Rimsha Fatima1, Nabeela Safdar2, Somia Faisal3*, Hafiz Muhammad Asim4
1Student, Physical Therapy Department, Lahore College of Physical Therapy, LM&DC, Lahore, Pakistan![]()
2Senior Lecturer, Neurosciences Department, Lahore College of Physical Therapy, LM&DC, Lahore, Pakistan![]()
3*Demonstrator, Applied Science Department, Lahore College of Physical Therapy, LM&DC, Lahore, Pakistan![]()
4Professor, Lahore College of Physical Therapy, LM&DC Lahore Pakistan![]()
ABSTRACT
Aims of Study: The purpose of the study was to assess the functional capabilities of patients with Stage III Parkinson’s disease (PD). Functional status of PD patients declines due to impaired postural reflexes and characteristic loss of balance which became evident at Stage III thus activities of daily living (ADLs) are compromised as the severity of the disease increases.
Methodology: Descriptive case series was conducted on stage III PD patients (n=64). Patients with age ranges from 45 to 75 years were recruited and patients with other neurological issues were excluded. They were assessed using a Functional independence measure scale having reliability 0.95.
Results: Out of 64 patients, 75% required minimal assistance and 9.4% required supervision while performing the ADLs. Whereas, 81% of patients need 2 hours of personal care assistance according to burden of care.
Limitations & Future Implications: Only functional status of PD patient is determined no exercise regime or intervention were incorporated to assess their impact on the PD patient functional activities. Thus, future studies should be carried out to find the correlation between aerobic exercises and their impact on PD patient level of functional independence.
Originality: Information added was all taken from databases and reduced to similarity index and was not submitted to any other journal.
Conclusion: Stage III Parkinson’s disease patient required minimal level of assistance while performing tasks of daily living. However, majority of these patients required 2 hours of personal care assistance on average per day to compete with daily living.
Keywords: Functional status, parkinson disease, cognitive dysfunction, disease progression, orthostatic hypotension, tremors.
Introduction
Parkinson’s Disease (PD) is a progressive disease involving central nervous system (CNS) eliciting both motor and non-motor complications1. It’s the second most common degenerative disorder with neurological impairments2. It is initiated by loss of nerve cells in substantia nigra due to which brain fails to produce dopamine3. The cardinal features of this disease involve tremors, rigidity, bradykinesia, and postural instability. Secondary motor symptoms include reduction in muscle strength, muscle performance, and gait impairments4. Non-motor signs and symptoms associated are dysphagia, speech disorder, cognitive dysfunction, autonomic dysfunction, orthostatic hypotension, and sleep disorder5. It is prevalent in about 7 to 10 million people worldwide1. While in Pakistan about 450,000 people are affected with Parkinson’s disease6. It is more prevalent in males than females7. On an average 50 to 65 is the age of onset of Parkinson’s disease8.
Hoehn & Yahr (H&Y) classification scale represents the severity of Parkinson’s symptoms and disease progression9. It classifies PD into five stages following the characteristics which patient represents. Stage 1 is unilateral minimum disability, stage 2 bilateral minimum disability without impairment of balance, stage 3 impaired rightening reflex and impaired balance, stage 4 severe disability and assistance required in standing and walking, stage 5 patient confined to bed/wheelchair bound10. The lowest stage 0 is asymptomatic and in stage 5 patients became bedridden11. The modified H&Y scale defines PD severity more broadly, with stages 1 to 2 representing mild disease, stages 2.5 to 3 moderate disease, and stages 4 to 5 severe disease12.
Cognitive dysfunction is evident feature at stage III it drastically drags patients toward postural instability and balance impairment and advanced Parkinson’s disease with characteristic features of dementia, and memory impairment13. Reservation of cognition is essential for mobility and ambulation of patients as the era of disease increases14.With the progression of the disease, mobility of the patient compromises as step length and gait velocity reduces to an extent that the patient became unable to perform Activities of Daily Livings (ADL)15. The patient’s participation in activities decreases tremendously with the progression of symptoms leaving the patient in a socially isolated state16.
Most evident changes in functional capabilities occur at stage III owing to loss of balance and decreased reflexes17. Assessing the Functional status of an individual with Parkinson at an early stage would lead to a better rehabilitation protocol strategy18. When physical therapy interventions are used early in the course of Parkinson’s disease, the disease’s progression can be slowed down, which reduces the burden of the disease and its impairments on society19.
The rationale of the current study is to assess the functional status of patients with stage III Parkinson’s disease so that appropriate preventive and rehabilitative measures can be incorporated at this stage which will helps to preserve the maximal level of functioning and slow down the advancement of the disease.
Methodology
It was a descriptive case series, n=32 subjects were recruited from the following hospitals of Lahore; Ghurki Trust Teaching Hospital, Jinnah Hospital and Neurology department of Mayo Hospital. The duration of study was from June 2020 to January 2021. The sampling technique used was non-probability convenience sampling. The study was approved by the ethical board of Lahore College of physical therapy LCPT/DPT/16/631. The inclusion criteria were clinically diagnosed subjects of Parkinson Disease at Stage III (Hoehn & Yahr) scale with age ranges from 45 to 75 years that is middle aged and elderly individuals. Patients with other neurological issues were excluded from the study. Written informed consent was taken from each patient prior to study. The patients were assessed using a Functional independence measure (FIM) scale having inter-rater reliability of 0.9520. It contains 18 items composed of 13 motor tasks and 5 cognitive tasks and tasks are rated on 7-point ordinal scale that ranges from total assistance to complete independence. The total score for the FIM motor subscale (the sum of the individual motor subscale items) will be a value between 13 and 91; whereas, cognition subscale (the sum of the individual cognition subscale items) will be a value between 5 and 35. Hence, the total score for the FIM instrument (the sum of the motor and cognition subscale scores) will be a value between 18(lowest) and 126(highest). Thus, FIM is used to assess and grade the functional status of a person based on the level of assistance he or she requires. The inter-rater reliability of FIM ranged from 0.93 to 0.97, while the intra-rater was 0.99 for the motor, cognitive and total FIM score. Cronbach alpha coefficients were 0.97 and 0.95 respectively for the motor and cognitive scores21. Data was analyzed by using SPSS version 21 descriptive statistics were reported and variables are presented in the form of frequencies and percentages.
Results
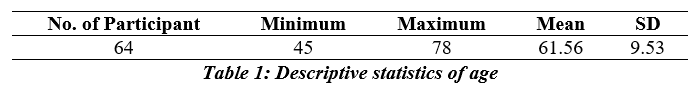
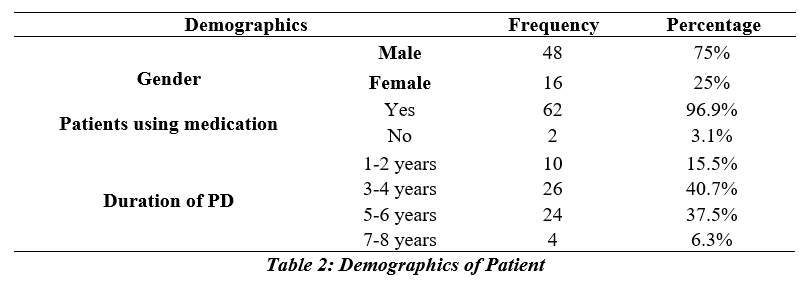
Out of 64 participants, the minimum age of participants was 45 years; maximum age 78 years with a mean age was of 61.56 and standard deviation (SD) of 9.53 as shown in table 1. Whereas, 75% (n=48) were males and 25% (n=16) were females.
About, 96.9% (n=62) participants were taking medication for Parkinson’s disease and 40.7% (n=26) were suffering from Parkinson’s disease from last 3-4 years as shown in table 2.
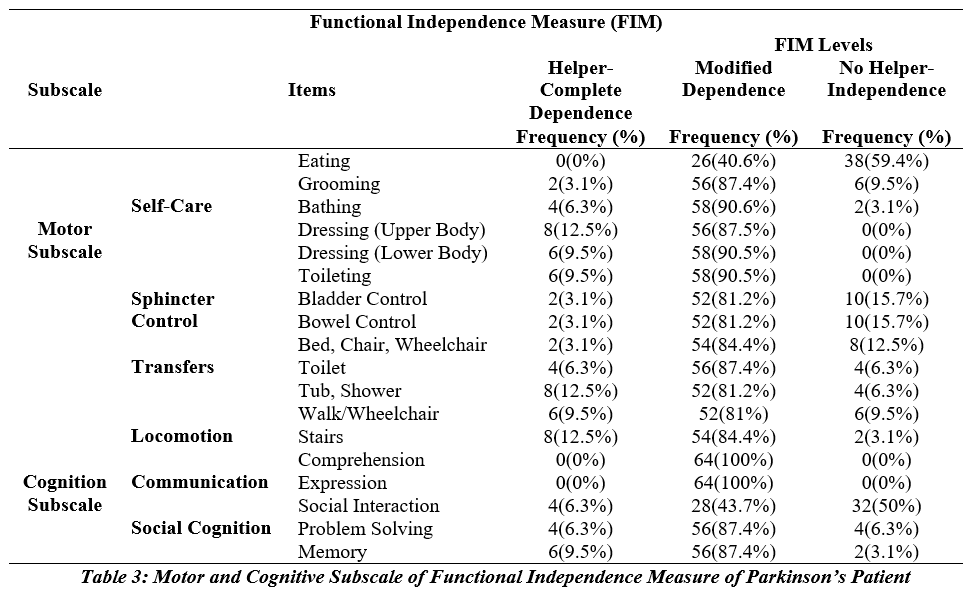
Functional status of patient assessed with FIM shows that in motor activities subjects requires assistance or modified dependency in self-care, sphincter control, transfer and locomotion. Eating being the easiest motor task of self-care as 59.4% patients showed moderate independence to complete independence while in stair climbing reported to be a difficult motor task as 84.4% patients required moderate assistance or modified dependency in it. In FIM Cognition subscale the communication task patient need supervision in comprehension and assistance in expression which mean somehow dependency. In social cognition component memory recalling is difficult as 87.4% patients require moderate assistance. Hence, functional status of Parkinson disease at stage Stage III (Hoehn & Yahr) had been shown in table 3.
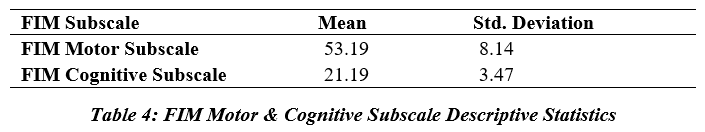
FIM motor subscale total score shows a mean value 53.19 and SD 8.14 and FIM cognitive subscale total score mean was 21.19 and SD 3.47 as shown in Table 4.
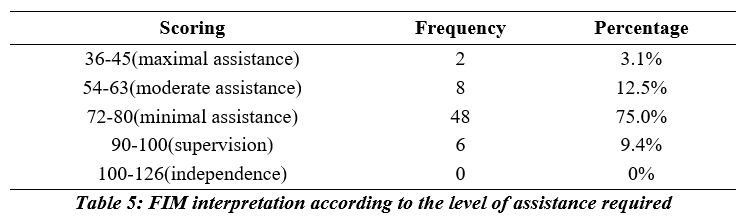
According to the frequency analysis, out of 64 patients, 75% (n=48) required minimal assistance in tasks of their daily life and 9.4% (n=6) required supervision. Whereas, 12.5% (n=8) required moderate assistance and 3.1% (n=2) required maximal assistance in ADLs.
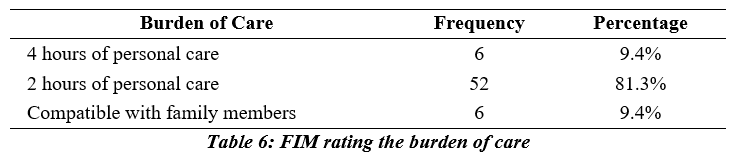
However, 2 hours of personal care assistance is needed per day by 81.3% participants with PD to compete with daily living.
Discussion
The purpose of the study was to analyze the functional status of patients, hours of care and level of assistance a patient need in stage III of PD by using FIM (functional independence measure) questionnaire so that appropriate preventive and rehabilitative measures can be incorporated by the physical therapist at this stage which will helps to preserve the maximal level of functioning and slow down the advancement of the disease. In 2019, Paul, Chuang, et al. conducted a study to find association between lifestyle factors and Parkinson’s disease progression. He concluded that lifestyle elements decrease the rate of progression of disease22. Macchi, Koljack, et al. in 2019 elaborated that patient and caregiver factors lead to caregiver burden in individuals with PD23. Moreover, in 2019 Feigin et al conducted a systematic analysis and interpreted that neurological burden increases with age and needs to develop prevention and treatment strategies24. Hence, in current study it was found that with the progression of the disease to stage III Burden of care increases.
In 2019, Pelicioni, Menant et al. performed a study on ‘Falls in Parkinson’s Disease Subtypes’ he concluded that patients with Postural Instability and Gait Difficulty are at greater risk of falls owing to functional impairments25. The current study demonstrates that patients with Parkinson’s disease suffer postural difficulties with growing age as the disease progress to stage III, balance impairment starts to prevail. Hence, compared to stages 1 and 2 assistance is required by patients at stage III to accomplish their ADLs. Therefore, it elaborates need for preventive measures to slow down the disease progression.
In 2018, Gupta, Fahn, et al. hypothesized that Hoehn and Yahr scale can be used globally for the assessment of posture, balance, stability, and other movement disorders26. Moreover, Ladislav K Valach et al. in 2017 conducted an observational study indicating the usefulness of FIM in monitoring the patients with PD27. However, in current study patient at stage III of Hoehn and Yahr scale were recruited and functional status of patients were assessed with FIM scale. The study revealed that minimal assistance is required in self-care; moderate to minimal assistance is required in sphincter control, minimal assistance in transfers, and moderate to minimal assistance in locomotion tasks.
In 2017, Yumiko Kaseda et al. conducted a study on the Therapeutic effects of intensive inpatient rehabilitation in advanced Parkinson’s disease and found FIM motor average value 52-63, FIM cognitive average value 26-27.6, and total FIM score of 78-9028. In the current study, it was concluded that at stage III patients with Parkinson’s disease require minimal assistance to accomplish activities of daily living revealing a consistency of results with the previous study.
In 2021 Yang Li et al. conducted a systemic review to assess the efficiency of aerobic exercise among Parkinson’s disease patients and concluded that moderate aerobic exercise improves balance and gait in PD patients. Exercise of various kinds has diverse effects on PD patients’ quality of life. It is imperative to systematize the exercise program additionally29. Whereas, in the current study only the functional status of PD patient and their level of assistance is determined no exercise regime or intervention were incorporated to assess their impact on the PD patient functional activities.
Thus, it is recommended that future studies should carried out to find the correlation between aerobic exercises and their impact on PD patient level of functional independence.
Conclusion
According to the results of this study, it was reported that patients with Stage III Parkinson’s disease required minimal level of assistance while performing tasks of daily living. However, majority of these patients required 2 hours of personal care assistance on average per day to compete with activities of daily living.
AUTHORS’ CONTRIBUTION:
The following authors have made substantial contributions to the manuscript as under:
Conception or Design: Rimsha Fatima
Acquisition, Analysis or Interpretation of Data: Somia Faisal
Manuscript Writing: Nabeela Safdar
Approval: Hafiz Muhammad Asim
All authors acknowledge their accountability for all facets of the research, ensuring that any concerns regarding the accuracy or integrity of the work are duly investigated and resolved.
ACKNOWLEDGEMENTS: The authors thank the Dean of Lahore College of Physical Therapy for his endless support and guidance.
INFORMED CONSENT: (dealing with studies involving human subjects.) Written informed consent from the participants was obtained before inclusion in the study.
CONFLICT OF INTEREST: None
FUNDING STATEMENTS: None
ETHICS STATEMENTS: The protocol of the present study was registered by the local ethics committee of Lahore College of Physical Therapy LCPT/DPT/16/631.
References
- Feng H, Li C, Liu J, Wang L, Ma J, Li G, Gan L, Shang X, Wu Z. Virtual reality rehabilitation versus conventional physical therapy for improving balance and gait in Parkinson’s disease patients: a randomized controlled trial. Medical science monitor: international medical journal of experimental and clinical research. 2019;25: pp 4186.
- Abbas MM, Xu Z, Tan LC. Epidemiology of Parkinson’s disease—East versus West. Movement disorders clinical practice. 2018 Jan;5(1): pp 14-28.
- Minić I, Pejčić A, Popović S. Link between periodontal inflammatory disease and Parkinson’s disease. GSC Advanced Research and Reviews. 2020;5(2): pp 84-88.
- Zhao P, Zhang B, Gao S, Li X. Clinical features, MRI, and 18F‐FDG‐PET in differential diagnosis of Parkinson disease from multiple system atrophy. Brain and Behavior. 2020 Nov;10(11): pp e01827.
- Filippi M, Elisabetta S, Piramide N, Agosta F. Functional MRI in idiopathic Parkinson’s disease. International review of neurobiology. 2018;141: pp 439-467.
- Imtiaz N, Mehreen S, Saeed K, Akhtar N, Ur H, Rehman SA, Rehman AU, Ali J, Ayub M. Study of prevalence of Parkinson’s disease in elderly population in Rawalpindi, Pakistan. Pakistan. J. Entomol.Zool Stud. 2016; 4(6): pp 845-847.
- Durcan R, Wiblin L, Lawson RA, Khoo TK, Yarnall AJ, Duncan GW, Brooks DJ, Pavese N, Burn DJ, ICICLE‐PD Study Group. Prevalence and duration of non‐motor symptoms in prodromal Parkinson’s disease. European journal of neurology. 2019 Jul; 26(7): pp 979-985.
- Cerri S, Mus L, Blandini F. Parkinson’s disease in women and men: What’s the difference? Journal of Parkinson’s disease. 2019 Jan 1; 9(3): pp 501-515.
- Tsiouris KM, Rigas G, Antonini A, Gatsios D, Konitsiotis S, Koutsouris DD, Fotiadis DI. Mining motor symptoms UPDRS data of Parkinson’s disease patients for the development of Hoehn and Yahr estimation decision support system. In 2017 IEEE EMBS International Conference on Biomedical & Health Informatics (BHI) 2017 Feb 16: pp 445-448. IEEE.
- Fine EM, Meier A, Serbin M, Stahl M, Dabbous F. Parkinson’s Disease Burden by Hoehn and Yahr Stage Using Real-World Data from the Parkinson’s Outcomes Project (4183) 2021.
- Chatterjee N. Automatic Classification of Parkinson’s Disease Based on Severity Estimation. Proceedings of the 1st International Conference on Data Science, Machine Learning and Applications 2020 May 19; 601: pp 190.
- Kahn L, Mathkour M, Lee SX, Gouveia EE, Hanna JA, Garces J, Scullen T, McCormack E, Riffle J, Glynn R, Houghton D. Long-term outcomes of deep brain stimulation in severe Parkinson’s disease utilizing UPDRS III and modified Hoehn and Yahr as a severity scale. Clinical neurology and neurosurgery. 2019 Apr 1; 179: pp 67-73.
- Weil RS, Winston JS, Leyland LA, Pappa K, Mahmood RB, Morris HR, Rees G. Neural correlates of early cognitive dysfunction in Parkinson’s disease. Annals of clinical and translational neurology. 2019 May; 6(5): pp 902-912.
- Wang CY, Chan L, Wu D, Chi WC, Yen CF, Liao HF, Hong CT, Liou TH. Effect of cognitive disability and ambulation status on functioning in moderate-to-advanced Parkinson disease. Frontiers in Neurology. 2020 Jan 9; 10: pp 1360.
- Mirelman A, Ben Or Frank M, Melamed M, Granovsky L, Nieuwboer A, Rochester L, Del Din S, Avanzino L, Pelosin E, Bloem BR, Della Croce U. Detecting Sensitive Mobility Features for Parkinson’s Disease Stages Via Machine Learning. Movement Disorders. 2021 Sep; 36(9): pp 2144-2155.
- Kanegusuku H, Ritti-Dias RM, Barbosa PY, das Neves Guelfi ET, Okamoto E, Miranda CS, de Paula Oliveira T, Piemonte ME. Influence of motor impairment on exercise capacity and quality of life in patients with Parkinson disease. Journal of Exercise Rehabilitation. 2021 Aug; 17(4): pp 241.
- Palakurthi B, Burugupally SP. Postural instability in Parkinson’s disease: a review. Brain sciences. 2019 Sep 18;9(9): pp 239.
- Kotagal V, Bohnen NI, Müller ML, Frey KA, Albin RL. Cerebral amyloid burden and Hoehn and Yahr stage 3 scoring in Parkinson’s disease. Journal of Parkinson’s disease. 2017;7(1): pp 143-147.
- Santos P, Machado T, Santos L, Ribeiro N, Melo A. Efficacy of the Nintendo Wii combination with Conventional Exercises in the rehabilitation of individuals with Parkinson’s disease: A randomized clinical trial. NeuroRehabilitation. 2019 Jan 1; 45(2): pp 255-263.
- Brosseau L, Wolfson C. The inter-rater reliability and construct validity of the Functional Independence Measure for multiple sclerosis subjects. Clinical Rehabilitation. 1994 May;8(2): pp 107-115.
- Gkouma A, Theotokatos G, Geladas N, et al. Validity and Reliability Evidence of the Functional Independence Measurement (FIM) for individuals with Neurological Disorders in Greece. J Med – Clin Res & Rev. 2022; 6(5): pp 1-11.
- Paul KC, Chuang YH, Shih IF, Keener A, Bordelon Y, Bronstein JM, et al. The association between lifestyle factors and Parkinson’s disease progression and mortality. Movement Disorders. 2019;34(1): pp 58-66.
- Macchi ZA, Koljack CE, Miyasaki JM, Katz M, Galifianakis N, Prizer LP, Sillau SH, Kluger BM. Patient and caregiver characteristics associated with caregiver burden in Parkinson’s disease: a palliative care approach. Ann Palliat Med. 2020 Feb 1; 9: pp 24-33.
- Feigin VL, Nichols E, Alam T, Bannick MS, Beghi E, Blake N, et al. Global, regional, and national burden of neurological disorders, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. The Lancet Neurology. 2019;18(5): pp 459-480.
- Pelicioni PH, Menant JC, Latt MD, Lord SR. Falls in Parkinson’s disease subtypes: risk factors, locations and circumstances. International journal of environmental research and public health. 2019;16(12): pp 2216.
- Gupta DK, Fahn S, Tatsuoka C, Kang UJ. Hoehn and Yahr stage 3 and postural stability item in the movement disorder society–unified Parkinson’s disease rating scale. Movement Disorders. 2018;33(7): pp 1188-1189.
- Valach L, Selz B. Rehabilitation Programs monitored by Functional Independence Measure: An Observational Study. Int Phys Med Rehab J. 2017;2(1): pp 00039.
- Kaseda Y, Ikeda J, Sugihara K, Yamawaki T, Kohriyama T, Matsumoto M. Therapeutic effects of intensive inpatient rehabilitation in advanced Parkinson’s disease. Neurology and clinical neuroscience. 2017;5(1): pp 18-21.
- Li Y, Song H, Shen L, Wang Y. The efficacy and safety of moderate aerobic exercise for patients with Parkinson’s disease: a systematic review and meta-analysis of randomized controlled trials. Ann Palliat Med. 2021 Mar 1;10(3): pp 2638-2649.
The Ziauddin University is on the list of I4OA, I4OC, and JISC.
This is an open- access article distributed under the terms of the Creative Commons Attribution License (CC BY 4.0).
