ABSTRACT
OBJECTIVE
In this particular systematic review, the researcher evaluates the impact of visceral mobilization or manipulation in improving low back pain via standard protocols.
MATERIALS AND METHODS
Literature was searched electronically on various databases such as PEDro, PubMed Central, Google Scholar, BioMed Central, MEDLINE, EMBASE and Science Direct considering duration of 2011 to 2019. Randomized Controlled Trials investigating effectiveness of visceral manipulation or mobilization, either, in the comparison with different modalities or with sham/placebo were included. Data was extracted and studies were reviewed on standardized qualitative assessment criteria. Cochrane guidelines were followed to find out the risk of bias among the particular research.
RESULTS
All the studies provided moderate to high quality evidence in favor of visceral mobilization or manipulation being effective on low back pain in terms of risk of bias and quality assessment with significant results (p-value <0.05).
CONCLUSION
The available studies provided the significant and strong effectiveness of visceral manipulation and mobilization. However, scarcity of literature in domain raises an inevitable need for further studies to be conducted in future.
This is an open-access article distributed under the terms of the Creative
Commons Attribution Licence (CC BY) 4.0 https://creativecommons.
KEYWORDS
Viscera, Mobilization, Low back pain, Quality of life, Sham, Pain.
Mirza M. Zeeshan Saeed
Physiotherapist
SIUT
Nabeel Baig
Assistant Professor
Ziauddin College of Rehabilitation
Sciences
Muhammad Ather Hashmi
Lecturer
Ziauddin College of Rehabilitation
Sciences
[Mirza MZS, Baig N, Hashmi MA Visceral Mobilization as Management Option for Low Back Pain-A Systematic Review.Pak.j.rehabil.2020:9(2);4-10}
DOI:10.36283/pjr.zu.9.2/003
LBP – Low Back Pain, is among the commonest pathological problems and it is more associated with comorbidity and disability than any other condition1,2. The pervasiveness of low back pain globally is reported 7.5% at 95% confidence interval that is higher in females as compared to males3. Approximately, about 80% of the population suffered from low back pain in their life span4. Statistical reports of United States suggest that every 1 individual out of 4 adults is reported to have suffered with low back pain almost every day, in last 3 months4. However, in most researches, age is regarded as the commonest contributing factor of low back pain5. Moreover, it is suggested that the incidence of low back pain increases tremendously, after 60-65 years of age6. Furthermore, statistics show that an increased pervasiveness of low back pain is also related with the patient’s educational and socioeconomic statuses7. People with low educational status are predicted to suffer more prolonged episodes of low back pain and have a poor prognosis8. In other researches, LBP is the termed as an inconvenient condition to be managed for clinicians, patients, and policy makers9. Although, low back pain is equally prevalent among the individuals of all age groups and hinder daily aspects of their life10. However, its consequences badly affect the elderly population11. Researchers suggest that visceral dysfunction may be the underlying etiology of low back pain or contribute as the aggravating factor for it12. There are various approaches prevailed for the management of LBP, but preceding studies demonstrates visceral mobilization might be beneficial for the treating low back pain13. A recently conducted clinical case series demonstrate that the symptoms of low back pain were improved following a specific visceral manipulation technique in which a mobilization maneuver on the kidneys in people with nonspecific low back pain13. Studies show that specific visceral disorders, such as refractory irritable bowel syndrome and chronic constipation in women found good outcomes after visceral techniques on patient with Low back pain14. In asymptomatic individuals with chronic Low back pain do not reach the flexion relaxation phenomena, which is decrease in or absence of electromyography activity in paraspinal muscles found at the time of full trunk flexion15. The rational of this particular therapeutic study is that visceral disorders could potentially cause LBP14. The central sensitization activated by visceral nociceptors, these receptors trigger by alter gut environment/ urinary motility and these visceral receptor evoke peripheral hypersensitivity 15. This is not yet understood the mechanism of visceral manipulation have effect on pain15. Hypothesis reveals that the supportive layers below skin that surrounds internal space of fissures of trunk and visceral nociceptive signaling is modulated by visceral manipulation and specific manual treatments14. Over decades, the treatment for LBP is intuitive manipulation has been utilized for about last ten years almost in LBP treatment, but its efficacy is still unproven14. The mechanism of visceral pain referral to somatic structures occurs by neural merging, from where sympathetic afferent nerves conveys signal to visceral join with somatic nerves in the dorsal horn14. Just because of low intensity of visceral receptors it fails to bring mindful sensitivity, viscera nociceptive input can be misjudged as ascending from body (soma) structures14 Evidence shows that people with low back pain has neuromuscular deficit in spine15.
The guidelines of Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) were followed for this systematic review.
Databases and Eligibility Criteria
Literature was searched electronically on various databases such as PEDro, PubMed Central, Google Scholar, BioMed Central, MEDLINE, EMBASE and Science Direct considering duration of 2011 to 2019. The retrieval strategies were utilized in order to perform article search include keywords, MeSH terms with use of Booleans such as “Visceral Mobilization AND low back pain”, “Visceral mobilization AND LBP”, “Visceral Mobilization and Manipulation”, “VM AND LBP”.
Eligibility of Studies
Randomized Control Trials investigating effectiveness of visceral manipulation or mobilization, either, in the comparison with different modalities or with sham/placebo from 2011 to 2019 were included. The flow of studies is represented in Figure-1.
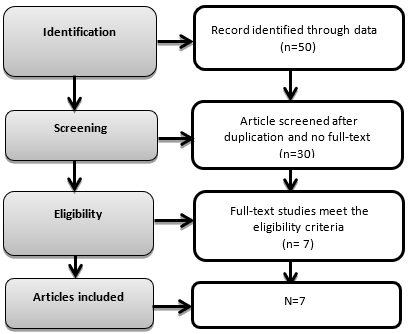
Figure.1 Flow of Studies according to PRISMA
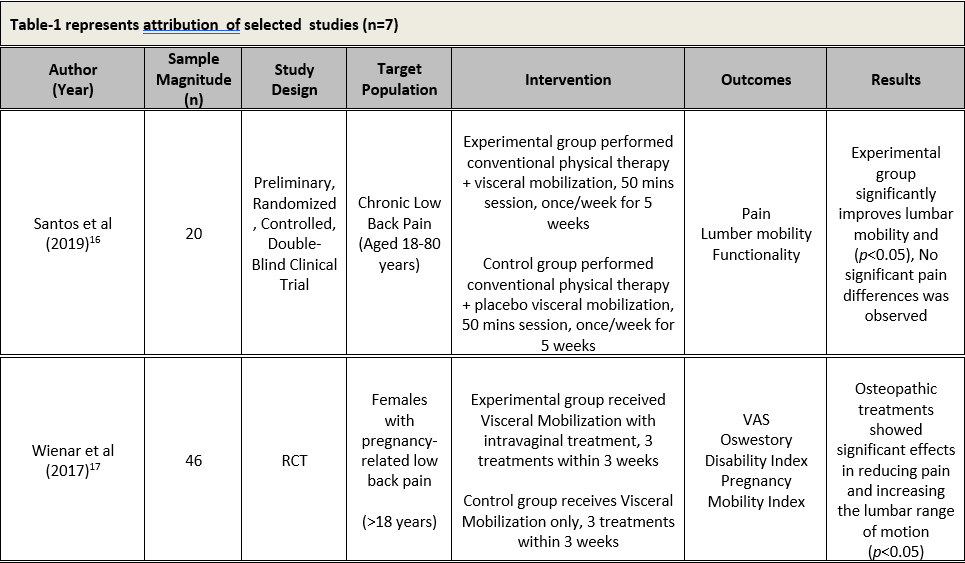
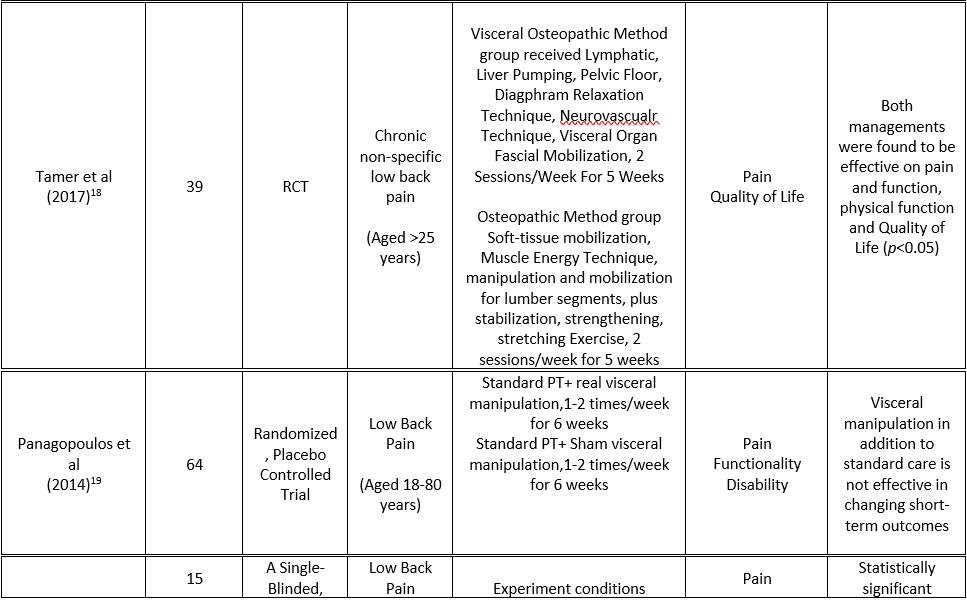
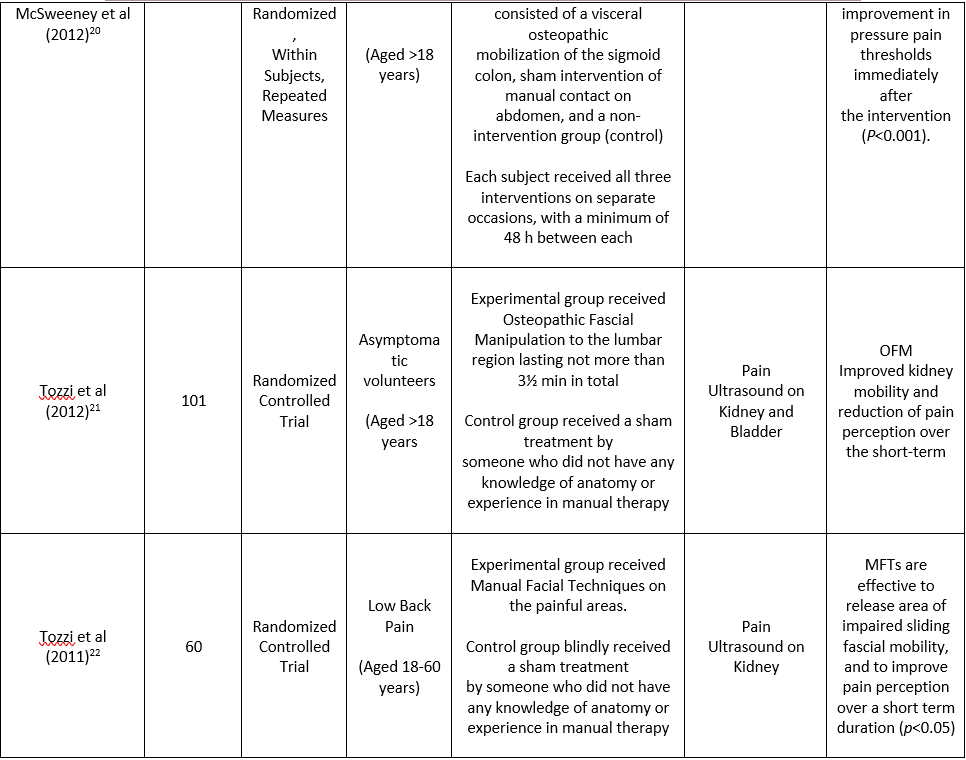
Study Characteristics
Among included studies, six were randomized control trials; however one is randomized placebo controlled trial. These studies recruited participants ranging from asymptomatic to those having chronic low back pain and even pregnant females with low back pain. Moreover, six studies compared the effects of visceral mobilization/manipulation with sham or placebo; but one study compared visceral mobilization with a combination of visceral mobilization and an intravaginal treatment maneuver. Table 1 represents the study characteristics of included researches.
Outcome Measures
All studies considered perception of pain as the primary outcome measure. Secondary outcome measures consisted of quality of life, functionality, pregnancy mobility index, disability index and ultrasound.
Extraction and Management
Data was extracted and analyzed according as per the criteria designed for induction of study. Studies comparing the role of visceral mobilization/ manipulation and other manual therapy modalities on LBP either in combination of traditional/conventional physical therapy or as the sole treatment strategy were included. Few of the researches that fails to fulfill criteria of inclusion were excluded from this review such as the studies examining the effects of visceral manipulation of cervical spine or bowel movements. Moreover, outcomes measures of these studies included pain, disability index, mobility while pregnancy and quality of life. Considering the standardized
protocols, all data were collected in a structured table in order to maintain the accuracy and validity of data. A standardized table was formulated to categorize the researches on the basis of first author’s name, sample size, target population, provided intervention, outcome measures and results of each specific study that is represented as Table-1.
Selection of Articles
A total of 50 research articles were retrieved from various databases including such as PEDro, PubMed Central, Google Scholar, BioMed Central, MEDLINE, EMBASE and Science Direct published between the duration of 2011 to 2019. Considering the inclusion criteria, only seven studies were included. Data was extracted and quality assessment was performed using standardized protocol of PRISMA guidelines. However, due to heterogeneity among the selected articles and their outcomes measures meta-analysis could not be performed.
Synthesis of Studies
All outcomes measures were assessed for each study with the interventions applied in order to examine the impact of visceral mobilization in improving low back pain as the primary outcome as well as functionality and quality of life. Conclusively, researches including Tamer et al18 and Santosa et al16 demonstrated significant difference in pain among the participant that received Visceral manipulation either in combination or alone with the p-value=0.9 . Panagoloulos et al19 found no significant effect of visceral mobilization in between the group analysis. However, pain levels significantly decreased within both groups after visceral mobilization with or without vaginal maneuvers with p-value <0.05. Similar improvement was found for Pregnancy-Mobility Index (PMI) and Oswestry Disability Index. Therefore, this study affirmed the impact of visceral mobilization. Moreover, Panagoloulos et al19 revealed non-significant impact of visceral mobilization in short term i.e. duration of 2 weeks, however, significant impact on 52 weeks. Thus, this advocated the effectiveness of long term application of visceral mobilization in improving low back pain. Furthermore, McSweeney et al. 201220 came up with the significant improvement in low back pain among experimental group that received visceral mobilization specifically mobilization of sigmoid colon. Consecutively, Tozzi et al 21,22 concluded that Manual Fascial Techniques and Osteopathic Manipulation are effective to relief area of reduced sliding fascial mobility, and to reduce pain perception for immediate duration in subjects with non-specific LBP. All the outcomes are represented in Table 2.
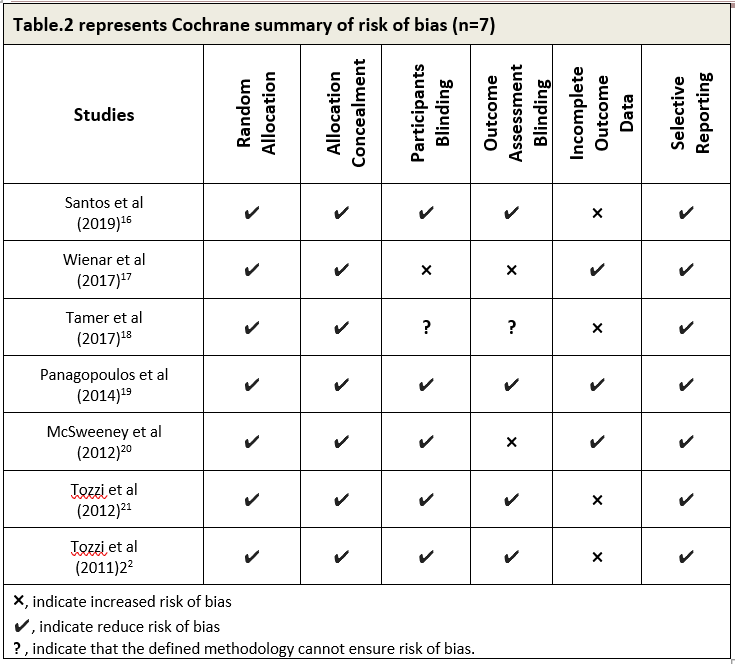
Risk of Bias and Overall Study Quality
Cochrane’s standardized checklist was used to identify the overall risk of biasness of the studies included in this paper as represented in Table-3.
Selection Bias
Random Sequence Generation
According to the author’s judgment, random Sequence generation of all seven studies 16,17,18,19,20,21,22 included in the systematic review demonstrated low random risk generation.
Allocation Bias
Similarly all included papers 16,17,18,19,20,21,22 displayed low risk of allocation concealment.
Presentation Bias
Blinding of Participants and Personnels
Assessment revealed that Santosa et al16, Panagopoulos et la14 and Mcsweeney20 reported low risk of bias.
However, study of Weisner et al17 showed high risk of bias while a single study Tamer et al18 provided no information regarding blinding of participant and personnel.
Exposure Bias
Blinding of Result Assessment
Three studies14,16,20 reported low risk of bias. However, one study17showed high and one 18 showed unknown risk of bias.
Attrition Bias
Incomplete Outcome Data
Three out of five studies14,17,20 reported the loss to follow-up data and incomplete outcome data. However, studies of Tamer et al 18 and Santosa et al16found to commit attrition bias.
Reporting Bias
Selective Reporting
All the included studies 16,17,18,19,20,21,22 showed low risk of selective reporting.
The selected all studies were done on effects of visceral mobilization in low back pain. In all articles there were not specified the specific area of the pain in lower back16-22. One study did not mention the complete results of their studies. In our study pain intensity was reduced in both OMT and VOMT groups. In placebo controlled, assessors- blinded clinical trial explained the effects of OVM program in 6th week. We believed that visceral applications have a great impact in low back pain patients. Different physiotherapy techniques such as spinal mobilization and fascial releasing techniques have big impact in reducing low back pain23-24. We think, visceral fascial limitation provoking the pain in lumber segment. We concluded from one study that a specific abdominal viscera such as sigmoid colon mobilization reduces the low back pain12. We concluded that duration and means restrict the outcome in a smaller sample magnitude that actually limits the importance of outcomes. Viscera’s manipulation has limited hypoalgesic effects in LBP, but this difference might also demonstrated because in our research we use visceral manipulation in combination with standard care. The outcomes and physical relevance of these studies will be vital, not only for researchers and policy makers, but it’s also for patients who suffering from nonspecific low back pain and functional constipation23-25. In some studies therapist will not be blinded which is the limitation. In one study it was concluded the results at the end of the sixth week, in which a total of 10 sessions were applied being two sessions per week. But there were some limitations in the review, as most of the studies has a smaller sample size and short term follow up of control groups. Also the studies did not cover different physical therapy methods that included functional and objective evaluation are the limitation of this study. There were no remarkable adverse effects were reported by the participants in any of included study. However, the most common complaint includes discomfort after intervention and no serious adverse effect was reported21.
It was concluded that effects of visceral mobilization in low back pain is significant, provided moderate to high quality evidence upon the effectiveness of visceral manipulation/ mobilization with low to medium risk of bias however the segment was not filtered among the studies.
- Hartvigsen J, Hancock MJ, Kongsted A, Louw Q, Ferreira ML, Genevay S, Hoy D, Karppinen J, Pransky G, Sieper J, Smeets RJ. What low back pain is and why we need to pay attention. The Lancet. 2018;391(10137):2356-67.
- Hoy D, March L, Brooks P, Blyth F, Woolf A, Bain C, Williams G, Smith E, Vos T, Barendregt J, Murray C. The global burden of low back pain: estimates from the Global Burden of Disease 2010 study. Annals of the rheumatic diseases. 2014;73(6):968-74.
- Wu A, March L, Zheng X, Huang J, Wang X, Zhao J, Blyth FM, Smith E, Buchbinder R, Hoy D. Global low back pain prevalence and years lived with disability from 1990 to 2017: estimates from the Global Burden of Disease Study 2017. Annals of Translational Medicine. 2020 ;8(6).
- Patrick N, Emanski E, Knaub MA. Acute and chronic low back pain. Medical Clinics. 2014 ;98(4):777-89.
- Wong AY, Karppinen J, Samartzis D. Low back pain in older adults: risk factors, management options and future directions. Scoliosis and spinal disorders. 2017;12(1):14.
- Cruz-Díaz D, Martínez-Amat A, Manuel J, Casuso RA, de Guevara NM, Hita-Contreras F. Effects of a six-week Pilates intervention on balance and fear of falling in women aged over 65 with chronic low-back pain: A randomized controlled trial. Maturitas. 2015;82(4):371-6.
- Williams JS, Ng N, Peltzer K, Yawson A, Biritwum R, Maximova T, Wu F, Arokiasamy P, Kowal P, Chatterji S. Risk factors and disability associated with low back pain in older adults in low-and middle-income countries. Results from the WHO Study on Global AGEing and Adult Health (SAGE). PLoS One. 2015 10(6):e0127880.
- Karran EL, McAuley JH, Traeger AC, Hillier SL, Grabherr L, Russek LN, Moseley GL. Can screening instruments accurately determine poor outcome risk in adults with recent onset low back pain? A systematic review and meta-analysis. BMC medicine. 2017;15(1):13.
- Foster NE, Anema JR, Cherkin D, Chou R, Cohen SP, Gross DP, Ferreira PH, Fritz JM, Koes BW, Peul W, Turner JA. Prevention and treatment of low back pain: evidence, challenges, and promising directions. The Lancet. 2018;391(10137):2368-83.
- Ramdas J, Jella V. Prevalence and risk factors of low back pain.2018
- Wong AY, Karppinen J, Samartzis D. Low back pain in older adults: risk factors, management options and future directions. Scoliosis and spinal disorders. 2017;12(1):14.
- Switters JM, Podar S, Perraton L, Machotka Z. Is visceral manipulation beneficial for patients with low back pain? A systematic review of the Int J Osteopath Med. 2019;33:16-23.
- Zollars JA, Armstrong M, Whisler S, Williamson S. Visceral and neural manipulation in children with cerebral palsy and chronic constipation: five case reports. Explore. 2019;15(1):47-54.
- Manchikanti L, Singh V, Falco FJ, Benyamin RM, Hirsch JA. Epidemiology of low back pain in adults. Neuromodulation: Technology at the Neural Interface. 2014;17:3-10.
- Childs JD, Fritz JM, Wu SS, Flynn TW, Wainner RS, Robertson EK, Kim FS, George SZ. Implications of early and guideline adherent physical therapy for low back pain on utilization and costs. BMC health services research. 2015;15(1):150.
- Santos LV, Córdoba LL, Lopes JB, Oliveira CS, Grecco LA, Andrade AC, Neto HP. Active Visceral Manipulation Associated With Conventional Physiotherapy in People With Chronic Low Back Pain and Visceral Dysfunction: A Preliminary, Randomized, Controlled, Double-Blind Clinical Trial. J Chiropr Med 2019;18(2):79-89.
- Wiesner A, Guenther-Borstel J, Liem T, Ciranna-Raab C, Schmidt T. Osteopathic intravaginal treatment in pregnant women with low back pain. In International Urogynecology Journal 2017 (Vol. 28, Pp. S115-S115). 236 Grays Inn Rd, 6th Floor, London Wc1x 8hl, England: Springer London Ltd.
- Tamer S, Öz M, Ülger Ö. The effect of visceral osteopathic manual therapy applications on pain, quality of life and function in patients with chronic nonspecific low back pain. Journal of back and musculoskeletal rehabilitation. 2017 ;30(3):419-25.
- Panagopoulos J, Hancock MJ, Ferreira P, Hush J, Petocz P. Does the addition of visceral manipulation alter outcomes for patients with low back pain? A randomized placebo controlled trial. Eur J Pain2015;19(7):899-907.
- McSweeney TP, Thomson OP, Johnston R. The immediate effects of sigmoid colon manipulation on pressure pain thresholds in the lumbar spine. Journal of bodywork and movement therapies. 2012;16(4):416-23.
- Tozzi P, Bongiorno D, Vitturini C. Fascial release effects on patients with non-specific cervical or lumbar pain J Bodyw Mov Ther. 2011;15(4):405-16.
- Tozzi P, Bongiorno D, Vitturini C. Low back pain and kidney mobility: local osteopathic fascial manipulation decreases pain perception and improves renal mobility. J Bodyw Mov Ther2012;16(3):381-91.
- Fernandes WV, Blanco CR, Politti F, de Cordoba Lanza F, Lucareli PR, Corrêa JC. The effect of a six-week osteopathic visceral manipulation in patients with non-specific chronic low back pain and functional constipation: study protocol for a randomized controlled trial. Trials. 2018;19(1):151.
- Degenhardt BF, Johnson JC, Brooks WJ, Norman L. Characterizing adverse events reported immediately after osteopathic manipulative treatment. J Am Osteopath Assoc 2018;118(3):141–9.
- Slattengren AH, Nissly T, Blustin J, Bader A, Westfall E. Best uses of osteopathic manipulation J Fam Pract 2017;66(12):743-8.
