ABSTRACT
AIMS AND OBJECTIVES
Sleep deprivation is a major contributor of health and mental problems that may cause serious difficulties in accomplishing ADL’s among students although severe health and mental conditions have direct impact on the quality and quantity of sleep too. Thus, this study aims to determine the quality of sleep and its association between anxiety, depression, and stress to improve health related quality of life (HRQOL) among undergraduate DPT students of ZCRS.
STUDY DESIGN
A cross-sectional survey
SAMPLE SELECTION
325 students were selected through convenience sampling technique from pre-clinical (1st, 2nd) and clinical (3rd, 4th, 5th) years of DPT program.
PROCEDURE
Data was collected on by providing Pittsburgh Sleep Quality Index and Depression, Anxiety and Stress Scale-21 to both students of pre-clinical and clinical years at beginning, middle and end of semester to determine the association of related outcome measures.
RESULTS
Strong association was found between sleep deprived students with depression, anxiety, and stress on chi-square test of association (p<0.05).
CONCLUSION
It was concluded that high prevalence of anxiety followed by depression and stress with the quality of sleep along with the amount of sleep in university students during all three phases of their academic semester. Although studies proposed genetic co-relation with anxiety, depression and stress as well as with the quality of sleep.
KEYWORDS
Depression, Anxiety, Sleep, sleep deprivation,Health-related quality of life, activities of daily living.
Beenish Zafar
Assistant Professor
Ziauddin College Rehabilitation
Sciences
Ziauddin University
[email protected]
Farzana Amir
Head of Department
Preventive Cardiology & Cardiac Rehabilitation
Chair Institutional Review Committee TABBA Heart Institute
[email protected]
Syed Wasif Ali
Associate Professor
Jinnah College of Rehabilitation
Sciences
[email protected]
[Zafar B,Amir F,Ali SW. Association of Depression, Anxiety and Stress with Quality of Sleep among DPT students of ZCRS Pak. j. rehabil. 2019;8(1):37-42]
This is an open-access article distributed under the terms of the Creative
Commons Attribution Licence (CC BY) 4.0 https://creativecommons.org/
Sleep deprivation can cause serious health and mental problems and can cause issues in performing activities of daily living1. Sleep, a compute of quanti-tative and qualitative components1. The duration of sleep comes under quantitative component while the depth and feeling of relaxation upon arousing is the domain of, the qualitative component1. Sleep quality and duration generally varies among genders and ages, though findings are inconsistent across studies. As according to one study, female students or individuals with increased age has been identified as having a higher risk of poor sleep quali-ty1 while one another study suggested one-third adult population is affected by sleep disorders2.
Sleep disturbances are so frequently perceived as a symptom that is indicative of certain psychiatric disorders as well as they are listed as diagnostic criterion under Diagnostic and Statistical Manual of Mental Disorders (DSM-IV)3.
A cross-sectional research performed at Auckland gave an idea about the correlation of sleep with anxiety and depression that was found to be total of 39.4% of the students had considerable sleep symp-toms lasted longer than 1 month. The most prevailed reason for sleep symptoms were depression and anxiety, found to be 17.3% and 19.7% respectively4.
Whereas stress is mind’s and body’s way of dealing with new complexity or complication in life, it’s good for making competitive and motivated individuals or sometimes this stress produces negative impact that leads to anxiety and depression5. People with family history of depression and anxiety are at higher risk of sleep disorders6.
Lack of involvement, loss of interest, persistent feeling of sadness, aversion to activity and low mood all leads to depression7; Depression is not just low spirits or bad mood that can influence a person’s opinion, belief and behavior, judgment, tendencies, feelings, and sense of frame of comfort and well-being. It’s a grave intellectual health state (mental illness) influencing both psychological and physical health6-7.
However, Anxiety is communal term for quite a few disorders such as fear, panic, alarm, dread, terror, apprehension, nervousness, and worrying etc. Hence affects our behavior7. Occasional anxiety is a normal part of life7. One may feel anxious when faced with a difficulty at work, prior taking a test, or making an important decision. Anxiety is simply considered as state of uneasiness in usual day to day life6-7.
One study revealed the prevalence of anxiety among medical students attending universities as 43.7%in Pakistan, 54.5% in Malaysia, 65.5% in Greece, and 69% in Beirut, while the prevalence of anxiety among students attending private medical colleges has been estimated to be 29.4% in Israel, 56% in India, and 60% in Pakistan8. However students with poor mental health suffering from depression, anxiety and stress are subjected to various problems including, bad academic, abandoning studies (drop out), and difficulty in managing relation with friends and family, and incompetent to survive a stressful situation. It results in reduced self-trust that had a direct impact on students’ academic perfor-mance6-8.
The Pittsburgh Sleep Quality Index (PSQI), used to assess the sleep quality during the past month. It has been designed in such a way that it can be used in multiple settings, including research and clinical activities, for the identification of sleep disorders. It has 9 questions and 7 components that evaluated participant’s sleep quality, sleep latency, sleep dura-tion, habitual sleep efficiency, sleep disturbances, uses of sleep medication and daytime dysfunction over the past month. This tool covered 19 individual items. Each item was scored on 0-3 interval scale, yielding one global score on the whole ranging from 0 to 21. Individuals that attained higher than 5 are considered sleep deprived9-10.
The Depression, Anxiety and Stress Scale (DASS-21) assessed participants’ mental health during the past week. It is a dimensional rather than a categorical conception of psychological order. This self-adminis-trated questionnaire has 21 items related to three components indicating mental health that are stress, anxiety and depression; each module consisted of 7 questions. Participants ranked each question from 0 to 3, 0 indicating the item “don’t apply to them at all”, to 3 indicating that the item “apply to them very much”. Subjects were given 4-point severity scales to rate the degree, they had been through each condition on the period of last week10.
Study Design
Longitudinal Study
Sample Size
A sample of 325 students was recruited in the study.
Study Setting and Participants
This longitudinal study was conducted among the DPT students from1st, 2nd, 3rd, 4th and 5th year at Ziauddin College of Rehabilitation Sciences.
Study Duration
This survey was conducted over the six months period.
Sampling Technique
Students were recruited for this survey through convenience sampling technique.
Inclusion and Exclusion Criteria
- DPT students from 1st, 2nd, 3rd, 4th and 5th year aged 18-25 years with written consent to participate in this survey were included.
- Any other medical and paramedical students or participants who have submitted incomplete ques-tionnaires were also excluded3, 11, 12.
Data Collection Tools
The participants were given a set of questionnaires consisted a consent form, a sociodemographic questionnaire that required each student to provide their age, gender and year of study and a DASS scoring system (the Depression, Anxiety and Stress Scale)10 along with the Pittsburgh Quality of Sleep Index (PSQI)9-10. Both the tools had open access to be used as per required. The questionnaire was culture free and that made the test feasible to adapt to any culture11.
Data Collection Procedure
Data was obtained through questionnaires among participants. Prior to the study signed consent was obtained from all the participants and were informed about the objectives and goals of this survey and assured anonymity. The recruitment was done at the start of the research that is students of all DPT years at the beginning of semester and collec-tion of data was performed in three phases:
- Start of the semester: the data was collected from all years students enrolled in undergraduate DPT program.
- Middle of the semester: then again students were given the same questionnaires to be evaluated during mid-semester.
- At the end of the semester: students yet again were assessed by the same questionnaires at the closing stages of the semester a week before the finals.
Data Analysis Strategies
SPSS version-20 was used for data analysis. Partici-pants demographic details were represented through mean age and percentage whereas scoring on PSQI and DASS-I were shown in terms of frequency and percentages.
Ethical Considerations
Both the tools had open access therefore no permis-sion was required to utilize these questionnaires as they had open right to use. Prior to consent, detailed understanding of questionnaires was provided to the participants.
308 out of 325 questionnaires received were correct-ly filled by the enrolled participants with mean age of 20 ±1.5 where 20.1% were male and 79.9% were female students.
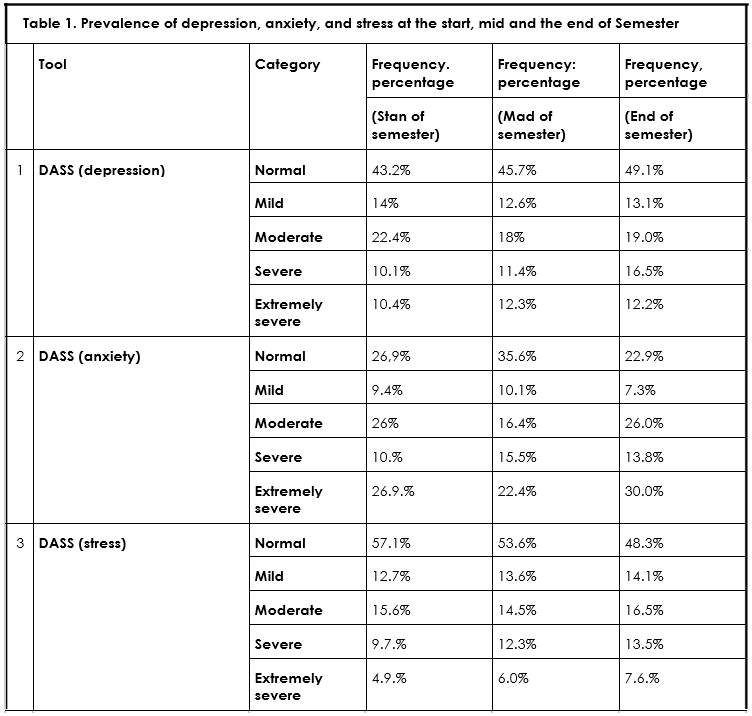
Results obtained at the start of semester from PSQI concluded that 76.0% students were deprived of sleep. Whereas depression, anxiety and stress calcu-lated on DASS-21 scale showed that 14% students were mild depressive, 22.4% were moderately depressed, 10.1% were severe while only 10.4% showed extremely severe depression. Similarly anxiety was found to be normal in 26.9%, 9.4% were mild anxious while 10.7% were in severe anxiety. Moreover, stress was reported normal in 57.1% of students, moderate in 15.6% of students, severe in 9.7% students and extremely severe in 12.7% of students.
Another set of data was collected at the mid of the semester that showed 73.2% students had reduced sleep quality calculated in PSQI. Furthermore, on DASS-21, 12.6% exhibited mild symptoms of depres-sion, 18% had moderate depression, while 11.4% were with severe depression. Anxiety was found to be normal in 35.6%, mild in 10.1%, moderate in 16.4%, severe in 15.5% students. On the contrary stress was reported normal in 53.6%, mild in 13.6%, moderate in 14.5%, severe in 12.3%, and extremely severe in 6.0% students.
The last data was gathered at the end of the semes-ter. Sleep quality measured on PSQI revealed that, 72.2% students had poor sleep characteristics. Estimation on DASS-21for depression was ranked normal in39.1%, mild in 13.1%, moderate in 19.0%, severe in 16.5% students. While anxiety appeared tobe normal in 22.9%, mild in 7.3%, moderate in 26.0%, severe in 13.8% students. Although stress was found to be normal in 48.3%, mild in 14.1%, moderate in 16.5%,severe in 13.5% students. The prevalence of Depression, Anxiety and Stress scores of all phases of semester are depicted in Table-1.
A chi-square test of association showed significant association (p<0.05) of sleep with depression, anxiety and stress in all phases of semester as shown in Figure1, 2 and 3.
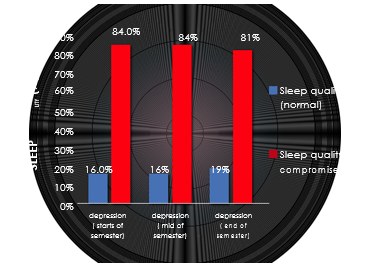
Figure 1. Association of depression with sleep
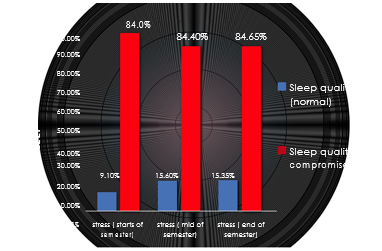
Figure 2. Association of stress with sleep
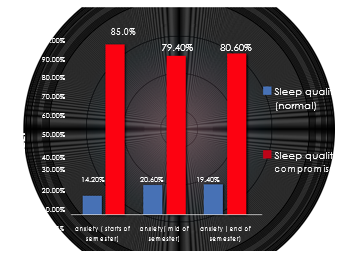
Figure 3. Association of anxiety with sleep
The prevalence of poor sleep quality in the present longitudinal study was 73.66%. Whereas different studies stated different prevalence for sleep disorders, in Wuhan University, had 17.7% of students had poor sleep13 while 55.8% had been reported sleep deprived in Ethiopia10. Moreover, 72% of students suffer from poor sleep in north border univer-sity Saudi Arabia14. However, another study conducted on university students in Lebanon report-ed 50.8% of students had poor sleep quality6 while students of Klaipeda reported 69.9%15, in Lahore 77.2% were suffered from sleeplessness16. Hence, a study stated that poor-quality sleep leads to depres-sion, and anxiety14 and bad behaviors3 that are due to academic pressure. Also, private university students are more under pressure than the others it could be due to high fees8.
As depression is common among students reported in the existing study 57.3%, other studies conducted in several universities report depression among their students as 10.6% had been reported in Wuhan University13 and 50.8% in Ethiopian students10. Where-as the study conducted on high school students, Chinese adolescent in Guandong stated 6.4% of students who showed depressive symptoms17. The undergraduate students of Sindh, Pakistan reported 48% students with depression11 while study occurred in Islamabad reported 40.9%18. A survey conducted in several universities in Auckland reported 17.3%4. Anxiety reported in the current study was72%. Whereas, Anxiety observed in students of Ethiopia is 58%10 also at north border of Saudi Arabia it was observed in 92% of medical students14 and among undergraduate students of Sindh reported was 68.4%11 on other hand in Islamabad 74.2% students were observed to be anxious18 The Universi-ty of Auckland stated anxiety in 19.7% of its students4. Anxiety has been reported most in transfer students, upperclassmen and those living off-campus7.
Findings from the present study indicate that there was a strong association between poor sleep quality and mental health problems i.e. depression, anxiety and stress throughout the semester. The findings obtained from one cross-sectional study conducted on female medical students stated that there was a strong association between undesirable sleep quali-ty and depression, anxiety, and stress that can be attributed to the P-value that was equal to 0.000. Specifically, 93.4% of students were found with com-promised sleep along with depressive symptoms, while 84.1% students showed poor sleep quality with anxiety and 90.1% of students experienced undesir-able sleep with stressful symptoms19. This strong association supports the findings of the present study with a P-value of 0.000 for all the variables. But the difference in percentages was found in the present study that was 83% of students with compromised sleep had depression, 86.35% of students with poor sleep quality had anxiety and 81.93% of students with low quality of sleep had stressful symptoms. Despite the fact, this difference can be attributed to gender difference as females were found with more com-promised sleep along with depression, anxiety, and stress20. Another study conducted on medical students of Tehran University, Iran also showed a strong association21. However, many factors influence these variables like academic stress of mainly getting poor grades, large content of study material, exam and time constraints, insufficient family time, emotional distress, financial issues. More-over, mental health can badly influence academic performance and may have played a role in substance abuse like smoking, caffeine consump-tion, etc22.The results obtained from the present study demonstrated that the mean sleep quality of male and female students had no significant difference that was consistent with the finding of multiple studies 21-25. Whereas, the study done in Iran exhibited that the mean sleep quality of males were less com-promised then females20.
The current study demonstrated that the mean depression, anxiety, and stress were more in females than males that were consistent with the finding of another study held at Fasa medical University20 and also in another study carried out in Islamabad showed the same results18. However, women are more often affected by depression4 whereas men are more anxious3-8. Although, the outcome of the studies varied with the results of this current study that showed stress, depression and anxiety and sleep disturbances were equal in both the genders13-16. It could be due to cultural differences. However, research stated that students who are sleep deprived had a higher incidence of depression and anxiety15. Another study reported that sleep disorder is increasing globally in adolescents aged between 13 to 16 years6. While in another research 20-year-old students had compromised sleep6-15.
It was concluded that high prevalence of anxiety was observed among DPT students followed by depression and stress in all three different phases. Whereas, the vast majority of students appeared to be sleep deprived. Moreover, strong associations were found between the poor quality of sleep in students who are exposed to depressive, anxiety and stress symptoms.
- Lemma S, Gelaye B, Berhane Y, Worku A, Williams MA. Sleep quality and its psychological correlates among university students in Ethiopia: a cross-sec-tional study. BMC psychiatry. 2012 ;12(1):237.
- Dikmen PY, Yavuz BG, Aydinlar EI. The relationships between migraine, depression, anxiety, stress, and sleep disturbances. Acta Neurologica Belgica. 2015;115(2):117-22.
- Pensuksan WC, Lertmaharit S, Lohsoonthorn V, Rattananupong T, Sonkprasert T, Gelaye B, Williams MA. Relationship between poor sleep quality and psychological problems among undergraduate students in the Southern Thailand. Walailak journal of science and technology. 2016;13(4):235.
- Samaranayake CB, Arroll B, Fernando AT. Sleep disorders, depression, anxiety and satisfaction with life among young adults: a survey of university students in Auckland, New Zealand. NZ Med J. 2014;127(1399):13-22.
- Jahan F, Siddiqui MA, Mitwally M, Zubidi A, Jasim NS, Zubidi A, Jasim HS. Perception of stress, anxiety, depression and coping strategies among medical students at Oman medical college. World Family Medicine Journal: Incorporating the Middle East Journal of Family Medicine. 2016;99(3719):1-8.
- Choueiry N, Salamoun T, Jabbour H, El Osta N, Hajj A, Khabbaz LR. Insomnia and relationship with anxiety in university students: a cross-sectional designed study. PloS one. 2016;11(2):e0149643.
- Beiter R, Nash R, McCrady M, Rhoades D, Linscomb M, Clarahan M, Sammut S. The prevalence and correlates of depression, anxiety, and stress in a sample of college students. Journal of affective disorders. 2015;173:90-6.
- Saravanan C, Wilks R. Medical students’ experi-ence of and reaction to stress: the role of depression and anxiety. The Scientific World Journal. 2014;2014.
- Hershner SD, Chervin RD. Causes and conse-quences of sleepiness among college students. Nature and science of sleep. 2014;6:73.
- Lemma S, Gelaye B, Berhane Y, Worku A, Williams MA. Sleep quality and its psychological correlates among university students in Ethiopia: across-sectional study. BMC psychiatry. 2012;12(1):237.
- Syed A, Ali SS, Khan M. Frequency of depression, anxiety and stress among the undergraduate physiotherapy students. Pakistan journal of medical sciences. 2018;34(2):468.
- Al-Maddah EM, Al-Dabal BK, Khalil MS. Preva-lence of sleep deprivation and relation with depres-sive symptoms among medical residents in King Fahd University Hospital, Saudi Arabia. Sultan Qaboos University Medical Journal. 2015;15(1):e78.
- Feng Q, Du Y, Ye YL, He QQ. Associations of physical activity, screen time with depression, anxiety and sleep quality among Chinese college freshmen. PloS one. 2014 ;9(6):e100914.
- Shathele SM, Oommen A. Factors influencing the academic performance of the female medical students in preclinical and clinical years. Journal of Medicine and Medical Sciences. 2015;6(6):109-14.
- Jurgita A, Šarūnė B, Asta M, Akvilė V. Relations among poor sleep, anxiety and depression among the students of health sciences. Applied research in health and social sciences: interface and interac-tion. 2017;14(1):26-38.
- Waqas A, Khan S, Sharif W, Khalid U, Ali A. Associ-ation of academic stress with sleeping difficulties in medical students of a Pakistani medical school: a cross sectional survey. PeerJ. 2015;3:e840.
- Guo L, Deng J, He Y, Deng X, Huang J, Huang G, Gao X, Lu C. Prevalence and correlates of sleep disturbance and depressive symptoms among Chinese adolescents: a cross-sectional survey study. BMJ open. 2014;4(7):e005517.
- Rizvi F, Qureshi A, Rajput AM, Afzal M. Preva-lence of depression, anxiety and stress (by DASS scoring system) among medical students in Islam-abad, Pakistan. Br J Med Med Res. 2015;8(1):69-75.
- Farzaneh F, Momayyezi M, Lotfi MH. Relationship between quality of sleep and mental health in female students of Shahid Sadoughi University of Medical Sciences (2015). Journal of Fundamentals of Mental Health. 2018;20(2):167-71.
- Najafi Kalyani M, Jamshidi N, Salami J, Pourjam E. Investigation of the relationship between psychologi-cal variables and sleep quality in students of medical sciences. Depression research and treatment. 2017;2017.
- Rezaei M, Khormali M, Akbarpour S, Sadeghnii-at-Hagighi K, Shamsipour M. Sleep quality and its association with psychological distress and sleep hygiene: a cross-sectional study among pre-clinical medical students. Sleep Science. 2018;11(4):274.
- Iqbal S, Gupta S, Venkatarao E. Stress, anxiety & depression among medical undergraduate students & their socio-demographic correlates. The Indian journal of medical research. 2015;141(3):354.
- João KA, de Jesus SN, Carmo C, Pinto P. The impact of sleep quality on the mental health of a non-clinical population. Sleep medicine. 2018;46:69-73.
- Isaac F, Greenwood KM. The relationship between insomnia and depressive symptoms: genu-ine or artifact?. Neuropsychiatric disease and treat-ment. 2011;7:57.
- McGillivray CJ, Pidgeon AM. Resilience attributes among university students: a comparative study of psychological distress, sleep disturbances and mindfulness. European Scientific Journal. 2015;11(5):33-48.
