ABSTRACT
BACKGROUND & OBJECTIVE
Stroke is a very common neurological condition affects various aspects of health. The primary objective of this study was to find out the frequency of functional disability and cognitive impairments in Sub-acute Stroke patients.
MATERIAL AND METHODS
A cross-sectional survey was conducted on 112 Sub-acute Stroke patients in Karachi, Pakistan. Using Barthel Index (BI) and Mini-Mental State Examination (MMSE) test was used to find out the frequency of functional disability and cognitive impairments of Sub-acute Stroke patients.
RESULTS
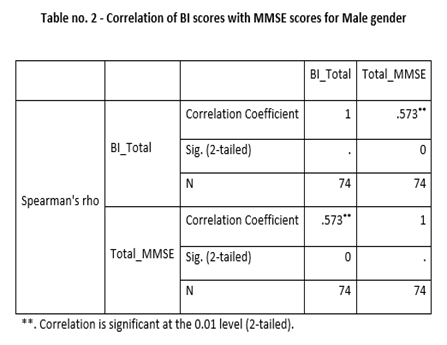
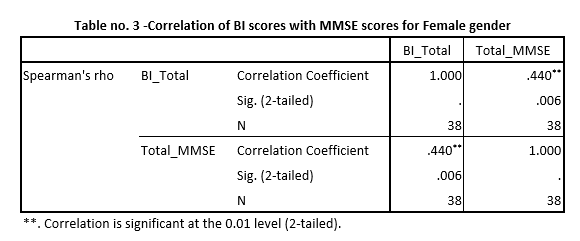
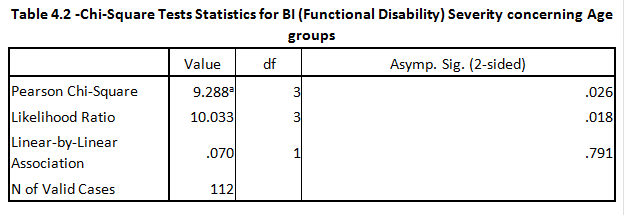
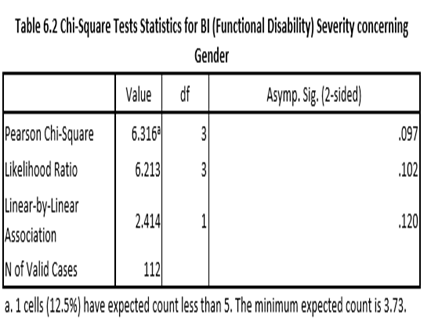
The correlation of BI scores with MMSE scores for the Male gender was 0.576 whilst the correlation of BI scores with MMSE scores for the Female gender was 0.440. The severity of functional disability concerning age groups assessed P-value was 0.026 using Chi-Square Test. The severity of functional disability (BI severity) concerning gender, P-value was found 0.097 using the same test.
CONCLUSION
Functional Disability is directly linked with age. However, there was no linkage established between Cognitive Impairment and age as well as gender. On close inspection, there was a trend between Functional disability and gender but not statistically significant.
KEYWORDS
Functional, Disability, Cognitive, Sub-Acute, Stroke, Barthel Index, Neurological.
Aisha Sarfaraz
Doctor of Physical Therapy
Rabia moon Hospital
Senior Physical Therapist
Karachi, Pakistan.
Dr Abdul Azeem
Instructor Cardiac Surgeon
Tabba Heart Institute
Karachi, Pakistan.
Mehwish Butt
Doctor of Physical Therapy
Liaquat National Hospital
Karachi, Pakistan.
Muhammad Umar
Student – Sheffield Hallam University.
Sheffield, Howard Street, UK.
[Sarfaraz A, Azeem A, Butt Me, Umar M. Frequency of Functional Disability and Cognitive Impairments In Sub-Acute Stroke Patients. An Observational Study. Pak.j.rehabil. 2021; 10(2):95-102] DOI: 10.36283/pjr.zu.10.2/013
This is an open-access article distributed under the terms of the Creative
Commons Attribution Licence (CC BY) 4.0 https://creativecommons.
INTRODUCTION
Stroke or Cardio Vascular Accident (CVA) is a common, serious, and disabling global health-related problem.1 Common risk factors of Stroke include age, diabetes mellitus, smoking, increased systolic blood pressure, prolonged use of antihypertensive drugs, and history of prior heart disease.2 Incidence of stoke is high among Pakistani population as compared to other developed countries with the world’s highest rate of stroke recorded in Pakistan per capita. The risk factor of stroke include hypertension, diabetes mellitus, prolong contraceptive use, dysthymias (atrial fibrillation, atrial flutter) Rheumatic/valve heart disease, socioeconomic background and health status but hypertension was most common risk factor according to prevalence rate3.
From all neurological conditions, it is one of the most catastrophic conditions.3 Furthermore, 15 million people out of the total world population receives this Neurological condition, out of these 15 million, 5.5 million deaths occur annually, in the USA, the death ratio is about 140,000, in Canada, 15,409 people get died in the year of 2001, Europe average approximately 650,000 each year, by the year of 2025, it is estimated that elder world population (more than 65 years of age) will suffer more and the ratio will be around 9 million.3 In India, the predominance of intellectual weakness is accounted for as 20% in complete stroke survivors. Moreover, the assessments of the commonness of psychological disability post-stroke range from 12% to 60% and differ as indicated by setting (emergency clinic versus local area), time since stroke, and incorporation of pre-stroke dementia3-4.
All around, 90% of the stroke victims as estimated in “disability-adjusted life years” or DALYs are affecting by the changeable risk factors, including 74% because of adaptive factors such as smoking, poor nourishment and less amount of physical movement.4 Furthermore, various factors related to metabolism such as raised systolic blood pressure, increased BMI, raised fasting plasma glucose level, raised cholesterol level and low GFR; 72% and environmental components include air contamination and infiltration of lead which contributed 33%, are the 2nd and 3rd biggest supporters of DALYs.4
Many physical impairments are treating by clinicians to rehab the stroke patients like muscle tone, muscle weakness, proprioception, sensory and motor deficits, muscle imbalance, alternation in line of gravity (LOG), and base of support (BOS), decrease safety awareness, and poor balance.5-7 The major cause of dysfunction in adults is high between 50 to 60 years of age thereby increasing mortality ratio that may cause economic burden on the society.
Decreased muscular strength (muscular weakness) and coordination are common symptoms of stroke; it can be in one or more than one extremities. This muscular weakness can occur in one part of the body like a hand, but mostly it occurs in more than one part on the same side of the body.8 Spasticity is another physical impairment in stroke patients it is characterized by the increased muscular tone, clonus (muscular contractions and relaxations in oscillatory fashion as the result of muscular stretching), and exaggerated stretch reflexes. It is probably caused by the removal of inhibitory influences exerted by the cortex on the postural centers of the vestibular nuclei in the reticular formation.8 Furthermore, Psychological impedance is linked to decreased activities of daily living and instrumental activities of daily living capacity, and patients may require long-term, ongoing repair. Patients with psychological impairment tend to be more organized, handicapped, have a higher death rate, and have a lower quality of life.
Despite of the number of impairments following stroke, cognition is characterized as an aspect of psychology that is responsible for processing information and comprehension in mind involving memory, judgment, thinking and observation that may have a significant role in emotional conduct. Moreover, functions of cognition are at an utmost requirement to perform activities of daily living and certain tasks, specifically for the purpose of rehabilitation such that cognition plays an important role in rehabilitation of clients having different diagnosis or conditions. However, daily and instrumental activities of life may get affected by the limitation of cognition, prompting to alter quality of life. Such deficit may leads to adverse consequences in performing tasks. Approximately more than 72% of stroke victims develop some minor cognitive impairment.9 It has been revealed that impairments include memory, problem-solving, speech, executive functions, and attention.10 Although, cognitive impairments are undetectable as clients have less familiarity and increase progression thus it is hard to perceive the cognitive deficiency in discipline of healthcare.
In 1965, Barthel Index (BI) came into existence, and after some time Granger and his co-workers modified it as a scoring tool that measures the victim’s performance in ten different ADLs. These ADLs can be placed into different groups that are related to self-care (grooming, dressing, feeding, bathing, toilet use, and bowel and bladder care) and a group related to overall movement (stair climbing, transfer, and ambulation).11-14 The total score is 100. 0 is considered the lowest score, indicating bed-bound state and total dependency, as the patient is progressing towards 100, indicating the independency.15-17
Post-Stroke Cognitive impairment is also very common and it is the predictor of early mortality and dependency. Approximately 10% of stroke victims who receive this neurological condition the very first time, also develop dementia. And 30% develop with recurrent stroke attacks. Although there is thus a need for short feasible tests of global cognition in stroke, the Mini-Mental State Examination (MMSE) is widely used.18 It is the tool that assesses cognition both in research study and clinical setup. The MMSE is divided into 2 parts, the first of which requires oral responses only and covers, orientation, memory, and attention. The second part tests subject’s ability to name objects, follow verbal and written commands, write a sentence and copy a complex polygon. The maximum total score is 30.19 Although MMSE is frequently used for evaluating cognitive functions in clinical practice, it has some limitations. It is concluded that MMSE could be inadequate in evaluating mild forms of cognitive dysfunction and cognitive impairments due to right hemisphere dysfunction.20
METHODOLGY
Sample Size
112
Study Design
Cross-Sectional
Sampling Method
Non–Probability Purposive Sampling Technique
A cross-sectional descriptive survey had been conducted among patients in different private and public sector hospitals in Karachi, Pakistan by students of the Institute of Physical Medicine and Rehabilitation, Dow University of Health Sciences.
The sampling technique was non – probability purposive sampling technique. The sample size calculated was 249 by using WHO online sample size calculator OPEN EPI version 3, with the hypothesized frequency of 63% (cognitively impaired patients), confidence limit of 5%, and design effect of 1%.5
However, a study was performed at 112 sample sizes because of the limited and short period. And the period it took was around 2 months after the approval of the synopsis.
Inclusion criteria
Individuals with Sub-Acute Stroke patients, both male and female population, and the age limit were 25-65 years.
Exclusion criteria
Individuals with Neurological conditions other than Sub-Acute Stroke e.g TBI, SCI, Neuroma, Dementia.
Two questionnaires for this study, Barthel Index which was used to check Functional Disability, and MMSE (Mini-Mental State Examination) test which was used to check cognitive impairment, among Sub-Acute Stroke patients. The collected data were kept confidential. The research was conducted according to the principles of the declaration of Helsinki.
The data was entered and analyzed by SPSS version 21 software. Frequency and percentage were put according to gender, age groups, and severity of functional disability and cognitive impairment. Correlation analysis and Chi-Square tests were applied to generate results for this statistical analysis.
Ethical Consideration
The set of rules were followed to the standards of the affirmation of the college and has been permitted by an institute. However, written consent was obtained from each applicant before every time test was executed. All members had the right to withdraw from this study at any phase.
RESULTS
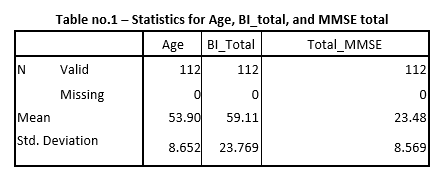
Correlation Analysis and Chi-Square test were applied during the statistical analysis to find out relations and frequencies, and tables that were generated by SPSS 21 software during statistical analysis. According to the interpretation of the tables the Mean age was 53.90 years with an S.D of 8.652 years. Mean scores for Barthel Index were 59.11 out of a total of 100 scores, with an S.D of 23.769. Mean scores of MMSE were 23.48 out of a total of 30 scores, with an S.D of 8.569. (Table no.1)
The mean age value was found in a research paper 80 years in female and 76 years in male subjects. However, this mean value of age is not matching with our study’s mean age because this study is done in western society and their life expectancy is higher than Pakistan.20
DISCUSSIONS
The primary aim of this study was to check the frequencies of Functional disability and Cognitive impairment in Sub-Acute Stroke victims. During the statistical analysis we focused on six parameters that are given below:
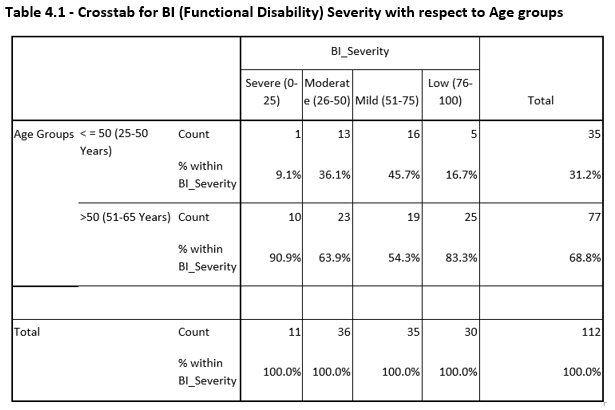
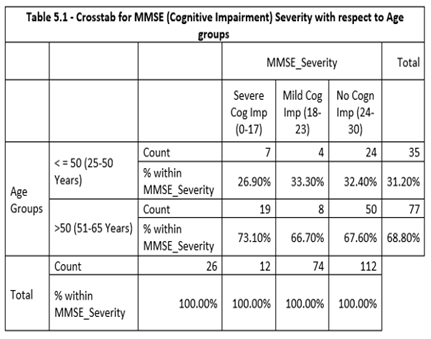
Here, above we discussed age groups, we considered two age groups. One was less than equal to 50 years (25-50 years) and the second was greater than 50 years (50-65 years). About the cutoff values for both the questionnaires, the details are given below:
As discussed above that during statistical analysis focus was on six main parameters, each one is discussed below.
When we correlated the BI scores with MMSE scores separately for the male gender there was a moderate positive correlation between BI scores and MMSE scores which means when BI score increases MMSE score also increases. When we correlated the BI scores with MMSE scores separately for the male gender there was a moderate positive correlation between BI scores and MMSE scores which means when BI score increases MMSE score also increases.
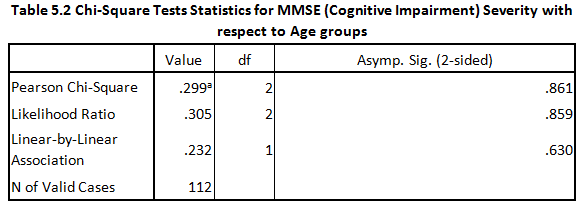
For Severity of functional disability (BI severity) with respect to age groups, Chi-Square test was applied and results showed that Functional Disability is directly linked with Age, as age increases Functional Disability also increases. On the other hand, for Severity of Cognitive impairment (MMSE severity) concerning age groups, the same test was applied and results showed that Cognitive impairment is not linked with Age.
The study concluded that there has been an increased risk of Stroke with age, leading to an increased level of disability post-stroke.21 This statement has an important impact on public health and policymaker to ensure that a sufficient amount of recourses would available to handle caring needs among the post-stroke older population.21
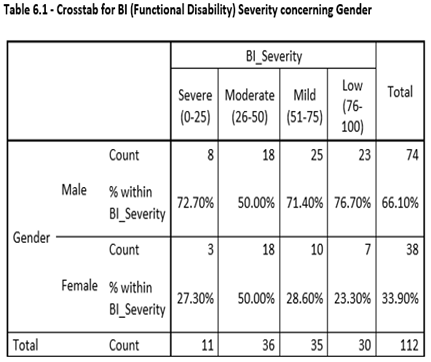
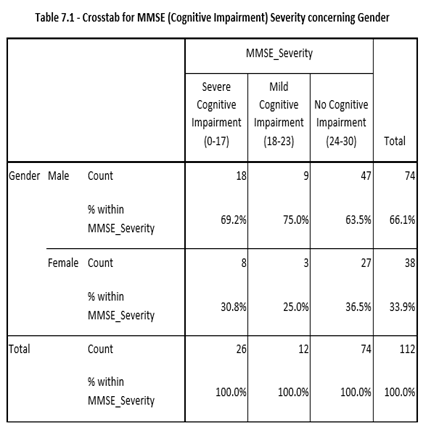
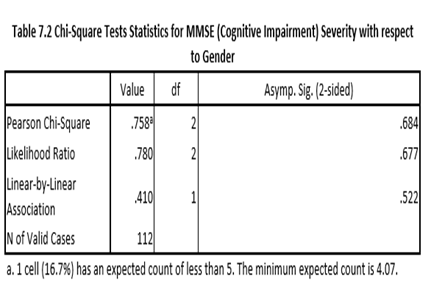
For Severity of Functional disability (BI severity) with respect to gender, the Chi-Square test was applied and results showed that Functional disability is somehow linked with gender, as P-value was very close to 0.05. On the other hand, for Severity of Cognitive (MMSE severity) for gender, the same test was used and results showed that Cognitive impairment is not linked with gender. In this study there was a moderate level of relationship was found between genders and BI & MMSE. Kelly-Hayes and co-researchers revealed that both genders similar levels of neurological deficits.22-25
Despite of the fact, the assessment strategies used by primary care professionals may be a top-down or bottom-up approaches according to the level of their competencies22. Consecutively, the standardized and non-standardized assessment tools are utilized for the assessment of specific cognitive and functional disabilities. On the other hand, cognitive capacities, memory and problem-solving strategies may also be determined through non-formal assessments20-25. On the contrary, standardized assessments utilized to quantify information with other experts on the health-care team have provided reliable and valid results as per the evidence as these assessments established for evidence-based practice in comparison to non-standardized assessments21. Thus, adequate knowledge of therapists regarding the tool or scale should be taken into consideration for better administration of outcome measures.
CONCLUSION
Functional Disability is directly linked with age. However, there was no linkage established between cognitive deficits and age as well as gender. On close inspection, there was a trend between functional disability and gender but not statistically significant. Further studies based on survey or experimental designs are needed in future to analyze the usage of cognitive and functional disability tools in the assessment of stroke-related deficits. Moreover, adequate knowledge of healthcare providers is suggestive for better administration of the functional assessments.
REFERENCES
- Langhorne P, Bernhardt J, Kwakkel G. Stroke rehabilitation. The Lancet. 2011;377(9778):1693-702.
- Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, Deo R, De Ferranti SD, Floyd J, Fornage M, Gillespie C, Isasi CR. Heart disease and stroke statistics—2017 update: a report from the American Heart Association. circulation. 2017 Mar 7;135(10):e146-603.
- Mukherjee D, Patil CG. Epidemiology and the global burden of stroke. World neurosurgery. 2011;76(6):S85-S90.
- Feigin VL, Roth GA, Naghavi M, Parmar P, Krishnamurthi R, Chugh S, et al. Global burden of stroke and risk factors in 188 countries, during 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. The Lancet Neurology. 2016;15(9):913-24.
- Paker N, Buğdaycı D, Tekdöş D, Kaya B, Dere Ç. Impact of cognitive impairment on functional outcome in stroke. Stroke Research and Treatment. 2010;2010.
- Champod AS, Gubitz GJ, Phillips SJ, Christian C, Reidy Y, Radu LM, Darvesh S, Reid JM, Kintzel F, Eskes GA. Clock Drawing Test in acute stroke and its relationship with long-term functional and cognitive outcomes. The Clinical Neuropsychologist. 2019 Jul 4;33(5):817-30.7.
- Balasubramnian S. MOTOR IMPAIRMENT FOLLOWING STROKE. Renjen PN, Gauba C, Chaudhari D. Cognitive impairment after stroke. Cureus. 2015 Sep;7(9).
- Robert Teasell MD, Macaluso S. Post-Stroke Cognitive Disorders.
- 10 Sun JH, Tan L, Yu JT. Post-stroke cognitive impairment: epidemiology, mechanisms and management. Annals of translational medicine. 2014 Aug;2(8).
- Sun JH, Tan L, Yu JT. Post-stroke cognitive impairment: epidemiology, mechanisms and management. Annals of translational medicine. 2014 Aug;2(8).
- Raju PS. Handbook of neurological physical therapy. JP Medical Ltd; 2012.
- Koch G, Bonnì S, Casula EP, Iosa M, Paolucci S, Pellicciari MC, Cinnera AM, Ponzo V, Maiella M, Picazio S, Sallustio F. Effect of cerebellar stimulation on gait and balance recovery in patients with hemiparetic stroke: a randomized clinical trial. JAMA neurology. 2019 Feb 1;76(2):170-8.
- Lo AC, Guarino PD, Richards LG, Haselkorn JK, Wittenberg GF, Federman DG, Ringer RJ, Wagner TH, Krebs HI, Volpe BT, Bever Jr CT. Robot-assisted therapy for long-term upper-limb impairment after stroke. New England Journal of Medicine. 2010 May 13;362(19):1772-83.
- Dennis M, Mead G, Forbes J, Graham C, Hackett M, Hankey GJ, House A, Lewis S, Lundström E, Sandercock P, Innes K. Effects of fluoxetine on functional outcomes after acute stroke (FOCUS): a pragmatic, double-blind, randomised, controlled trial. The Lancet. 2019 Jan 19;393(10168):265-74.
- Adeoye O, Nyström KV, Yavagal DR, Luciano J, Nogueira RG, Zorowitz RD, Khalessi AA, Bushnell C, Barsan WG, Panagos P, Alberts MJ. Recommendations for the establishment of stroke systems of care: a 2019 update: a policy statement from the American Stroke Association. Stroke. 2019 Jul;50(7):e187-210.
- Pendlebury ST, Cuthbertson FC, Welch SJ, Mehta Z, Rothwell PM. Underestimation of cognitive impairment by Mini-Mental State Examination versus the Montreal Cognitive Assessment in patients with transient ischemic attack and stroke: a population-based study. Stroke. 2010 Jun 1;41(6):1290-3.
- Spatola M, Petit-Pedrol M, Simabukuro MM, Armangue T, Castro FJ, Artigues MI, Benique MR, Benson L, Gorman M, Felipe A, Oblitas RL. Investigations in GABAA receptor antibody-associated encephalitis. Neurology. 2017 Mar 14;88(11):1012-20.
- Chan WL, Pin TW. Reliability, validity and minimal detectable change of 2-minute walk test, 6-minute walk test and 10-meter walk test in frail older adults with dementia. Experimental gerontology. 2019 Jan 1;115:9-18.
- Bernheisel CR, Schlaudecker JD, Leopold K. Subacute management of ischemic stroke. American family physician. 2011 Dec 15;84(12).
- Aad G, Abajyan T, Abbott B, Abdallah J, Khalek SA, Abdelalim AA, Aben R, Abi B, Abolins M, AbouZeid OS, Abramowicz H. Observation of a new particle in the search for the Standard Model Higgs boson with the ATLAS detector at the LHC. Physics Letters B. 2012 Sep 17;716(1):1-29.
- Raposa EB, Dietz N, Rhodes JE. Trends in volunteer mentoring in the United States: Analysis of a decade of census survey data. American Journal of Community Psychology. 2017 Mar;59(1-2):3-14.
- Winstein CJ, Stein J, Arena R, Bates B, Cherney LR, Cramer SC, Deruyter F, Eng JJ, Fisher B, Harvey RL, Lang CE. Guidelines for adult stroke rehabilitation and recovery: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2016 Jun;47(6):e98-169.
- Patel, M.D., Coshall, C., Rudd, A.G. and Wolfe, C.D., 2002. Cognitive impairment after stroke: clinical determinants and its associations with long‐term stroke outcomes. Journal of the American Geriatrics Society, 50(4), pp.700-706.
- Levine DA, Galecki AT, Langa KM, Unverzagt FW, Kabeto MU, Giordani B, Wadley VG. Trajectory of cognitive decline after incident stroke. Jama. 2015 Jul 7;314(1):41-51.
- Rosenich E, Hordacre B, Paquet C, Koblar SA, Hillier SL. Cognitive reserve as an emerging concept in stroke recovery. Neurorehabilitation and neural repair. 2020 Mar;34(3):187-99.
