KNEE JOINT
Knee joint is the largest synovial joint in the body, combined considerable mobility and strength with the stability necessary to lock the knee in the upright position. A bicondylar hinge joint, the knee is made up of three functional units; the medial and lateral tibiofibular compartments and the patellofemoral joint. The superior tibiofibular joint is included in the knee complex, which is often forgotten as a source of lateral leg and knee pain. It needs to be examined routinely in movement disorders of both the foot and the knee1.
HISTORY
In the musculoskeletal disorders, knee (OA) is one of the most common disorders which affect the patients and it exceeds prevailing articular disorder. It is also the major cause of disability and socioeconomic burden2.
EXAMINATION
The diagnosis of the knee can be done with considerable certainty and many conditions are easily curable. History is of critical diagnostic importance. The knee pain is usually Well localized and many of the tissues are accessible to palpation. Pain originating from the knee is limited to the four dermatomes which may also be affected by pain arising from the lumbar Spine L2 (left) L3 (right)3.
Jharna Devi
Senior Physiotherapist
Department of Physiotherapy
Ziauddin Hospital
Syed Abid Mehdi Kazmi
Manager
Department of Physiotherapy
Ziauddin Hospital
Nabiha Mujahid Faruq
Senior Physiotherapist
Department of Physiotherapy
Ziauddin Hospital
Iqbal Ahmed Siddiqui
Incharge
Department of Physiotherapy
Ziauddin Hospital
Samreen Iqbal
Senior Physiotherapist
Department of Physiotherapy
Ziauddin Hospital
Zuhaira Faruqui
Internee Physiotherapist
Department of Physiotherapy
Ziauddin Hospital
[Devi J, Kazmi SAM, Faruq NM, Siddiqui IA , Iqbal S, Faruqi Z,. Guideline for the Management of Knee Pain. Pak. j. rehabil. 2012;1(1):37-41]
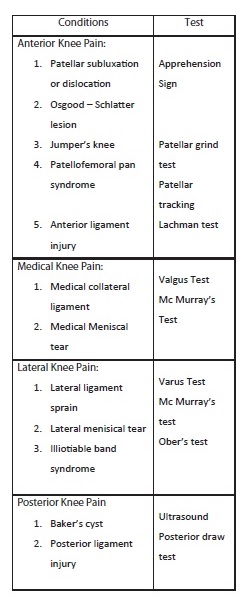
DIFFERENTIAL DIAGNOSIS (DD)
The following DD has been suggested for knee pain based on anatomical site4.
- Osgood-Schlatterdisease
Osgood-Schlatter disease is an overdoing injury which takes place in the teenager’s knee area that is caused by inflammation in the tendon below the kneecap (patellar tendon), through which it attaches with shinbone (tibia). The teenagers participating in various sports activities including gymnastics, soccer, basketball and distance running are exposed to this disease5.
Physiotherapy Treatment
- Ice or cool compress the person can get relief from the pain and reduce the swelling of the affected part of the body by applying the cool compress or ice for fifteen minutes6.
- Limitation of physical activity for six to eight weeks with a gradual return to full participation over another six-to-eight-week period has been monitored as an effective plan in reducing pain for these patients.
- Knee brace or support the stress at the tibial tuberosity may be reduced by using the strap on the front of the kneecap in the course of heavy physical activities.
- Low intensity quadriceps stretching has shown to decrease pain along with strengthening of the vastus medialis oblique, which have been observed to decrease pain for these patients7.
- Crutches The crutches may be used for few weeks by the person suffering from severe pain, it is applied for reducing the stress level on the knee and it also allows healing.
Prognosis In most of the cases Prognosis gets better after few weeks or months, it eventually leaves once the child has finished growing8.
- Jumper’s Knee
It commonly contains the attachment of kneecap tendon to the lower kneecap pole, It causes the injury or inflammation in the knee, where the thigh muscles tendon are attached to the upper kneecap pole and to lower leg bone9. The Jumper’s knee is usually observed in around 20% of jumping athletes10.
Treatment11
- The Cold therapy can be applied on the regular basis following any type of exercise.
- For reducing the pain use the knee strap for knee support.
- Transverse friction massage to the tendon.
- Quadriceps stretching and eccentric strengthening. If conservative treatments do not respond then other treatment option is surgery. After the surgery of patellar tendinopathy, it requires a number of months for rehabilitation.
- Meniscus Tear
It is rupturing of one or more of the fibro cartilage strips in the knee called menisci, which is a C-shaped piece of cartilage found in the knee joint. Meniscus protects the joint and serves as a shock-absorption system. It helps in lubricating the joint, at the same time restricts its ability to flex and extend12. Meniscal injuries are the most common knee injury, further its prevalence is 61 cases per 100,000 persons. After the age of 65 years degenerative meniscal tear is 60%13.
Post-Operative Rehabiltation14
The goals of the physical therapy program are given here under;
- To minimize the effusion
- Normalize gait
III. Normalize pain-free range of motion.
- Prevent atrophy of muscles, preserve its proprioception, and keep up the cardiovascular endurance.
- Exercises
– Static Quad exercises
– Straight-leg raise to the front
– Straight-leg raise to the outside
– Straight-leg raise to the back
– Hamstring curls
– Heel raise
– Heels dig bridging
– Half squat
- Patellofemoral Pain Syndrome
Patellofemoral joint pains are more common in musculoskeletal disorders in the all age groups, symptoms of which are anterior knee pain to peripatellar knee pain. In United States, Patellofemoral joint syndrome rate is around 25% of all athletes15.
Treatment:
Iceing
The Ice is used as an anti-inflammatory “medication,” however its effective use is for 10-to-20 minutes.
Taping The Knee16
Friction may be reduced by taping the patella in different positions.
Exercises17
- Static Quadriceps Contraction
- Adductor Squeeze (Supine)
- Knee Bend to Straighten
- Hip Extension in Standing
- Baker’s Cyst
it is a fluid which forms a lump at the back of knee. Baker’s cystitis also known as a popliteal cyst. The bursa can connect with the sac which supports knee bones (the synovial sac) to develop a cyst 18.
Exercises for a Baker’s Cyst19
The following exercises are commonly prescribed to patients with a Baker’s cyst.
- Knee Bend to Straighten
- Static Quadriceps Contraction
- Patellar Subluxation
Patellar subluxation occurs when the kneecap (the patella) is partly dislocated from its usual alignment inside the knee joint. Patellar tracking disorder is similar to patellar subluxation, but in this disorder the knee cap tends to be in its normal position unless the knee bends or straightens. Normally the occurrences of patellar subluxation is age group between 16 to 20 year20. This incidence was mostly seen due to sports such as soccer, gymnastics and ice hockey which accompanied with the injury involve sudden twisted of the knee20.
Physical Therapy21
- The PRICE (Protection Rest Ice Compression Evaluation)
- Quadriceps-static exercises
- Straight-leg raise
- Further, strengthening exercises should be
accomplished for hip abductors, flexors & adductors.
- Patellar bracing
- Patellar taping (McConnell method)
Post Operative Rehabilitation22
Above mentioned treatments may be included in the Rehabilitation plan after surgery, but it will necessarily take longer time to return on full mobility.
Exercises
The exercises should be started to improve the range of motion of the knee and to strengthen the supporting muscles.
- Quad Sets
- Hamstring Stretch
- Quad Stretch
- Side Leg Lift
- Straight Leg Raise
- Anterior Colleteral Ligament Injury
A force applied against the anterior thigh which drive the femur backward on tibia so that knee closes to full extension and tends to stress the ACL. It is the most frequently injured ligament which is associated with the limited range of motion23. Most of the authors have recommended that estimation of ACL repair performance is between 80,000 to 100,000 each year in United States24.
Physical Therapy25
The rehabilitation and physical therapy management
must include:
- Flexibility exercises.
- Strengthening exercises.
- Endurance activities.
- Coordination and agility training (for competitive athletes).
Post Operative Rehabilitation26
– Closed-chain exercises are used to focus on the maintenance of compete extension.
– Therapy protocols can be divided into IV phases as recommended by Shelbourne and Nitz:
Phase-I: The aim of this phase is to maintain the range of motion.
Phase-II (0 to 2 week): The aim is to reduce swelling, gain full extension & flexion up-to 90o to maintain quadriceps control.
Phase-III (3 to 5 week): Improve flexion up to full range of motion and maintain full extension. For which Bicycles& Stair- climbers may be used.
Phase-IV (6 week): Progressively coming back to sports and increase strength and agility.
- Medial Collateral Ligament Injury
The force on knee includes valgus stress and external rotation of tibia on the femur and anterior movement of the tibia on femur with torn medial capsule followed by torn MCL27.
Physiotherapy of MCL28
Grade-I & II of MCL injuries may be treated conservatively with a suitable functional rehabilitation program.
- RICE (Resting, Icing, Compression and Elevating)
- MCL Sprain Rehab:
Exercises:
Flex and extend:
Sitting, standing or lying on stomach, gently flex & extend the knee within the pain free range. Each set should have 10-20 repetitions; progress is up- to 3 sets thrice every day.
Heel slide:
Lying on back, bend the injured knee and keep the foot on the floor. Slide the heel towards the hips within the pain free range. Repeat each exercise 10-20 times.
Quad stretch:
Hold the right foot with right hand and gently pull the foot up and back towards the hips, stop when you feel the stretch. Maintain the stretched position for 10 seconds and then relax.
Hamstring stretch:
Standing, place one leg slightly in front of the other. Straighten the front knee& bend the back knee. Shift the weight on the bend knee, lean forwards until you feel a stretch in the back of the thigh. Hold for 5 to 10 seconds & then relax.
- Bracing:
A light weight hinged knee brace can be applied that will allow increase in range of motion gradually as the MCL heals.
- Posterior Cruciate Ligament (PCL) Injuries
A force during the tibia backward is applied on the femur which stresses the PCL. For example, dashboard injury: It is concluded by Schulz and his colleagues that 33% of PCL injuries were caused by sports29.
Treatment
The treatment of PCL injury can be determined by the grade of injury.
- A grade I &II injury is mostly treated with knee splinting in extension position.
- Early ROM of joint, quads & hamstring program (which is particularly eccentric)30.
- The exercises of closed chain are performed in 6 weeks.
- Hamstring exercises are postponed for 4 months to minimize the posterior load on the tibia.
- Cycling and aerobic exercise can also be beneficial for the patient and it is also useful for restoration function31.
Post-Operative Rehabilitation32
- Reestablishing knee motion.
- Reduce pain and inflammation
- Quads strengthen
- Knee brace in extension
- lliotibial Band Friction Syndrome (ITBFS)
ITBFS is an inflammatory, repetitive strain injury to the knee which is common in long distance runners33.
Physiotherapy34
Early goals of therapy are:
- To minimize the inflammation & swelling
- To increase strength & flexibility of the thigh, calf musculature, and hip.
- Mobilization of patella is used to free up joint motion.
- Electric muscle stimulation& Ultrasound combination therapy to return usual muscle tone, it also helps in healing process & decease the pain. Iontophoresis with dexamethasone is also a useful modality to decrease inflammation35.
Foam Roller (FR)
Roll affected leg over the FR and hold it for a few seconds and gradually increase time each day to mobilize tissues &break up adhesion tissue.
Single leg balance and strengthening
Start balancing on one foot during brushing the teeth. Then progressively increases the challenges with soccer ball and moving the ball in various directions.
Side leg lifts
Put back of the leg & hips beside the wall, slide the leg up towards the wall and hold for 5 seconds then slide back down.
Strengthening with Theraband
This exercise is performed for 3 to 5 times for every day for both legs.
REFERENCE
- Hengeveld E, Banks K, The Knee Complex. Maitland’s Peripheral Manipulation 4th Ed. 2005;pg 487
- Sun B, Wu C kaluain. K. New Development in Osteoarthirtis. Rheum. Disclin. Nrth Am 2007,33(I)135-48
- Cyriax J H, Cyriax P J,Theknee,Cyriax’s Illustrated Manual of Orthopaedic Medicine 2nd Ed. 1993;pg 94-95.
- Calmbach WL, Hutchens M. Evaluation of Patients Presenting with Knee Pain: Different Diagnosis, AM Fam Physician 2003;68:917–922.
- Nowinski RJ, Mehlman CT. “Hyphenated History: Osgood-Schlatter Disease”. Am J. Orthop 1998;27(8):584–5.
- El-Husseini TF, Abdelgawad AA. Results of Surgical Treatment of Unresolved Osgood-Schlatter Disease in Adults. J Knee Surg 2010;23(2):103-107.
- Gerulis V, Kalesinskas R, Pranckevicius S, Birgeris P. Importance of Conservative Treatment and Physical Load Restriction to the Course of Osgood-Schlatter’s Disease. Clinic of Pedia Surgery 2003;2(5):57-64.
- Wells L, Sehgal K. Kliegman RM, Behrman RE, Jenson HB, Stanton BF. Osgood-Schlatter Disease. Nelson Textbookof Pediatrics 19th Ed, 2011;chap 669.4.
- Blazina ME, Kerlan RK, Jobe FW, Carter VS, Carlson GJ. Jumper’s knee. OrthopClin North Am. Jul 1973;4(3):665-78.
- Witvrouw E, Bellemans J, Lysens R, Danneels L, Cambier D. Intrinsic risk factors for the development of patellar tendinitis in an athletic population. A two-year prospective study. Am J Sports Med. Mar-Apr 2001;29(2):190-5.
- Kongsgaard M, Aagaard P, Roikjaer S, et al. Decline eccentric squats increases patellar tendon loading compared to standard eccentric squats. Clin Biomech (Bristol, Avon). Aug 2006;21(7):748-54.
- Brockmeier SF, Rodeo SA. Knee: Meniscal injuries. In: DeLee JC, Drez D Jr, Miller MD, eds. DeLee and Drez’sOrthopaedic Sports Medicine. 3rd ed. Philadelphia, Pa: Saunders Elsevier; 2009:chap
- 23;sect B.
- Arendt EA, ed. Orthopaedic Knowledge Update: Sports Medicine 2. Rosemont, Ill: American Academy of Orthopaedic Surgeons; 1999.
- Brindle T, Nyland J, Johnson D. The meniscus: review of basic principles with application to surgery and rehabilitation. J Athl Train. 2001;36:160-169.
- Wieting JM, McKeag DB. Anterior knee pain and overuse. In: Sallis RE, Massimino F, eds. ACSM’s Essentials of Sports Medicine. St. Louis, Mo: Mosby-Year Book; 1997:421-32.
- Bockrath K, Wooden C, Worrell T, Ingersoll CD, Farr J. Effects of patella taping on patella position and perceived pain. Med Sci Sports Exerc. 1993;25:989–92.
- http://www.physioadvisor.com.au/8669550/patellofemoral- pain-syndrome-pfps-chondromalac.htm Biundo JJ. Bursitis, tendinitis, and other periarticular disorders and sports medicine. In: Goldman L, Schafer AI, eds. Cecil Medicine 24th Ed. Philadelphia, Pa: Saunders Elsevier; 2011:chap 271.
- http://www.physioadvisor.com.au/15266350/bakers- cyst-back-of-knee-pain-physioadvisor.html Atkin DM, Fithian DC, Marangi KS, Stone ML, Dobson BE,
- Mendelsohn C. “Characteristics of patients with primaryacute lateral patellar dislocation and their recovery within the first 6 months of injury”; Am J Sports Med 2000 28(4):472–9.
- Earl JE, Schmitz RJ, Arnold BL. Activation of the VMO and VL during dynamic mini-squat exercises with and without isometric hip adduction. J ElectromyogrKinesiol Dec 2001;11(6):381-6
- Mangine RE, Eifert-Mangine M, Burch D, Becker BL, Farag L. Postoperative management of the patellofemoral patient. J Orthop Sports PhysTher Nov 1998;28(5):323-35.
- Miyasaka KC, Danel DM, Stone ML, Hirsham P. The Incidence of Knee Ligament Injuries in the General Population. Am J Knee Surg 1991;4:3-8
- Grindstaff TL, et al. Neuromuscular control training programs and noncontact anterior cruciate ligament injury rates in female athletes: a numbers-needed-to-treat analysis. J Athl Train 2006;41(4):450–456.
- Beynnon BD, Fleming BC, Johnson RJ, et al. Anterior cruciate ligament strain behavior during rehabilitation exercises in vivo. Am J Sports Med. Jan-Feb 1995;23(1):24-34
- Shelbourne KD, Nitz P. Accelerated rehabilitation after anterior cruciate ligament reconstruction. Am J Sports Med. May-Jun 1990;18(3):292-9
- Singhal M, Patel J, Johnson D. Medical ligament injuries: 1. Medical collateral ligament injuries inadults. In: DeLee JC, Drez D Jr., Miller MD, eds. DeLee and Dree’sOrthopaedic Sports Medicine. 3rd ed. Philadelphia, Pa: Saunders Elsevier; 2009:chap23; sect C.
- Petersen W, Laprell H. Combined injuries of the medial collateral ligament and the anterior cruciate ligament. Early ACL reconstruction versus late ACL reconstruction. Arch Orthop Trauma Surg.1999;119(5–6):258–62.
- Schulz MS, Russe K, Weiler A, et al. Epidemiology of posterior cruciate ligament injuries. Arch Orthop Trauma Surg. May 2003;123(4):186-91.
- Jung YB, Tae SK, Lee YS, et al. Active non-operative treatment of acute isolated posterior cruciate ligament injury with cylinder cast immobilization. Knee Surg Sports Traumatol Arthrosc. Apr 17 2008;[Medline]
- Fanelli GC, Stannard JP, Stuart MJ, Macdonald PB, Marx RG, Whelan DB, et al. Management of complex knee ligament injuries. Instr Course Lect. 2011;60:523-35.
- Edson CJ, Fanelli GC, Beck JD.Postoperative rehabilitation of the posterior cruciate ligament. Sports Med Arthrosc. Dec 2010;18(4):275-9.
- Fredericson M, Cookingham CL, Chaudhari AM, Dowdell BC, Oestreicher N, Sahrmann S. Hip Abductor Weakness in Distance Runners with IliotibialBand Syndrome. Clinical Journal of Sport Medicine 2000;10:169-175.
- Menetrey J, Fritschy D. Subtalar subluxation in baletdancers. Am J Sports Med 1999;27(2):143-149.
- Pellecchia GL, Hamel H, Behnke P. Treatment of Infrapatellar Tendinitis: A Combination of Modalities and Transverse Friction Massage versus Iontophoresis. Journal of Sport Rehabilitation 1994;3:135-145.
