ABSTRACT
BACKGROUND AND AIMS
The havoc caused by COVID-19 leads to have an adverse impact on medical priorities for consultation however e-consultation has been used widely by practitioners to aid the patient and healthcare providers.
METHODOLOGY
A cross-sectional survey was conducted on allied health professionals, considering physical and occupational therapists. A self-administered questionnaire regarding impact assessment and level of attained satisfaction was distributed to participants in Google Docs via email or Whatsapp groups.
RESULTS
A total number of 109 responses obtained from the participants showed (34.9%) were agreed to understand the completed condition of the patient, (38.5%) but (41.3%) disagreed to treat the patient same as physical appointment and (35.58%) disagreed to work more productively. Only (32.1%) were agreed to be satisfied during their consultation, (49.5%) agreed that e-consultation can never be adopted as a good substitute of physical appointments.
CONCLUSION
It was concluded that limited number of therapists were satisfied with their e-consultation services while majority were agreed that the service cannot be a good substitute for a physical appointment. Therefore, further trials needs to be conducted to evaluate the factors causing hindrance in healthcare delivery.
KEYWORDS
Rehabilitation, Consultation, COVID-19, Health, ADLs, Healthcare.
Mubashir Siddiqui
Occupational Therapist
Sindh Institute of Physical Medicine and Rehabilitation
Karachi, Pakistan.
[Siddiqui M. Impact and Satisfaction with E-Consultation: A Perception of Allied Health Professionals. Pak.j.rehabil.2021; 10(2):26-34] DOI: 10.36283/pjr.zu.10.2/005
This is an open-access article distributed under the terms of the Creative
Commons Attribution Licence (CC BY) 4.0 https://creativecommons.
Surging demand in allied health care services in Pakistan have been a concern for both consultants as well as patients because of the complex nature of multi-level health care subsystems involving formal and informal private and public sectors1. These services are mainly delivered through vertically managed disease-specific mechanisms which have proven to be insufficient due to a lack of alternative methodologies2. However, Pakistan’s health sector is also marked by urban-rural disparities in terms of accessibility and a massive imbalance in the allied workforce due to insufficient health managers, nurses, paramedics, and skilled birth attendants in the peripheral areas as the nature of the problem widen3. With the overall clinical workload increasing day by day there is a dire need for a system that can ease the process of providing services to patients with minimum hassle amongst public and private sectors4. In addition to it, general practices are striving hard to meet these challenges of accessibility of the services that may have become a major source of patient dissatisfaction and leads to stress among practitioners. Moreover, allied healthcare professionals in recent times of a pandemic are more encouraged to develop new and flexible alternative models for patient access, predominantly the online consultation5. In e-consultation, patients are requested to complete an online assessment to provide a structured medical background of their condition to practitioners. The patients are directed towards relevant services based on information provided to ease physical and mental constraints on practices of providers and also improving patient access to it, but unfortunately, there is limited literature is available in this regard.
Several studies have suggested that online consultations have the potential to reduce the burden and time for patients and staff as well as can lead to a more focused and time-saving than face-to-face consultations6. According to National Health Service report ”Practice Forward View” advances a more noteworthy utilization of innovation by broad practices, for model, by means of online meeting frameworks, as a possible method to satisfy need7. Additionally, there is a chance to enhance access to specialist care through the utilization of innovative e-health platforms like electronic consultation. E-Consult links medical care providers —a group that includes physicians, practitioners and specialists through electronic means and suggest specialist recommendation to be given directly, usually without the need for a face-to-face visit8. Electronic counsel is a potential solution for address delayed expert wait times that has been executed by a few nations to improve admittance to single and numerous based clinical departments9. On the contrary, the current scenario indicated a low level of involvement with the minimalistic private sector practicing and has been using some other form of electronic consultation6.
Furthermore, a very small amount of government institutions are planning to do so in near future. Consecutively, the technology that supports online consultations has advanced in recent years into health care but the experience of using such systems has yet to be fully evaluated. Therefore, this study will assess the experiences through the perspective of practitioners who are currently involved or have been associated with e-consultation systems to explore potential points related to the holistic nature of these services that may be inculcated for the future development of such systems and can make e-consultation delivery more productive and effective for the better promotion of health. Electronic consultations are described as indirect contact between the patient and the provider, are utilized to access a piece of advice from the consultant more holistically and comprehensively. These services may include telephone consultations, real-time or asynchronous telemedicine, and e-mail10. These services serve as an opportunity for improvement through the use of innovative electronic platforms. E-Consultation integrates allied health professionals through electronic sources and transpires expert advice to be given directly, mostly without the need for a face-to-face meeting8. Likewise, it has been proposed that online discussions can possibly decrease the burden of time for patients and staff, and lead to more engaged, efficient meeting. The innovation has additionally been recognized as offering improved admittance to underestimated groups who may find difficult in typical access11. Therefore, drills to redesign and restructure health care typically to the needs of the patient serve as the goals for an integrated care system and foster coordination and teamwork among primary health care providers 12.
There has always been a dire need to improve the accessibility to the consultants to reduce delays in diagnosis and serve promptly with effective treatments of the patients.13 Therefore, primary health care consultants must recognize the long duration for patients to see a consultant14. In recent times, several patients are reported to be limited to one or a maximum of two specialty services.15 Moreover, in conventional health care settings providers are integrated through a shared electronic health record facility that provides access to the patient’s history and results more effectively16 .The classic form of consultation through referral requires the patient to physically set up a meeting with the specialist before any sort of recommendations are provided to the primary health care provider17. However, the shortcomings of these consultations are strict to be exchanged between the providers and the patient in a secure and controlled environment with complete confidentiality to a maximum extent for the utilization of such services18.
Health care service providers who witness innovation as having an advantage relatively more easy over current practices19. In addition to all these technological improvements, the engagement and appointment of the service provider are extremely critical in the case of e-consultation19. Furthermore, several interventions for telehealth have been proposed to enhance communication minimize care fragmentation and reduces wait times. Despite, the possible benefits of e-consultation the rectification of it is remains limited due to fee-for-service health system in United States due to absence of reimbursement. The process of adaptation of new technology for health care providers is indeed challenging, and impediments such as the relative advantage, complexity, and observable benefits ought to be considered when implementing these new systems anywhere20. As innovation in new technologies still be introduced into health care, studies including, which provide the distinctive views of the health care facilitators who must adopt and use new systems that are necessary. Our results can facilitate others who are considering implementing similar systems8. In Pakistan, there are negligible experiences reported in the literature therefore, this study leads to further exploration of revolutionizing health care services of Pakistan for the future to come.
Study Setting: The data was collected from primary and tertiary care hospitals of Karachi.
Target Population: Allied health professionals, occupation and physical therapists.
Study Design: Cross-sectional survey.
Duration of Study: 6-8 months.
Sampling Technique: Non-Probability Convenience Sampling Technique.
Sample Size: n=384
Sample Selection
Inclusion criteria
- Male and female OT‟s and PT‟s aged 25-65 years currently working in clinics or academics with an experience of at least 1 year or more.
Exclusion criteria
- Therapists not working currently or on house job, and those who refuse to participate.
Data Collection Tool: Data was collected through self-administered questionnaire which includes demographics of the participants and questions regarding impact assessment and level of attained satisfaction on the likert scale of strongly agree, agree, neither agree nor disagree, disagree, strongly disagree respectively.
Data Collection Procedure: Data was collected from OT‟s and PT‟s from of primary and tertiary care hospitals of Karachi, recruited via convenience sampling technique. Prior to data collection all participants were provided with informed consent to ensure their voluntary participation. The questionnaire was formulated into Google Docs and sent to participants via email or Whatsapp groups. The responses were then analyzed to assess the impact and satisfaction regarding e-consultation.
Data Analysis Strategy: Data was analyzed on Google Docs Editor. The demographic characteristics of the participants were represented through frequency, mean and standard deviations whereas the participant responses were evaluated through frequency and percentage.
Ethical Considerations: Ethical consideration was taken via verbal and written consent by the participant before starting the data collection. All information of the participants will be kept anonymous under investigator’s supervision.
A total number of 109 responses obtained from the participants including 64 (58.7%) females and 45 (41.3%) males respectively with highest responses reported form 20-25 years (44%) (Figure-1) comprised of 63 (57.8%) physiotherapists and 46 (42.25) occupational therapists including (67.9%) graduates and 31 (28.4%) masters with 0-5 years (66.1%) of level of experience followed by 5-10 years (18.3%) and >10 years (15.6%).
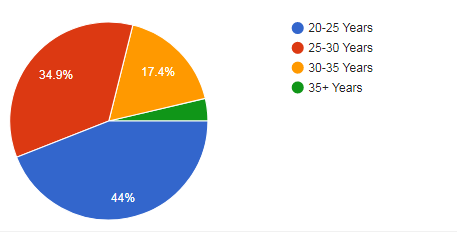
Figure-1 shows age range of participants included in the study
The e-consultation services provided by therapists showed that (34.9%) were agreed to understand the completed condition of the patient, (38.5%) somewhat agreed to define the course of action but (41.3%) disagreed to treat the patient same as physical appointment and (35.58%) disagreed to work more productively as shown in Figure-2
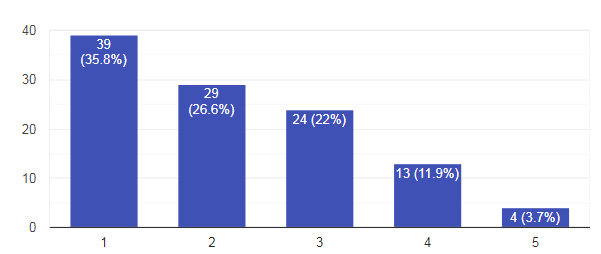
Figure-2 show percentage of work productivity in providing e-consultation services
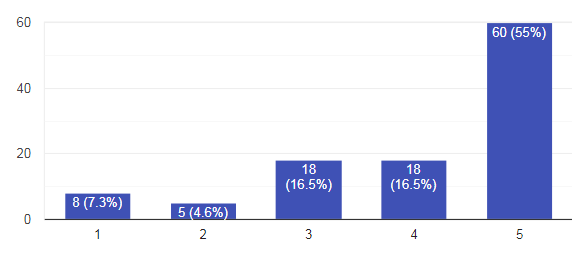
In the acquired healthcare services, (25.7%) therapists were able to understand the complete condition of patient during e-consultation while (12.8%) were unable to do so. Moreover, (37.6%) were able to work productively. Therefore, (60%) therapists agreed to find e-consultation as a good substitute as shown in Figure-3 while only (12.8%) were unable to define course of action.
Figure-3 show percentage of work regarding e-consultation as a substitute to physical appointments
In the level of attained satisfaction by therapists, only (32.1%) were agreed to be satisfied during their consultation, (28.4%) were found to be satisfied with their course of action while (28.4%) remain neutral in this regard. However, only (4.6%) were agreed to be satisfied of their devised treatment plan but (26.6%) remain convinced that they were unable to understand the complete condition of the patient during e-consultation. Consecutively, (49.5%) agreed that e-consultation can never be adopted as a good substitute of physical appointments as shown in Figure-4.
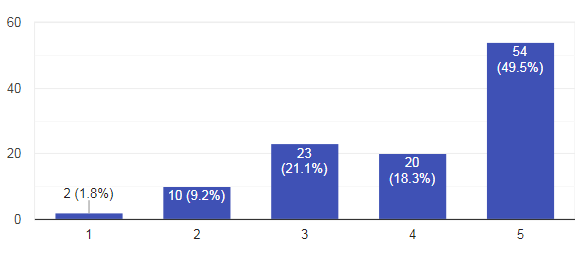
Figure-4 show percentage of therapists regarding e-consultation as a substitute for physical appointments
However, (54.1%) were remain neutral regarding their learning and productivity in rendering e-consultation services as shown in Figure-5.
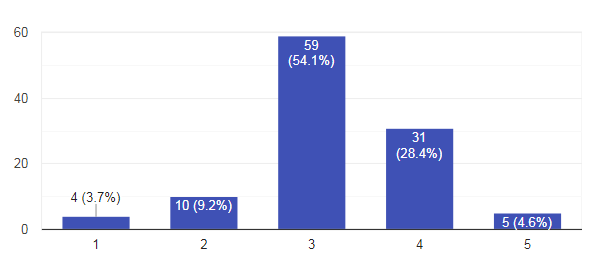
Figure-5 show percentage of therapists in learning and productivity in rendering e-consultation services
DISCUSSION
The findings of this study showed that e-consultation services provided by therapists showed that (34.9%) were agreed to understand the completed condition of the patient, (38.5%) but (41.3%) disagreed to treat the patient same as physical appointment and (35.58%) disagreed to work more productively. Only (32.1%) were agreed to be satisfied during their consultation, (4.6%) were agreed to be satisfied of their devised treatment plan but (26.6%) remain convinced that they were unable to understand the complete condition of the patient during e-consultation. Consecutively, (49.5%) agreed that e-consultation can never be adopted as a good substitute of physical appointments although e-consultation is revolutionizing the world during this pandemic and have proven itself to be a savior in many cases. However, the rehabilitation services such as occupational therapy or physiotherapy requires a little more effort, as in these fields’ interaction is the key of prognosis and success.
E-consultation services may also decrease the need for patients to time lag and to travel father for face-to-face or in-person appointments with specialists. This practice allows primary care professionals to communicate directly with sub-specialists for supervision8-10. However, limited studies has been conducted to determine the link between using an e-consult service and to avoid face-to-face referrals as well as specific content inside each session. It has also been evident that e-consultation sessions are dependent upon the the type of question asked, its framing, and the speciality being addressed that will be significantly associated with referral outcomes12-14. Besides of the disparities between primary healthcare practitioners on which patients require in-person referrals may be beneficial to detect knowledge gaps and direct professional growth. Furthermore, studies reported that certain questions are associated with the highest avoided referral rates included non-specific requests, pertaining to diagnosis, questions without specified interventions with most discrepancies due to the health care providers making a referral without the specialist recommendation20.
In this survey, number of questions regarding inclusion of e-consultation services have answered a cumulatively series of questions on the current system showed that physical appointments are much better than e-consultation in terms of understanding and responsiveness, awareness regarding e-consultation should be provided beforehand as everyone is not that adaptive in this particular domain. Similarly, practices were initially intrigued by the framework to improve and make efficiencies. While a few patients utilized the framework to attempt to save time for both themselves and their GP. Different patients were initiated to utilize e-interviews when they couldn’t get a convenient arrangement. Since pratices were reliant upon patients choosing how and when to utilize e-meetings, more clear direction might be required for patients to help more proficient utilization of e-counsels 21. Physical examination and exercise routines are inseparable part of this field. In particular, the service is easier but lack potential to actually generate results in this particular field7. However during pandemic, it’s a considerable option as most of the people are left out with no other option. Studies have suggested that future use of e-consultations is estimated to account for 30 to 40% with the GP if supported by applications or wearable system22. Similarly, in most of the regions, one-third of all consultations with the GP will be digital in future constitutes of electronic booking of appointments and prescription renewal23. However, the e-consultation service for medical inquiries is still used at a lower degree, as indicated in a recent qualitative study. Despite the fact, time-saving represents the most evident benefit for patients who seek e-consultation i.e. 95% of the users perceived the service as more efficient than the phone24. This was confirmed by the differences in time spent using digital health services compared with conventional approaches was found to be statistically significant. However, findings from previous studies also reported that the majority of patients received a delayed response that leads to dissatisfaction thus; quicker response times might further improve patient satisfaction in acquiring e-consultation services25.
STRENGTH
To the best of the author’s knowledge, this study is the first to be conducted in Pakistan to explore the impact of allied health professionals regarding e-consultation. Moreover, the providers showed a somewhat positive attitude towards innovation than thus be more enthusiastic and inclined to use the services.
LIMITATIONS
Several limitations occurred during this study, as information regarding the number of unique system users of the services were not available due to privacy issues. Moreover, the potential number of therapists who were eligible for this survey was unknown therefore it was not possible to calculate a response rate. Besides, a low sample was attained due to the ongoing pandemic.
FUTURE DIRECTIONS
As it is quite clear, those professionals of the field do recognize its importance during situations like pandemic, but on the other hand, prerequisites of this field create hindrances in terms of its adaptability. A mix of both systems can still work out in the field rather than a total dependency on online system.
It was concluded that limited number of therapists were satisfied with their e-consultation services while majority were agreed that the service cannot be a good substitute for a physical appointment. Therefore, further trials needs to be conducted to evaluate the factors causing hindrance in healthcare delivery. Moreover, it is important to make the service functional and provide adequate information and training for its easy access and implementation.
- Rajani A, Khan MH. Career and service structure of allied health science in pakistan, a perspective in question. PJR. 2016 Jul 1;18(3).
- Andermann A. Taking action on the social determinants of health in clinical practice: a framework for health professionals. Cmaj. 2016 Dec 6;188(17-18):E474-83.
- Paracha PI, Hameed A, Simon J, Jamil A, Nawab G. Prevalence of Anaemia in Semi-Urban Areas of Peshawar, Pakistan-A Challenge for Health Professionals and Policy Makers. Journal-Pakistan medical association. 1997 Feb 1;47:49-53.
- Frenk J, Chen L, Bhutta ZA, Cohen J, Crisp N, Evans T, Fineberg H, Garcia P, Ke Y, Kelley P, Kistnasamy B. Health professionals for a new century: transforming education to strengthen health systems in an interdependent world. The lancet. 2010 Dec 4;376(9756):1923-58.
- Saxon RL, Gray MA, Oprescu FI. Extended roles for allied health professionals: an updated systematic review of the evidence. Journal of multidisciplinary healthcare. 2014;7:479.
- Speyer R, Denman D, Wilkes-Gillan S, Chen YW, Bogaardt H, Kim JH, Heckathorn DE, Cordier R. Effects of telehealth by allied health professionals and nurses in rural and remote areas: a systematic review and meta-analysis. Journal of rehabilitation medicine. 2018 Mar 5;50(3):225-35.
- Edwards HB, Marques E, Hollingworth W, Horwood J, Farr M, Bernard E, Salisbury C, Northstone K. Use of a primary care online consultation system, by whom, when and why: evaluation of a pilot observational study in 36 general practices in South West England. BMJ open. 2017 Nov 1;7(11).
- Liddy C, Rowan MS, Afkham A, Maranger J, Keely E. Building access to specialist care through e-consultation. Open Medicine. 2013;7(1):e1.
- Lai L, Liddy C, Keely E, Afkham A, Kurzawa J, Abdeen N, Audcent T, Bromwich M, Brophy J, Carsen S, Fournier A. The impact of electronic consultation on a Canadian tertiary care pediatric specialty referral system: A prospective single-center observational study. PloS one. 2018 Jan 10;13(1):e0190247.
- Caffery LJ, Smith AC. A literature review of email-based telemedicine. Stud Health Technol Inform. 2010 Jan 1;161:20-34.
- Banks J, Farr M, Salisbury C, Bernard E, Northstone K, Edwards H, Horwood J. Use of an electronic consultation system in primary care: a qualitative interview study. British Journal of General Practice. 2018 Jan 1;68(666):e1-8.
- Gibson S, McCrea J, Morgan S. Northern Ireland Waiting Time Statistics.
- Keely E, Liddy C, Afkham A. Utilization, benefits, and impact of an e-consultation service across diverse specialties and primary care providers. Telemedicine and e-Health. 2013 Oct 1;19(10):733-8.
- Schoen C, Osborn R, Squires D, Doty M, Rasmussen P, Pierson R, Applebaum S. A survey of primary care doctors in ten countries shows progress in use of health information technology, less in other areas. Health affairs. 2012 Dec 1;31(12):2805-16.
- Tran C, Liddy C, Pinto N, Keely E. Impact of question content on e-consultation outcomes. TELEMEDICINE and e-HEALTH. 2016 Mar 1;22(3):216-22.
- Angstman KB, Rohrer JE, Adamson SC, Chaudhry R. Impact of e-consults on return visits of primary care patients. The health care manager. 2009 Jul 1;28(3):253-7.
- Bichel A, Erfle S, Wiebe V, Axelrod D, Conly J. Improving patient access to medical services: preventing the patient from being lost in translation. Healthc Q. 2009 Jan 1;13(Spec. Issue):61-8.
- Rushakoff RJ, Woeber KA. Evaluation of a “formal” endocrinology curbside consultation service: Advice by means of the internet, fax, and telephone. Endocrine Practice. 2003 Mar 1;9(2):124-7.
- Gagnon MP, Desmartis M, Labrecque M, Car J, Pagliari C, Pluye P, Frémont P, Gagnon J, Tremblay N, Légaré F. Systematic review of factors influencing the adoption of information and communication technologies by healthcare professionals. Journal of medical systems. 2012 Feb;36(1):241-77.
- Greenhalgh T, Robert G, Macfarlane F, Bate P, Kyriakidou O. Diffusion of innovations in service organizations: systematic review and recommendations. The milbank quarterly. 2004 Dec;82(4):581-629.
- Farr M, Banks J, Edwards HB, Northstone K, Bernard E, Salisbury C, Horwood J. Implementing online consultations in primary care: a mixed-method evaluation extending normalisation process theory through service co-production. BMJ open. 2018 Mar 1;8(3).
- Fagerlund AJ, Holm IM, Zanaboni P. General practitioners’ perceptions towards the use of digital health services for citizens in primary care: a qualitative interview study. BMJ open. 2019 May 1;9(5):e028251.
- Katz SJ, Moyer CA, Cox DT, Stern DT. Effect of a triage‐based e‐mail system on clinic resource use and patient and physician satisfaction in primary care: a randomized controlled trial. Journal of general internal medicine. 2003 Sep;18(9):736-44.
- Leong SL, Gingrich D, Lewis PR, Mauger DT, George JH. Enhancing doctor-patient communication using email: a pilot study. The Journal of the American Board of Family Practice. 2005 May 1;18(3):180-8.
- Lugtenberg M, Pasveer D, van der Weijden T, Westert GP, Kool RB. Exposure to and experiences with a computerized decision support intervention in primary care: results from a process evaluation. BMC family practice. 2015 Dec;16(1):1-0.
