ABSTRACT
OBJECTIVES
A Quasi experimental study was performed to evaluate the impact of aquatic therapy on sensory modulation in order to improve the ADL’s in children with autistic spectrum disorder.
STUDY DESIGN
A Quasi Experimental study.
SAMPLING TECHNIQUE
Convenience sampling technique was used.
STUDY SETTINGS & PARTICIPANTS
This study was conducted in Liaquat National Hospital-Occupation-al Therapy Peads Unit. The participants were the children with autis-tic spectrum disorder having sensory modulation disorder.
INTERVENTIONS
56 autistic children were enrolled in this study. Each autistic child was first assessed on the basis of sensory profile for sensory deprivation and on WeeFIM pediatric functional independence measure for activities of daily living. The entire protocol was divided into six months of aquatic therapy with a frequency of 3 days a week.
RESULTS
A significant difference was observed in pre and post measurement of sensory profile and WeeFIM score measured by paired t-test. The p-value is found to be 0.03 on sensory profile and a p-value of 0.02 on FIM.
CONCLUSION
The findings indicated that the aquatic therapy has good impact on sensory modulation for activities of daily living.
KEYWORDS
Hydrotherapy, Sensation Disorder, Functional Independence Mea-sure, Short Sensory Profile, Autistic Disorder.
Samreen Quraishi
Occupational Therapist
Liaquat National Hospital
Tooba Jarrar
Occupational Therapist
Liaquat National Hospital
[Qureshi.S, Jarrar.T Impact of Aquat-ic Therapy on Sensory Modulation of Autistic children to improve Activities of daily living. Pak. j. rehabil. 2018;7(2):13-18]
According to the National Health Statistics Reports, Autism spectrum disorder ASD affects 2.24% of children1. ASD is a developmental disorder that is characterized by difficulties in communication and social interaction, along with behavioral rigidity and repetitiveness2. Autism child requires a considerable number of services to improve behavior and devel-opmental challenges3. ASD child often observed sensory processing difficulties in terms of discrimina-tion, interpretation, and organization of sensory modulation.
Sensory modulation is the capability to maintain and grade responses to the environment so that sensory input will respond appropriately to the demands of daily life4. Children with Autistic spec-trum disorder has altered sensory modulation. A study reported increased sensory responsiveness and low sensory integration behavior in autism as comparison with other developmental disorder5. Sensory modulation dysfunction has a significant influence on participation of daily living6.
A study shows that motor development is basic need of an autistic children, in this regard the reha-bilitation centers should focus on children‘s physical movements games and sports to achieve better proficiency in motor development7. Autistic children with different sensory profile usually enjoy calming activities, deep pressures, tactile and vestibular activities to reduce their sensory problems, stereo-type behavior and difficulties in daily living task8. Water and swimming activities are becoming progressively usual activities for children with Autism9. Families find swimming most common phys-ical activity and overall favorite activity in children with disabilities10. Water activities help in energizing, relaxing and providing postural support to muscles thus allows variety of necessary motor skills to be performed that are dependent on an individual’s skills level11,12.
According to the study aquatic based exercises were found to be time effective approach in com-parison to land based in improving balance and functional outcome13. Further, the concept Halliwick exercises of utilizing the body mechanics and hydrodynamics that comprises of 4 phases: adjust into the water, rotations, control of move-ment in water, and movement in water were too found to be effective in improving the motor and functional skills of Cerebral palsy children14. Frenzen and Tryniszewiskil in their 14-week of interventional strategy concluded that gait velocity, stride length and motor function were significantly improved among children given intervention on aquatic exercises program15. Similarly 12 weeks of hydrother-apy program was also found to be effective in improving motor activity among children with ASD16. A survey performed by occupational therapists regarding the efficacy of hydrotherapy strategy revealed their perception that the strategy was not only effective in improving balance but indeed found to be effective in improving muscle strength, touch toleration, eyecoordination and social participation17.
Although the effectiveness of aquatic based exercises interventions are found to be proven in improving the balance and functional outcome among cerebral palsy children but the gaps in literature still exist regarding the effectiveness of strategy among autistic children. Hence our study is aimed to determine the impact of structural six weeks of aquatic based exercises program in improving the sensory modulation of autistic children.
Study Design
It was quasi-experimental study
Study Settings
This study was conducted in Liaquat National Hospi-tal
Study Duration
8 months
Sampling Method
Non probability convenient based sampling was used
Sample Size:
The Sample size of 56
Inclusion Criteria
- 5 to 8 years of diagnosed Autistic Children
- Able to follow simple commands19.
Exclusion Criteria
Children who has physical disability or decreased fitness or unable to walk independently and other medical symptoms which can be hinder in their performance15.
Data Collection Tool
- The data tool was sensory profile and Functional independence measure WeeFIM for pediatric clients.
- Short Sensory profile used for sensory modulation disorder and WeeFIM for activities of daily living.
Short Sensory Profile
A sensory profile is an assessment tool that helps to measure the children’s sensory processing on regu-lar performance. It is a standardized questionnaire comprise on 38 statements, all arise from the longer sensory profile. It is consist on >125 statements. A short sensory profile have 7 categories i.e. movement sensitivity, tactile sensitivity, taste sensitivity, visual auditory sensitivity, auditory filtering, under responsive seeking, low energy20. The occupational therapist rate the child response according to each statement on out of 5 points, i.e. (1=always, 2=fre-quently, 3=occasionally, 4=seldom, 5=never). The highest score suggest maximum number of behav-iors that are in normal limits. This tool is used in research to measure the sensory modulation21. The reliability of short sensory profile is 0.70-0.90 whereas the construct validity of the SSP total and section scores ranges from (0.25-0.76)20, 21.
Functional Independence Measure (WeeFIM)
The Functional Independence Measure for pediat-ric (WeeFIM) evaluates the functional class of a child on the basis of assistance level ,he or she requires. The scale consists of 18 items, with two parts in it–A motor and B cognition. Each statement is scored on out of 7 point ordinal scale. The highest the patient gain the score, the more patient is independence in daily activities of life. I t measures several metrics of functional ability including selfcare(feed, groom, bath, dress, and complete toileting tasks including the management of bowel and bladder), mobility(transfer in/out of a chair or wheelchair, on/off a toilet, or in/out of a tub or shower, walk, crawl, or use wheelchair; and go up and down stairs), and cognition(understands, expresses themselves, interacts with peers, solves daily problems, and recalls information). WeeFIM measures the improvement — or gain — in the areas from time to time during therapy.
Data Collection Procedure
The study was conducted on 56 autistic children both male and female (17 female, 39 male) aged between 5 to 8 years old, were selected among the children’s currently receiving therapy sessions at an outpatient occupational therapy department. The participants were known case of autistic spectrum.
Disorder and having definite difference in sensory modulation. The consent was taken from the parents/guardians prior to the study. The partici-pants of study were assessed on Sensory profile to assess their sensory modulation, deficits in the integration of sensations and WeeFIM to assess their Functional independence before and after the study. The autistic children were given 45 minutes of aquatic therapy thrice a week for six months.
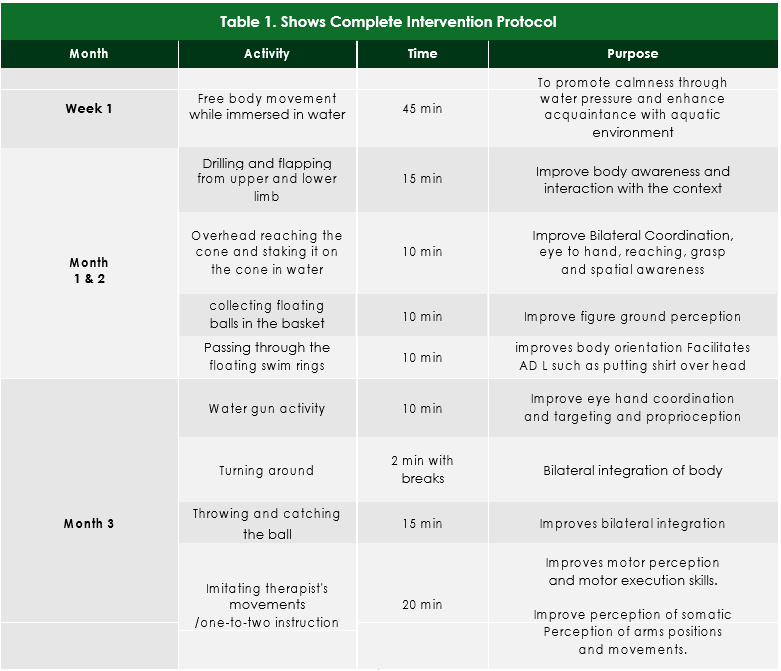
Intervention Protocol
In first week children in group of 6 were allowed to do free body movements in water pool bath tub swimming pool to reduce their anxiety and to make them familiar to it. In the following weeks, each time the session was started from 5 min free movements after which children were engaged in purposeful movements commanded by occupational thera-pists. The activities in water are designed according to purposeful movement. The following 2 months were intended to improve the body awareness, coordination and body orientation. The 3rd month works upon proprioception, bilateral integration and motor skills. The 4th month was designed to reduce repetitive movements, and improve kines-thesia, visuopraxis, and auditory feedback. The 5th month work on playing skills, interaction, and converting verbal commands into action, whereas the last 6th month improve motor planning that incorporated with daily activities, complete intervention protocol described in Table 1.
Data Analysis
Data was analyzed on SPSS version 20 Pre and Post analysis was determined by using paired t-test. Level of significance was calculated at 95% CI, p-value of < 0.05 was considered significant
Ethical Consideration
Consent form from parents was taken before the study to acknowledgment of all the risk during the study and to provide assurance of confidentiality. Data collection and intervention in the hospital was done after taking permission from Head of depart-ment.
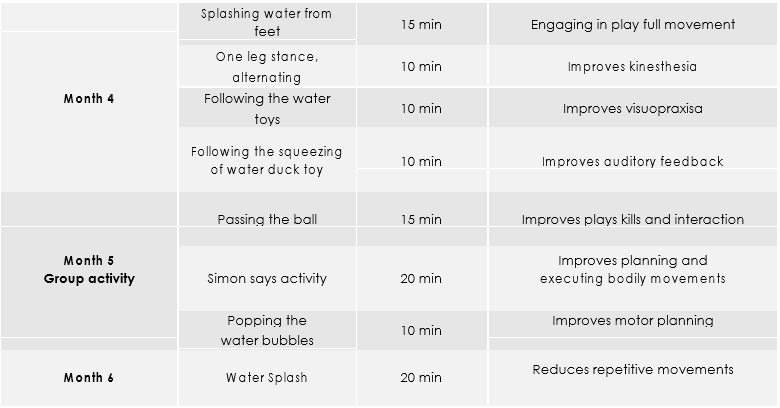
A total of 56 participants within an age group of 5 to 8 years were recruited in the study. The baseline characteristics of the participants has revealed that at baseline the mean FIM score was 61.58 ± 9 and short sensory profile scoring was 51.48 ±11.10. The male and female proportion of the participants in the study was 69.6% and 30.3% respectively. (Table-2)
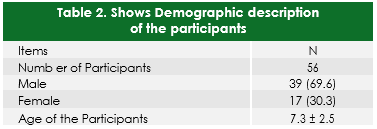
After six months of intervention the mean score of the participants measured at FEM and Sensory profile scale had increase to 66.8 ± 7.8 and 54.98 ±
- respectively (Table -3)
Paired t test analysis of the data revealed that after six month of interventional strategies based on structured exercises protocol the participants has shown a significant mean difference from the base-line where the value on the FEM score has improved from 61.58 ± 9 to 66.8 ± 7.8 with a mean difference of 5.22 ± 2.3 at 95% of CI (p= 0.02). The values on the short sensory profiles has also shown a significant mean difference from the baseline with a mean difference of 3.5 ±1.02 at 95% of CI (p=0.03) where the baseline values were 51.48 ± 9 and the values obtained at six months were 54.98 ± 11.22
The result of our study has revealed that aquatic therapy provides a positive effect in improving the Functional Independency and Sensory profile of children with Autistic spectrum disorder. The results were according to the study conducted by Alaniz ML in 2017 in which they had concluded that even a shorter duration of aquatic therapy had provided a significant results in improving the func-tion independency of the children’s, however their limitation was a small sample size23. In another study conducted in 2010 it was observed that aquatic based structured exercises therapy had prolific results in improving the kinesthesia and social skills of the participants after 10 weeks session19. Yilmaz et al14 has evaluated the motor perfor-mance through water based exercises observed that 10 weeks of hydrotherapy sessions improves motor skills among autism children where endur-ance, flexibility, speed, power balance and grip strength were improved Ennis et al18 in a research report concluded that 10 weeks hydrotherapy program with intention to increase strength and social skills has shown a significant improvement on WOTA (water orientation test) and peadiatric quali-ty of life Inventory (Peads-QL). Ballingtonet al report-ed in a Randomized Controlled trial performed on Cerebral palsy children reported a significant improvement on Gross motor functional scale among the participants whom were intervened on aquatic based exercises program in comparison to patient in the control group24. A pilot on children with autistic spectrum disorder was performed in group aquatic exercise therapy and its effects were compared with control group who were asked to do their routine schedules activity and it was found that children who were given intervention on aquatic exercises showed a significant improve-ment in swimming skills, following a 14 week of programme25.
The key strength of our study was that it was a first of its type in Pakistan that involved the aquatic based interventional strategy for the purpose of rehabilita-tion of autistic children that involved a sample size measured at 95% of CI with a 5% of bound of error. However the study have some weaknesses as well firstly the data was collected from single tertiary care hospital of Pakistan that may perhaps limits the generalizability of the methodology and second, the study include participants from the upper middle strata of society that may help in better understanding of the findings obtained among the children as the parents and the guardian were well aware with concepts of the intervention. The research however recommends that in future randomized controlled trials should be performed among in order to get further definite findings of the effects of aquatic therapy among the autistic population of Pakistan.
The study concluded that six months of aquatic based intervention strategies showed significant results in improving FIM and Short Sensory profile of children diagnosed with autistic spectrum disorder.
- Zablotsky B, Black LI, Maenner MJ, Schieve LA, Blumberg SJ. Estimated prevalence of autism and other developmental disabilities following ques-tionnaire changes in the 2014 National Health Interview Survey.
- Sinha P, Kjelgaard MM, Gandhi TK, Tsourides K, Cardinaux AL, Pantazis D, Diamond SP, Held RM. Autism as a disorder of prediction. Proceedings of the National Academy of Sciences. 2014;111(42):15220-5.
- Boulet SL, Boyle CA, Schieve LA. Health care use and health and functional impact of develop-mental disabilities among US children, 1997-2005. Archives of pediatrics &adolescent medi-cine.2009 ;163(1):19-26.
- Stone H. Sensory evaluation practices. Academic press; 2012 Aug 16.
- McCormick C, Hepburn S, Young GS, Rogers SJ. Sensory symptoms in children with autism spec-trum disorder, other developmental disorders and typical development: a longitudinal study.2016 ;20(5):572-9.
- Wigham S, Rodgers J, South M, McConachie H, Freeston M. The interplay between sensory processing abnormalities, intolerance of uncer-tainty, anxiety and restricted and repetitive behaviours in autism spectrum disorderJ Autism 2015;45(4):943-52.
- Green D, Charman T, Pickles A, Chandler S, Loucas T, Simonoff E, Baird G. Impairment in movement skills of children with autistic spectrum disorders. Developmental Medicine & Child Neurology. 2009;51(4):311-6.
- Teresa Garland MO. Self-Regulation Interventions and Strategies: Keeping the Body, Mind & Emotions on Task in Children with Autism, ADHD or Sensory Disorders. PESI Publishing & Media; 2014 Feb 1.
- Little LM, Sideris J, Ausderau K, Baranek GT. Activity participation among children with autism spec-trum disorderAm J Occup Ther. 2014;68(2):177-85.
- Obrusnikova I, Miccinello DL. Parent perceptions of factors influencing after-school physical activity of children with autism spectrum disorders. Adapt-ed Physical Activity Quarterly. 2012 ;29(1):63-80.
- Lee J, Porretta DL. Enhancing the motor skills of children with autism spectrum disorders: A pool-based approach. Journal of Physical Educa-tion, Recreation & Dance. 2013;84(1):41-5.
- Yanardag M, Akmanoglu N, Yilmaz I. The effec-tiveness of video prompting on teaching aquatic play skills for children with autism. Disability and rehabilitation. 2013;35(1):47-56.
- Chandolias K. Evanthia C PapadopoulouAlexan-dra H (2018) The Effect of Hydrotherapy-Halliwick Concept on the Respiratory System of Children with Cerebral Palsy. BAOJ Pediat.;4:063.
- Tripp F, Krakow K. Effects of an aquatic therapy approach (Halliwick-Therapy) on functional mobility in subacute stroke patients: a random-ized controlled trial. Clinical rehabilitation. 2014;28(5):432-9.
- Franzen K, Tryniszewski P. Effectiveness of aquatic therapy for children with neurodevelopmental disorders: A systematic review of current literature (Doctoral dissertation, Sage Colleges).
- Yanardag M, Akmanoglu N, Yilmaz I. The effec-tiveness of video prompting on teaching aquatic play skills for children with autism. Disability and rehabilitation. 2013 ;35(1):47-56.
- Mortimer R, Privopoulos M, Kumar S. The effective-ness of hydrotherapy in the treatment of social and behavioral aspects of children with autism spectrum disorders: a systematic review. J Multidiscip Healthc. 2014;7:93.
- Ennis E. The effects of a physical therapy-directed aquatic program on children with autism spec-trum disorders. Journal of Aquatic Physical Thera-py. 2011;19(1):4-10.
- Pan Effects of water exercise swimming program on aquatic skills and social behaviors in children with autism spectrum disorders. Autism. 2010 ;14(1):9-28.
- Davis AM, Bruce AS, Khasawneh R, Schulz T, Fox C, Dunn W. Sensory processing issues in young children presenting to an outpatient feeding clinic: A retrospective chart review. Journal of pediatric gastroenterology and nutrition. 2013 ;56(2):156.
- Lane AE, Molloy CA, Bishop SL. Classification of Children With A utism S pectrum D isorder by Sensory Subtype: A Case for Sensory‐Based Phenotypes. Autism Research. 2014 ;7(3):322-33.
- Park EY, Kim WH, Choi YI. Factor analysis of the WeeFIM in children with spastic cerebral palsy. Disability and rehabilitation. 2013 ;35(17):1466-71.
- Alaniz ML, Rosenberg SS, Beard NR, Rosario ER. The effectiveness of aquatic group therapy for improving water safety and social interactions in children with autism spectrum disorder: a pilot program. Journal of autism and developmental disorders. 2017;47(12):4006-17.
- Ballington SJ, Naidoo R. The carry-over effect of an aquatic-based intervention in children with cerebral palsy. Afr J Disabil .2018;7:1-8.
- Fragala-Pinkham MA, Haley SM, O’Neil ME. Group swimming and aquatic exercise programme for children with autism spectrum disorders: a pilot study. Developmental Neurorehabilitation. 2011 14(4):230-41.
