ABSTRACT
BACKGROUND AND AIMS
Patient safety has been neglected in the rehabilitation as per many of the studies, there is a surge demand to get acquainted with the knowledge of patient safety for quality and reliable care. This study aimed to explore the attitude and preferences of rehab sciences students about patient safety and quality improvement education to overcome the gaps in practice regarding patient safety.
METHODOLOGY
A cross-sectional survey was conducted on undergraduate medical students of physical and occupational therapy, on convenience sampling technique. Data was collected through WhatsApp and e-mail on self-administered questionnaire formulated on google document, based on attitude and preferences of patient safety and quality improvement education.
RESULTS
A total number of 134 responses received out of which 56.7% were occupational therapy (OT) and rest physical therapy (PT) student. 67.9% OT and 79.9% PT have rated their current knowledge of patient safety and quality improvement as an average. Moreover, students believe that 97.8% good communication, 98.5% patient participation and motivation and 96.3%multidisciplinary teamwork plays a vital role in reducing risk of error. Consecutively, 95.5% of students encourage the safety measurement and quality practice should be an objective of undergraduate curriculum.
CONCLUSION
The curriculum must include objectives that introduce clinical guidelines to devise a standardized protocol for safety and quality work concepts in order to reduce the risk of errors in practicing and promote patient safety.
This is an open-access article distributed under the terms of the Creative
Commons Attribution Licence (CC BY) 4.0 https://creativecommons.
KEYWORDS
Patient, Rehab Sciences, Healthcare, Safety, Quality, Education, risk
Iqra Rani
Occupational Therapist
Freelancer
[Rani T. Attitude and Preference of Rehab Sciences Students On Patient Safety And Quality Improvement Education.Pak.j.rehabil.2021;10(1):0–]
10.36283/pjr.zu.10.1/009
Patient safety is defined as the prevention of harm to the patient associated with the healthcare system1. On the other hand, quality improvement education may help improving patient outcomes such as satisfaction, preventing harm, and reducing fiscal costs. Thus, both the terminologies are interconnected. Yet a number of studies have been shown that providing patient safety education may help in improve medical standards 2,3. According to Bari et al4 the concept is crucial to learn by all health care professionals in their certain levels of training. In addition, medical understudies have the potential to prevent medical errors if they have trained in patient safety skills prior to their practice5. However, Health care professionals need to realize the importance to educate undergraduate students about patient safety to handle the situation when dealing with an error6. Therefore, students are required to focus more on patient safety and physical therapy error during clinical practice 7,8. In Pakistan, it has been revealed that a lack of attention to patient safety among health care professionals is evident. This may lead to medical errors as many patients might have been facing other health-related issues which in turn increase their hospital stay9. Even though it was documented that senior medical students tend to have less knowledge regarding patient safety10.
As students are the future professionals, therefore their foundation of knowledge should be built strong during learning years to bring out effective solutions in healthcare delivery. Moreover, the awareness may lead to a greater impact on the patient, subsequently to a better prognosis. Despite the fact, lack of quality improvement education may serve as a barrier to patient safety. However, currently, no specific guidelines are available regarding the patient safety and quality improvement11. A study conducted by Gaw, Alshehab, and Alsheikh12 investigate the level of awareness, knowledge, and perceptions about patient safety of undergraduate students via the Health Professional Education in Patient Safety Survey (H-PEPSS) concluded that students in the 5th year had a high level of confidence in labeling patient safety issues in medical education whereas, students in the 6th year reported to be unhesitating to speak up about patient safety. Moreover, the study also highlights a comparison of the culture of safety and effective communication between males and females that revealed a statistically significant difference between both genders. Thus, there is an identified knowledge gap is existing among the undergraduates about patient safety concepts.
Another study explored that the perceptions regarding patient safety, attitude and knowledge of medical students about patient safety showed that 50% of the students had high knowledge but patient safety education was insufficient which showed a crucial need for formal curriculum and better policies on the concept13. In addition, Lee, Hahm, and Lee14 evaluated undergraduate medical students’ perceptions about safety, teamwork, error disclosure, and behavioral intentions during their clinical clerkship displayed that 78% of students were influenced by teamwork although 41.2% of students reported having the intention to disclose an error if their team member committed it. Furthermore, the majority of students were facing difficulty while discussing medical errors. Therefore, it is inevitable to discuss guidelines in developing to enhance patient safety education.
According to Teigland et al15 more than 80% of participants believed that patient safety education was equal or greater important than basic science or clinical skills, while 70% of students rated quality improvement education to be equal or more important. Thus, it was also showed that teaching of these concepts should be adequately integrated into clinical education. In addition to it, undergraduate medical students have shown a positive attitude towards patient safety despite having little knowledge regarding error disclosure10. Besides, physical therapy students also showed assurance towards patient safety, however, demonstrated high pressure during their work setting which leads to having compromised patient safety that can increase the risk of error or patient injury during physical therapy in a clinical setting16.Thus by teaching the students about patient safety during their study program aids to improve the work quality within the area in which they are functioning and have them to develop the adequate clinical practice that is needed to be executed.
To the best of the author’s knowledge, there is no data available that explore student attitudes and preferences about patient safety and quality improvement education in the profession of physical and occupational therapy. Besides, there are relatively few studies in Pakistan that have been evaluated patient safety awareness in the fields of medicine and nursing. Therefore, this study will serve as a bridge to ascertain the emerging concept of patient safety and quality improvement education in the medical curriculum, in particular for rehab sciences so that they are able to direct their patient well.
Hence, the knowledge of patient’s safety awareness should be given to the students of physical and occupational therapy, as this will aid them to work more efficiently in future. Thus, teaching the proper guideline of patient safety to the students during their learning years, help them to eradicate the medical errors related to patient safety in future. And they will be able to work more professionally in future to avoid any harm and improve patient satisfaction.
Consecutively, this study will devise future research options in this context to facilitate better services.
Study Setting: This study was conducted at the rehabilitation institutes of Karachi including Institute of Physical Medicine and Rehabilitation (IPM&R), Liaquat National School of Physiotherapy (LNSOP), Isra Institute of Rehabilitation and Dr. Ziauddin Hospital, North and Clifton campuses respectively.
Target Population: Undergraduate physical and occupational therapy students.
Study Design: Cross-sectional survey.
Duration of Study: 6-8 months.
Sampling Technique: Non-Probability Convenience Sampling Technique.
Sample size was calculated by using Open EPI software. Therefore, at anticipated frequency of 50%, Confidence Interval of 95% with margin of error at 5%, the sample size of n=134 were calculated.
Sample Selection
Inclusion criteria
- Male and female undergraduate physical and occupational therapy students of 3rd to 5th year and house officers with an experience of > 6 months were included.
Exclusion criteria
- Students who are unwilling to participate or are their initial years of education were excluded from the study.
Data Collection: The self-administered questionnaire has been adapted from the study of Teigland et al15 divided into three sections i.e. section ‘A’ comprised of socio-demographic background of participants, ‘B’ consisted of questions to analyze the impact of knowledge about the patient safety and quality improvement education while C’ constituted of statements to elicit the level of attitude and preferences of rehab students on a 5 point Likert scale listed as strongly disagree, disagree, undecided, agree and strongly agree.
Participants were enrolled in study through convenience sampling technique from primary and tertiary care hospitals. The questionnaire was formulated in Google Docs and sent to participants via email or WhatsApp group. Prior to collection, all participants were given consent form to ensure their voluntary participation. After their consent, understanding about the questionnaire was ensured in order to record the responses on self-administered questionnaire. The data was analyzed upon completion of sample.
Data was analyzed on the Google Docs Editor. The demographic characteristics of the participants were represented through frequency, mean and standard deviations whereas the participant responses were evaluated through frequency and percentage.
According to the participants the ethical consideration criteria includes:
Ethical consideration was taken via verbal and written consent by the participant before starting the data collection. All information of the participants will be kept anonymous under investigator’s supervision. However, there will be fair selecting criteria without being unjust to the participants.
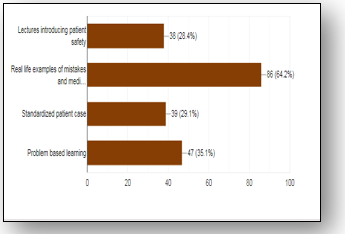
A total number of 134 responses received from the participants included (56.7%) occupational while (43.3%) physical therapy students of 3rd year (36.6%), 4th year (31.3%) and 5th year (32.1%) respectively with the highest number of responses reported from the age group of 21 to 23 years (31.3%). In Section-B, it was reported that majority of students (67.9%) have rated their current knowledge of patient safety as an average, (26.1%) excellent while only (6%) rated as poor, in comparison to the importance of basis science knowledge, students reported the patient safety information (64.9%) and clinical knowledge (56%) as more important. It was revealed that (50.7%) have attended formal education regarding patient safety from lecture, workshops or seminars while (48.5%) have received from informal education. Besides, students have preferred real life examples (64.2%), problem based learning (35.1%), lectures (28.4%) and cases (29.1%) that will be helpful in teaching about the patient safety as shown in Figure-1.
Figure-1 Represents the perception of students regarding teaching aids in patient safety education
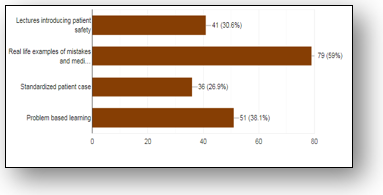
In Section-C, (79.9%) students reported to have an average knowledge of quality improvement while on (6%) have rated having poor knowledge. In comparison to basic science knowledge, (50.7%) marked the quality improvement knowledge as of same important, (48.5%) more important while (56.7%) and (41%) rated clinical knowledge of same and more importance. Moreover, (46.3%) have attended quality improvement education from formal (41.8%) and (34.3%) informal education respectively. Furthermore, students have preferred real life mistakes (59%), problem based learning (38.1%), lectures (30.6%) and cases (26.9%) that will be helpful in teaching about quality improvement education as shown in Figure-2.
Figure-2 represents the perception of students regarding teaching aids in quality improvement education
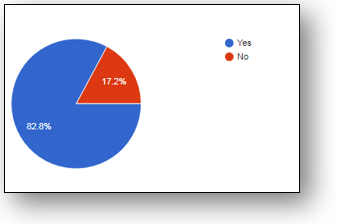
In section D, (51.5%) students believed that most of the medical errors are impossible to avoid while (48.5%) disagreed, however majority (63.4%) thought that if there is no harm to client than there is no need to report the error while in the presence of error that may lead to patient harm should be disclosed by the therapists (82.8%) as shown in Figure-3, although it was strongly believed that (97.8%) good communication, (98.5%) patient participation and motivation as well as (96.3%) multidisciplinary teamwork plays a vital role in reducing risk of error.
Figure-3 represents the perception of students regarding error disclosure
It was showed that (89.6%) believed that clinical errors made it easy to learn from errors of others however (94%) agreed to have detailed knowledge about medical errors, although (97%) prefer that therapist should insist on the importance of proper therapeutic resources for patient safety and should admit the errors and must devise effective strategy. In addition, (58.2%) believed that patient safety is learned through clinical experience only and (95.5%) preferred that the topic should be included as a separate curriculum in undergraduate program.
Despite of the fact, number of participants was willing to spread awareness regarding CPR training (61.9%) about currently available courses/training seminars (13.6%) while (23.7%) thought free training as the best method to increase the awareness of CPR (Figure-5).
The findings of this study showed that that majority of students (67.9%) and (79.9%) have rated their current knowledge of patient safety and quality improvement as an average. Besides, majority of students have preferred real life examples and problem based as helpful in teaching these aspects Moreover, it was strongly believed that (97.8%) good communication, (98.5%) patient participation and motivation as well as (96.3%) multidisciplinary teamwork plays a vital role in reducing risk of error while (89.6%) believed that clinical errors made it easy to learn from errors of others. Consecutively, (95.5%) preferred that the topic should be included as a separate curriculum in undergraduate program.
The last decades have shown significant progress in teaching about patient safety and quality improvement among medical professionals17. The students of our study reported having recognition of these concepts despite having varied exposure. Besides, in general, the majority of students preferred these topics in their curriculum comprising of hands-on approaches, lectures and independent study methods, and real life mistakes or participation in as most helpful. The findings of our study were consistent with the study of Teighland et al15 who demonstrated that teaching of patient safety and quality improvement to medical understudies shall be integrated into clinical education rather than taught alone.
Despite this, the attitudes and learning preferences of students are important to consider when implementing a curriculum change that may assist in prioritizing the effective pedagogical methods also leads to the understanding liable curriculum18. On the contrary, Thain and colleagues19 concluded that 70% of students preferred internet-based learning for patient safety although our study didn’t explore the participant’s perception in this regard. However, similar results demonstrated in our and Thain’s study declared that the majority of students thought real-life mistakes as most valuable to learn and reduces the risk of error.
It was further revealed that students of the modern era preferred quality improvement education in simulated environments like virtual reality that perhaps due to the divergence in students’ attitudes towards internet-based learning. However, as per our study results, it seemed that students preferred to have real-life situations to be engaged in proper learning therefore, education should be delivered in as real an environment as possible.
A number of authors have also suggested that lacking fully trained educators in medical curricula may lead to slow integration of these topics20,21. Therefore, the curriculum should be devised as a promising paradigm in medical education. Furthermore, students’ participation in the integration of the knowledge may serve as an effective support to improve quality care22,23. Likewise in our study, the majority of students have taken a number of lectures, seminars, workshops, etc. that highlight their interest in learning these concepts with appropriate knowledge and skills in the topic. Therefore, integration of knowledge and student’s recognition in these topics may leads to enhancement in medical curriculum and shall endorsed high quality teaching24,25.
Thus in present days, it is hard to get enough guideline on patient safety. And due to lack of awareness, the amount of knowledge that should be given were taking for granted by the students which leads to have compromised patient safety and causing the increase of medical errors in the work setting by them.
However, this study will help rising new thoughts about improving quality and will work towards effective educational programs of patient safety, that to be implemented in their clinical practice in order to provide the finest possible service to the patient. Beside this will benefit students to reduce medical errors in future clinical practice by discussing and learning the guideline about patient safety.
To the best of author’s knowledge, this study is the first to be conducted in Pakistan considering about patient safety and quality improvement education. The study has highlighted the importance aspects in medical curricula that is crucial for healthcare professionals to understand, in particular rehabilitation specialist to provide better and safer patient care in their clinical practice.
Several limitations have been encountered in our study included that participants may have been more likely to be interested in patient safety and quality improvement. Furthermore, the survey represents the opinions from a single rehab facility therefore the preferences may not be generalizable to other schools.
It was concluded that majority of the participants has an average knowledge regarding patient safety and quality improvement education thereby shown a positive attitude and the proactive preferences regarding it. However, future studies shall be directed on the clinical guidelines to devise a standardized protocol for these concepts in order to reduce the risk of errors in practicing and promote patient safety. Consequently, it is recommended that the medical curricula should be upgraded taking into account the patient safety and quality improvement education as a sole course with real-life exemplariness and problem based learning.
- Asem N, Sabry HA, Elfar E. Patient safety: knowledge, influence and attitude among physicians: an exploratory study. Journal of the Egyptian Public Health Association. 2019 Dec 1;94(1):22.
- Halbach JL, Sullivan LL. Teaching medical students about medical errors and patient safety: evaluation of a required curriculum. Academic medicine. 2005 Jun 1;80(6):600-6.
- Myung SJ, Shin JS, Kim JH, Roh H, Kim Y, Kim J, Lee SI, Lee JH, Kim SW. The patient safety curriculum for undergraduate medical students as a first step toward improving patient safety. Journal of surgical education. 2012 Sep 1;69(5):659-64.
- Bari A, Jabeen U, Bano I, Rathore AW. Patient safety awareness among postgraduate students and nurses in a tertiary health care facility. Pakistan journal of medical sciences. 2017 Sep;33(5):1059.
- Henderson D, Carson-Stevens A, Bohnen J, Gutnik L, Hafiz S, Mills S. Check a box. Save a life: how student leadership is shaking up health care and driving a revolution in patient safety. Journal of patient safety. 2010 Mar 1;6(1):43-7.
- Kiesewetter I, Könings KD, Kager M, Kiesewetter J. Undergraduate medical students’ behavioural intentions towards medical errors and how to handle them: a qualitative vignette study. BMJ open. 2018 Mar 1;8(3).
- King J, Anderson CM. Patient safety and physiotherapy: what does it mean for your clinical practice?.
- Anderson JC, Towell ER. Perspectives on assessment of physical therapy error in the new millennium. Journal of Physical Therapy Education. 2002 Dec 1;16(3):54.
- Shiwani MH. Reforms for safe medical practice. JPMA. The Journal of the Pakistan Medical Association. 2007 Apr;57(4):166.
- Kamran R, Bari A, Khan RA, Al-Eraky M. Patient safety awareness among undergraduate medical students in Pakistani medical school. Pakistan journal of medical sciences. 2018 Mar;34(2):305.
- Slusser LR, Rice MS, Miller BK. Safe patient handling curriculum in Occupational Therapy and Occupational Therapy Assistant Programs: a descriptive study of school curriculum within the United States of America. Work. 2012 Jan 1;42(3):385-92.
- Gaw ZR, Alshehab AM, Alsheikh RH. Medical Student Awareness And Knowledge Of Patient Safety At Imam Abdulrahman Bin Faisal University. International Journal of Scientific Research. 2019 Nov 28;8(11).
- Nabilou B, Feizi A, Seyedin H. Patient safety in medical education: students’ perceptions, knowledge and attitudes. PloS one. 2015 Aug 31;10(8):e0135610.
- Lee HY, Hahm MI, Lee SG. Undergraduate medical students’ perceptions and intentions regarding patient safety during clinical clerkship. BMC medical education. 2018 Dec 1;18(1):66.
- Teigland CL, Blasiak RC, Wilson LA, Hines RE, Meyerhoff KL, Viera AJ. Patient safety and quality improvement education: a cross-sectional study of medical students’ preferences and attitudes. BMC medical education. 2013 Dec 1;13(1):16.
- Struessel T, Forster JE, Van Zytveld C. Doctor of Physical Therapy Student Experiences During Clinical Education: Patient Safety, Error, and the System. Journal of Physical Therapy Education. 2019 Mar 1;33(1):3-15.
- Donaldson MS, Corrigan JM, Kohn LT, editors. To err is human: building a safer health system. National Academies Press; 2000 Apr 1.
- McNulty JA, Sonntag B, Sinacore JM. Evaluation of computer‐aided instruction in a gross anatomy course: A six‐year study. Anatomical sciences education. 2009 Jan;2(1):2-8.
- Thain S, Ang SB, Ti LK. Medical students’ preferred style of learning patient safety. BMJ quality & safety. 2011 Feb 1;20(2):201-.
- DesHarnais SI, Nash DB. Reforming way medical students and physicians are taught about quality and safety. Mount Sinai Journal of Medicine: A Journal of Translational and Personalized Medicine. 2011 Nov;78(6):834-41.
- Ogrinc G, Nierenberg DW, Batalden PB. Building experiential learning about quality improvement into a medical school curriculum: the Dartmouth experience. Health affairs. 2011 Apr 1;30(4):716-22.
- Bohomol E, Freitas MA, Cunha IC. Patient safety teaching in undergraduate health programs: reflections on knowledge and practice. Interface-Comunicação, Saúde, Educação. 2016 Mar 1;20:727-41.
- Boonyoung N. Head Nurses’ management regarding patient patient safety and its related factors in public hospitals aceh Province, Indonesia (Doctoral dissertation, Prince of Songkla University).
- Mahmud MD. Effeectiveness of Group therapy with Conventional Therapy Among Cerebral Palsy (CP) Children (Doctoral dissertation, Department of Physiotherapy, Bangladesh Health Professions Institute, CRP).
- Nair P, Barai I, Prasad S, Gadhvi K. Quality improvement teaching at medical school: a student perspective. Advances in Medical Education and Practice. 2016;7:171.
