinical and contributes in the development of professionalism among the physical therapy students.5 The failure to establish a link between theoretical information obtained with the existing and actual application in health care practice is known as theory practice gap, and this gap has been recognized in many studies.6 Furthermore, one researcher claimed that the time the student spends on practical and clinical aspects is inadequate as compared to the time spent on the theoretical component of the course.7 However, Positive and welcoming environment is another variable as a student’s motivator. Along with it productive criticisms in the clinical setting also help in boosting the students to be a skilled practitioner and resist in doing malpractice.8 Conversely, identifying and highlighting student’s mistake in front of patients, interrogating in an impolite way that demotivate the students, not acknowledging the extra efforts of students, insufficient teaching time, non-professionalism , uncooperative supervisors and Chaotic and disorganized environment have negative impact on the clinical learning.9 Furthermore, role shifting from student to member of healthcare team generate substantial challenges that hesitant and increase uncertainty as a novice practitioner. Ultimately this uncertainty impedes the beginners to apply properly their preclinical learning into patient problem.10 This uncertain nature of clinical course can be the main source of generating difficulties among allied students. To attain the purposeful and successful learning, clinical placement reflects the priority of knowledge and skills that cannot be implement in the absence of clinical experience.11 Moreover, an intimate challenge in professional education is the transition of students from gaining theoretical knowledge and conceptual apprehension and amplifies this knowledge as a novice practitioner. This transition occurs particularly when students proceed from preclinical phase to clinical phase. Transformation in medical education, with a source of expending competence by gaining new knowledge and skills, is emotionally and socially active process,12 but also a source of anxiety and stress that decline the capabilities of students13 and may impede their training.
METHODOLOGY
Study Setting
The study was conducted at Colleges of Rehabilitation Sciences.
Target Population
The target population was students who have done their clinical rotations during internship.
Study Design
It was an observational cross sectional study.
Duration of Study
Six months after the approval of synopsis.
Sampling Technique
Non-probability, convenience sampling techniques
Sample Size
168 participants
Data Analysis
Data was analysed on SPSS (Statistical Package for Social Sciences) version 20. The demographic characteristics of the participants were represented through frequency, mean and standard deviations whereas the participant responses were evaluated through frequency and percentage.
Inclusion Criteria
- Both male and female
- BPT Students who have cleared their four years of study.
Exclusion Criteria
- Students who have not cleared their examination of all four years of study.
Data Collection Tool
The data was collected from physical therapy students using a researcher developed questionnaire adapted from the article written by Muhamed E.L.hassan Abdallah and Sarra shorbagi”.10 Challenges faced by medical students during their first clerkship training”, in 2018. The questionnaire is modified according to the current research scenario. The questionnaire comprised of close ended questions focusing on five domains that includes patient contacts, theory v/s practice gap, communication with clinical supervision, transition from pre-clinical to clinical and knowledge and skills. The data was measured on 5 points Likert scale where 1 being “strongly disagree” and 5 being “strongly agree” for all the questions
DATA COLLECTION PROCEDURE
The data was collected from physical therapy students who have done their 8 weeks clinical rotations. Informed consent was taken from the participants and the purpose and the benefit of study was explained. The questionnaire was distributed to students when they came back from their clinical rotation.
RESULT
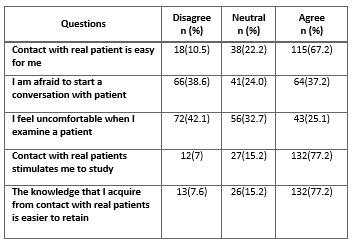
A total of 168 samples were taken including both male and female students of BPT. As for patient contact, majority number of students (38.6%) expressed that they weren’t afraid to start a conversation with patients, and 77.2% (N = 132) students mentioned that contact with patients encouraged them to study as they experienced that the knowledge acquired from practicing theoretical knowledge on patients helped them to retain while only 7.6% (N = 13) students didn’t agree. All the numbers and percentages are mentioned in the table no. 1.
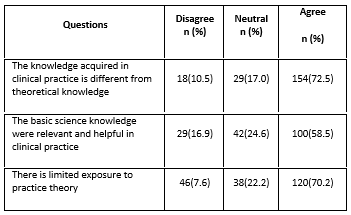
However, as far as the student’s response regarding the identification of gap between theoretical and practical knowledge is concerned, the responses were much diversified as according to feedback, 72.5% student perceived that knowledge acquired in clinical practice is different from theoretical knowledge, while 10.5% disagree. On the other hand 57.9% report that they are unable to transfer theoretical knowledge into practice, while 18.5% were not agreed. Moreover, majority of student around 70% had limited exposure to practice theory (table-2).
Communication with supervisor is another major challenge 45% (N= 108) students indicated that they hesitate in taking guidance and asking questions from clinical supervisors 31.6%(N=54) students disagree meanwhile 23.4%(N=25) were neutral. For majority of students 63.1% (N=108) clinical supervisors talk about inadequacies in clinical setting with an inappropriate manner meanwhile 22.2% (N=38) disagree and 14.6% (N=25) were neutral. A large number of students 58.5%(N=100) disagree that the competencies been arranged during clinical rotation were explained by supervisor whereas 26.9% (N=46) were neutral and only 14.6% (N=25) students agreed. Moreover 49.7%(N=85) student indicated that they do not receive sufficient supervision and constructive feedback about their performance whereas 25.1% (N=43) were neutral agree with the statement.
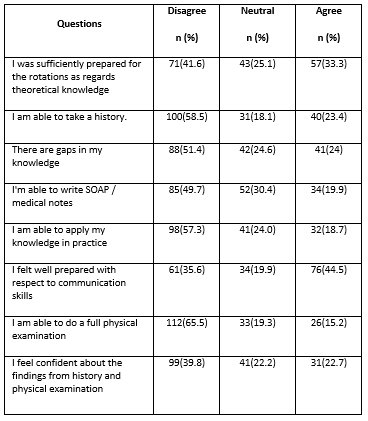
When evaluating the knowledge and skills of students, more than half of the participants were unable to apply their knowledge in practice (57.3%, N=98), only 18.7 % (N=32) were capable to apply. However, 24% responded neutral. Upon asking, 58.5 % (N=100) students respond that they were unable to take history while only 23% (N=40) were able to take (table_5).
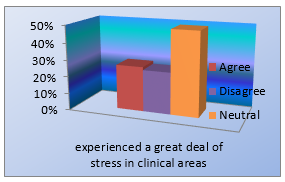
45% (N = 77) students experienced an abrupt transition from pre-clinical to clinical training and most of the students 49% (N = 84) perceived that they had an increase level of stress in clinical area. Moreover, 76.6% (N = 131) students felt that a good introduction should be given to the new clerks to make transition into clinical practice from pre-clinical less challenging whereas, only 7% (N = 12) disagreed.
DISCUSSION
Sufficient knowledge and skills are the backbone for clinical rotation. Taking part in real consultation with a real patient is a strong incentive for students to prepare for the contact. Seeing real patient excites student’s curiosity and it is more powerful motivator to study the literature. According to our research most students gave a positive feedback that they were not afraid to start a conversation with patient. Whereas, when asked if they are able to take a history or can do a physical examination a large number of population disagreed.
On the other hand, our studies revealed that majority of students were in the favor that contact with real patient stimulated them to study. On the contrary to this the gap between the theory, knowledge and practice were found to be a major issue among them and also they were unable to write the medical notes14-16.
Furthermore, in our investigation mostly students were in favors that the knowledge they retain by contact with patient was easier but they were still incapable to apply their knowledge in practice. The purpose of this study was to explain the gap students face between theory vs practical. The findings obtained from the study demonstrated that many students did not have sufficient knowledge to take care at the bedside patients. Dealing with the clinical learning environment and providing care to the patients was challenging for them. In our investigation majority of undergraduate students were agree about the knowledge acquired in clinical practice is different from theoretical knowledge14-16.
Consequently, before understudies enter the clinical condition, it ought to be found out that they are hypothetically and basically set up as they step through exams and give care in the ability lab.
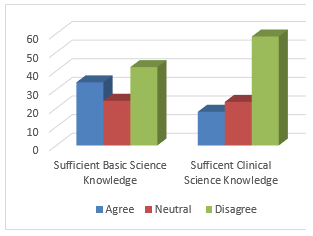
One significant statute is that fusing fundamental science preparing into the clinical years may require workforce improvement for instructors so the connection among science and the clinical choices is made explicit, concise, and clear. According to our research results majority of undergraduate students were agree about the basic science information were significant and accommodating in clinical practice the result of Nasir et al17shows that students stated, the abundance number of understudies in the research center practices in school and restricted offices adversely influence their learning. Understudies communicated that practices learned in the research center presently before clinical practice are all the more enduring. Besides, understudies brought up that the training they are appeared in school and the one acted in the facility are unique and this circumstance makes suspiciousness during a training Students who participated in the study pointed out that there is limited exposure to practice theory. It was observed that students who participated in this study majority agreed the results of Wijbenga et al15, which shows that both understudies and clinical instructors expressed patient presentation was key in the advancement of clinical thinking aptitudes. Students need ‘practice hours’ to gain proficiency with their calling and become flight chief18.
Understudies learned most when they could test their own clinical thinking approach on singular patients, all things considered, practice. Effective communication among supervisors and students is important as it greatly affects the performance and productivity of students as well as the quality of health care provided. Based on our findings, half of the undergraduate students received sufficient supervision however they did not sustain adequate response about performance. The results of Ghrayeb16 also shows that the clinical supervisors were not able to collaborate with medical students in wards, and was not able to do objective assessment for students. According to our research, undergraduate students faced negative feedback from the supervisors19. Majority of the students hesitate in taking guidance or asking questions from the supervisors. Students highlighted the impartial control of patient, right feedback from supervisor and exams as some of the important elements that enhance their learning. In addition to this, proper response by the teacher to the students in clinical learning is the most vital issue that intensifies the students’ ability. In our study majority of students were dissatisfied about the effective supervision that hinders students’ learning. Study highlighted inadequate supervision by clinical supervisors, lack of resources, and quality of practical assessment in clinical area, as some of the key factors that hinder efficacy of learning20-22.
Our study showed that there is no satisfactory supervision and constructive feedback by the supervisors about the students ‘performance however another study conclude that sufficient supervision assist the students in learning medical skills in productive manner17. Transition from pre-clinical to clinical for an orientating students’ needs a proper orientation which helps them to clarify their domains of clerkship and importance of their clerkship. In our study majority of the students wants a good introduction and orientation which was regarding clerkship moreover. Lack of preparedness for clinical training and supervision during the clerkship both hamper the transition learning23-24. In addition to this in our study inadequate training of transition from pre-clinical to clinical of a medical student was also the cause of stress among students. Similarly, another study reveals that inadequate clinical training and improper orientation were the main cause of stress and anxiety among medical students.25
CONCLUSION
Predicting the troubles confronting the new interns and executing measures to facilitate their progress ought to be a need for any in clinical teaching.
It is inescapable that understudies ought to need to acclimate to social contrasts between the study hall and the clinical setting. The current investigation affirms the earnestness of the transition, knowledge and skills issue by giving quantitative affirmation.
Clinical educators should invigorate their understudies to effectively take an interest, ideally in a group of various health care experts and assistants and uphold understudy learning by giving individual review and posing inquiries that prompt understudies to consider their activities and learning.
Understudies learning is additionally improved by monotonous practice of their skills, pointed toward coordinating components of the clinical thinking measure into a more regular stream.
REFERENCE
- Pashmdarfard M, Shafarood N. Factors affecting the clinical education of rehabilitation students in Iran: A systematic review. Medical Journal of the Islamic Republic of Iran. 2018;32:114.
- AlHaqwi AI, van der Molen HT, Schmidt HG, Magzoub ME. Determinants of effective clinical learning: a student and teacher perspective in Saudi Arabia. Education for Health. 2010 Aug 1;23(2):369.
- AAl, M., 2015. Clinical nursing teaching in Saudi Arabia challenges and suggested solutions. J Nurs Care S, 1, pp.2167-1168.
- Serrano CM, Botelho MG, Wesselink PR, Vervoorn JM. Challenges in the transition to clinical training in dentistry: an ADEE special interest group initial report. European Journal of Dental Education. 2018 Aug;22(3):e451-7.
- Ehsan S, Butt MS, Umar B. Perception of undergraduate physical therapy students regarding the clinical teaching attributes of their clinical instructors.
- Salifu DA, Gross J, Salifu MA, Ninnoni JP. Experiences and perceptions of the theory‐practice gap in nursing in a resource‐constrained setting: A qualitative description study. Nursing open. 2019 Jan;6(1):72-83.
- Kandiah DA. Perception of educational value in clinical rotations by medical students. Advances in medical education and practice. 2017;8:149.
- Gemuhay HM, Kalolo A, Mirisho R, Chipwaza B, Nyangena E. Factors affecting performance in clinical practice among preservice diploma nursing students in Northern Tanzania. Nursing Research and Practice. 2019 Mar 3;2019.
- Drateru KC. Challenges Experienced by Student Nurses During Skill Acquisition at The Clinical Area. Nur Primary Care. 2019; 3 (3): 1-4. Texila American University, Uganda.
- Abdalla ME, Shorbagi S. Challenges faced by medical students during their first clerkship training: A cross-sectional study from a medical school in the Middle East. Journal of Taibah University Medical Sciences. 2018 Aug 1;13(4):390-4.
- Liljedahl M, Boman LE, Fält CP, Laksov KB. What students really learn: contrasting medical and nursing students’ experiences of the clinical learning environment. Advances in Health Sciences Education. 2015 Aug 1;20(3):765-79.
- Atherley AE, Hambleton IR, Unwin N, George C, Lashley PM, Taylor CG. Exploring the transition of undergraduate medical students into a clinical clerkship using organizational socialization theory. Perspectives on Medical Education. 2016 Apr 1;5(2):78-87.
- Aboshaiqah, A.E., Roco, I.M., Pandaan, I.N., Baker, O.G., Tumala, R.B. and Silang, J.P.B.T., 2018. Challenges in the Clinical Environment: The Saudi Student Nurses’ Experience. Education Research International, 2018.
- Arkan B, Ordin Y, Yılmaz D. Undergraduate nursing students’ experience related to their clinical learning environment and factors affecting to their clinical learning process. Nurse education in practice. 2018 Mar 1;29:127-32.
- Wijbenga, M.H., Bovend’Eerdt, T.J. and Driessen, E.W., 2019. Physiotherapy students’ experiences with clinical reasoning during clinical placements: A qualitative study. Health professions education, 5(2), pp.126-135.
- Ghrayeb FA. Nursing and Midwifery Students Lived Experiences During Clinical Practice in Palestine.
- Nasir B, Jurd K, Cook S, Kwan M, Ostini R. Developing an Internship Preparedness Program for Final Year Medical Students. MedEdPublish. 2018 Sep 21;7.
- Macauley K, Jette DU, Brudvig TJ, Callahan J, Levangie PK. Students’ Perceptions of a New Doctor of Physical Therapy Curriculum Based on Constructivism and Cognitive Load Theories: A Qualitative Study. Journal of Physical Therapy Education. 2021 Mar 1;35(1):27-37.
- Hayward LM, Black LL, Mostrom E, Jensen GM, Ritzline PD, Perkins J. The first two years of practice: a longitudinal perspective on the learning and professional development of promising novice physical therapists. Physical therapy. 2013 Mar 1;93(3):369-83.
- Rodger S, Webb G, Devitt L, Gilbert J, Wrightson P, McMeeken J. Clinical education and practice placements in the allied health professions: an international perspective. Journal of Allied Health. 2008 Mar 14;37(1):53-62.
- Lunnen KY. Students’ perceptions of what employers consider desirable abilities, attributes and qualifications for physical therapists in today’s workforce.
- Baird N, Dilger B. How students perceive transitions: Dispositions and transfer in internships. College Composition and Communication. 2017 Jun 1:684-712.
- Bozzolan M, Simoni G, Balboni M, Fiorini F, Bombardi S, Bertin N, Da Roit M. Undergraduate physiotherapy students’ competencies, attitudes and perceptions after integrated educational pathways in evidence-based practice: a mixed methods study. Physiotherapy theory and practice. 2014 Nov 1;30(8):557-71.
- Córdova-León K, Fernández-Huerta L, Rojas-Vargas M. Perception of clinical educational environment by student of physiotherapy based on the Educational Environment Measurement Questionnaire of the Postgraduate Hospital in Chile. Journal of educational evaluation for health professions. 2019 Jun 14;16:16-.
- Hayward L, Sellheim DO, Scholl J, Joyce C. Defining Key Elements for Effective Physical Therapist–Physical Therapist Assistant Working Relationships: A Qualitative Study. Journal of Physical Therapy Education. 2021 Mar 1;35(1):19-26.
