ABSTRACT
BACKGROUND & AIM
The body of evidence related to higher incidence of breast cancer related lymphedema after breast surgeries concluded compromise Quality of Life (QoL) among women over the past decade. The aim of this study is to evaluate the effectiveness of Manual Lymphatic Drainage (MLD) in improving QoL among women with Breast cancer related Lymphedema.
STUDY DESIGN & PARTICIPANTS
A Quasi Experimental study was conducted on women of the age 36-60 years with stage I and II breast cancer related lymphedema at Rehabilitation Department of a tertiary care Hospital.
METHODS
Total 70 women recruited with lymphedema were assessed at base-line and after treatment on Lymphedema Life Impact Scale. Manual lymphatic drainage technique was applied for 3 days in a week for 6 weeks with a compression bandage for first 4 weeks.
RESULTS
The findings showed that Manual Lymphatic Drainage (MLD) tech-nique significantly improves the Lymphedema Life Impact Scale score after intervention p <0.05 notably in psychological domain of the scale p=0.0001 furthermore, the percentage of impairment was also reduced significantly from 75.98% to 44.18%.
CONCLUSION
MLD is found to be more effective treatment for improving the overall Quality of Life among women with Breast cancer related lymphedema
KEYWORDS
Manual Lymphatic Drainage (MLD), Quality of Life (QoL), Breast Cancer, Compression Bandage, Impairment, Lymphedema Life Impact Scale.
Nazia Iqbal
Physiotherapist
Ziauddin Hospital
Hussaini Begum
Senior Physiotherapist
Darul Sehat Hospital
Amanullah Khan
Physiotherapist
PNS Shifa Hospital
[Iqbal N, Begum H, Khan A. Effec-tiveness Of MLD in Improving QoL Among Women With Breast Cancer Related Lymphedema Pak. j. rehabil. 2018;7(2);38-44]
Globally, the most frequent malignancy among women is breast cancer1, which is accounted as 23% of all the cases and its frequency is increasing day by day2. In 2002, the incidence of breast cancer worldwide was estimated 1.1 million; 641,600 cases were reported more in developed countries and 509,700 reported in less developed countries. Due to breast cancer, the death rate was found higher in under developed countries3. In Korea over the past 14 years there has been 3.3% of population is diagnosed with Breast Cancer but the mortality rate has been reduced since the year 2002, while incidence and survival has improved because of great advances in treatment approaches4. While in Pakistan 1 in 9 females are diagnosed with breast cancer5.
According to Shaukat Khanum Memorial Cancer Hospital (the leading cancer care Hospital in Pakistan) statistics, 45.9% are women, out of which 21.5% are diagnosed with Breast Cancer. In 2010 Age-Standardized Incidence Rate (ASR) An annual report from Asia showed 69 per 1 lac women diag-nosed with breast cancer in Karachi South that is second highest in Asia. There is lack of cancer data registries region wise in Pakistan which makes it difficult to report the overall incidence of the disease in the country6.
Women who have underwent to breast cancer related treatment including surgeries, radiotherapy, chemotherapy or other hormonal therapies are at continuing risk of producing breast cancer related lymphedema7. It is an untreatable lifelong medical condition occurs due to damage in lymphatic system during treatment8.The lymphatic system fails to remove excess accumulation of protein rich fluid manifested as tissue swelling present in one or both arm9. The most common symptom experienced by women is arm swelling other include the warm extremity, heaviness, tightness, stiffness, tingling and restricted range of motion on shoulder, elbow, wrist and even small joints of fingers10.
The Quality of Life is severely compromised in women with unilateral arm lymphedema after breast surgery because the condition may cause significant psychological, physical, functional, and social morbidity thus downgrading Health Related Quality of Life. Physiological manifestations and loss of function in lymphedema is harder to hide by the patients. Lymphedema is more distressing than breast cancer surgery11-12. Therefore, an effort required to implement the effective treatment approach to minimize the psychological, physical and functional disturbances in women with breast cancer related lymphedema13-15.
Lymph edema Functioning, Disability and Health questionnaire (Lymph ICF) and lymphedema quali-ty of life (LYMQOL) are the widely available tools to assess the Quality of Life among lymphedema patients moreover, Lymphedema Life Impact Scale (LLIS) is a collective tool to inquire the incidence of infection, impairment and measurement of lymph-edema which is contributing significantly in examin-ing the participation restriction16.
The primary directing component for current standard therapeutic approaches in the manage-ment of lymphedema is Knowledge of anatomy and physiology of the lymphatic system. However, for more exploration in scientific world an improved understanding of the embryonic formation of the lymphatic system is also important in managing secondary lymphedema17.
There is no cure for this condition once established; the options available for alleviating the symptoms include drugs, surgery and conservative treatment including Complex Decongestive Therapy (CDT), Pneumatic Compression Therapy and Manual Lymphatic Drainage (MLD). Little evidence is also found on low dose laser Therapy but its efficacy is still questionable18.
Now a days, MLD has become popular in European countries for managing lymphedema. Gentle massage techniques are applied to cause lymphat-ic flow, thereby increasing the lymphatic drain-age19.
Therefore, the aim of this study is to provide the most effective treatment approach that may not only prevent or reduce the volume of limb but should also address psychological, physical and functional parameters of health-related Quality of life among women with unilateral arm lymphedema after treatment of breast cancer.
Study Design
Quasi Experimental Study
Sampling Technique Convenient Sampling Technique
Study Setting
The study was conducted in the Outpatient Depart-ment of Physical Therapy at a tertiary care hospital.
Target Population
Women with unilateral arm lymphedema and age range from 36 to 60 years were included after treat-ment of breast cancer.
Duration of Study
Six months
Sample Size
A Sample size of 70 has been selected using WHO Software.
Sample Selection
Inclusion criteria
Women of age 36-60 years with Breast cancer identified unilateral arm lymphedema. Stage I & II lymphedema.
Radiotherapy and chemotherapy sessions were completed before the study begins1.
Exclusion criteria
Bilateral arm Lymphedema.
Evidence of recurrence and metastases.
Infection in affected limb.
Heart and Renal insufficiency.
DVT in the upper limb1.
Interventional Strategies
The study was conducted on 70 females reported to Physiotherapy Department after breast cancer treatment. In first four week of treatment, Females receiving Manual Lymphatic Drainage followed by multilayered short-stretch compression bandaging with appropriate padding, each participant under-went 3 days for 4-week cycle. Then MLD continues for two more weeks without the bandage. All sessions consist of 45 to 60 minutes performed by a trained physiotherapist. The technique included three basic lymphatic drainage strategies that were Stationary circles, Rotary technique and Thumb Circle. The patients were called a total of three days per week for the duration of six weeks. The interven-tion includes following phases20-21.
Preparatory Phase
The preparatory phase included the detail descrip-tion of the intervention given to the patient also mentioned time given for wearing loose and com-fortable clothing. The purpose of preparatory phase was to provide ample time for self-acclimatized with the environment of treatment area.
Treatment Phase
This phase comprised of three different treatment strategies that were given to the patient in a single session.
Stationary Circles
The technique involved the use stationary circle technique of massage to be applied to the patient using elbow. The therapist applied the massage on the neck and shoulder area of the patient. Zero phase strategy was used to induce lymphatic drain-age. For Zero phases the therapist hands were in complete contact with the patient body with full stretch and light touch. Stationary circles massage was given for the duration of 10 to 15 minutes.
Rotary Technique
The technique was applied on flat body surface such as on the back of the patient. It was a two-handed technique in which therapist applied massage in the oval direction parallel to the spine the technique of zero phase was applied to make patient feel comfortable and relax during treat-ment. Rotary technique was applied for the dura-tion of 15-20 minutes.
Thumb Circles
Thumb circles were provided on the periphery of the patient. The massage was given towards the direction of drainage; thumb movement during the therapy was spirally in direction towards the center of the body, the technique was given for the dura-tion of 10 minutes.
Outcome Measure Lymphedema Life Impact Scale
The scale was based on Physical, psychological and Functional Concern of the patient. It is a Likert scale comprised of 18 items divided into three cate-gories. The patient were asked to complete the scale twice once before the start of the session and second after the completion of six weeks of the session. The intraclass correlation coefficient value for this scale was calculated 0.687 and Cronbach α coefficient for internal consistency were recorded as 0.84716.
Data analysis
For storage purpose, Data were entered in Excel 2016 spreadsheets. Further, the Statistical Analysis was done on SPSS software, version 20.
Data were first described in terms of percentage, mean and standard deviation. However, inferential analyses were performed using Paired T-test, for the lymphedema life impact scale variables, in order to compare the pre-post analysis within the group.
Ethical Considerations
The study was ethically approved by Hospital Ethical Committee. Informed consent was obtained from all participants before enrolling into the study and the data was kept confidential and secure.
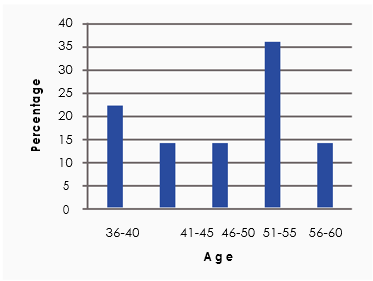
A total of 70 females included in the study had developed lymphedema after mastectomy (n=56) and axillary lymphadenectomy (n=14) illustrated in figure-1. The participants mean age was 49.6±1.9, whereas most of the lymphedema cases were seen in the age range of 51-55 (36%) and 36-40 (22%). The age-wise distribution of the participants is shown in figure-2.
Figure 1. showing the type of Breast Surgeries
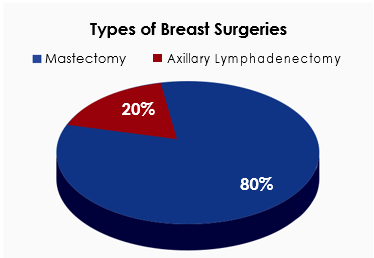
Figure 2. showing the Distribution of Age
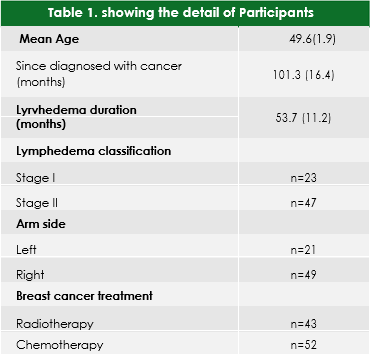
At baseline, most of the participants (n=49) report-ed left sided lymphedema whereas (n=21) partici-pants had right sided lymphedema. However, maxi-mum of the cases (n=47) were presented with stage-II lymphedema classification. Detailed information of participants characteristics are represented in table-1.
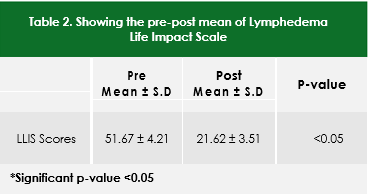
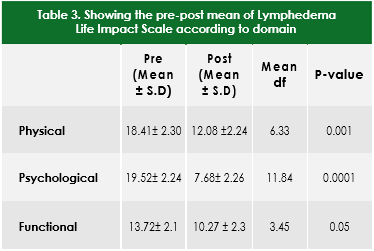
After intervention for the duration of 6 weeks’ signifi-cant improvement (P<0.05) was observed in overall Quality of Life among women participated in the study, the outcome measure was assessed using Lymphatic Life Impact Scale both at baseline and after intervention. (table-2)
The domain wise pre and post mean values of LLIS are depicted in table 3, the results indicated that there is highly significant reduction was recorded in psychological domain after Manual
Lymphatic Drainage (p<0.05) with a mean differ-ence of 11.84. The mean difference of each domain is shown in table 3.
The severity of impairment was calculated by impairment score calculator, there were statistically significant improvement reported by the partici-pant after 6 weeks of Manual Lymphatic Drainage. The graphical representation of percentage differ-ence at baseline and after intervention is represent-ed in figure 3.
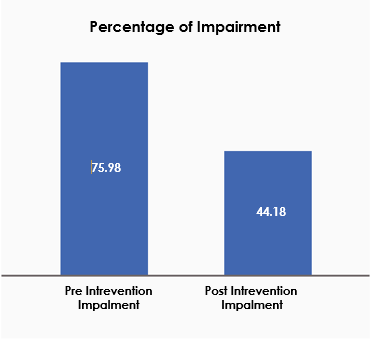
Figure 3. showing the Percentage of Impairment before and after treatment
This study evaluated the effectiveness of manual lymphatic drainage in improving the Psychological, physical and functional domains of lymphedema life impact scale among women with breast cancer related lymphedema and attended the Rehabilita-tion Clinic at tertiary care Hospital in Karachi. After 6 weeks of intervention, the result suggests that Manual lymphatic drainage technique was found to be effective in improving the patient perception towards Lymphedema life impact scale. The three domains of the scale that are physical, psychologi-cal and functional were improved significantly. Our finding shows that the risk of lymphedema may increase after 50 years of age similarly one study conducted in 2014, revealed that the risk of lymph-edema is found to increase 3.3 times in women more than 50 years of age with the reason unknown22. On the contrary, another study concluded that lymphedema is more prevalent among young adult women with obesity in com-mon23.
According to our baseline assessment, most of the women had undergone mastectomy. Left sided arm edema was found significantly with stage II lymphedema. The psychological well-being of the participant were significantly improved with 6-weeks of MLD with P=0.0001.
Previous studies showed the effectiveness of MLD in addressing Quality of Life in lymphedema among systemic sclerosis, reflex sympathetic dystrophy, and psoriatic arthritis patients furthermore, in fibromyalgia syndrome it reduces pain threshold and intensity thus, improves the overall QoL and disability24. Our findings also support these results among breast cancer related lymphedema women by reducing the scores of Lymphedema life impact scale after 6-week of intervention with com-pression bandage (p<0.05).
Williams and Szolnoky et al in a study conducted on patient having greater than 10% of volume differ-ence in the circumference of the arm among patient age 63 and above revealed that Manual lymphatic drainage technique applied for three weeks significantly reduced the lymph circumfer-ence25-26. However, a meta-analysis conducted on the effects of manual lymphatic drainage on the breast cancer patient suggested that manual lymphatic drainage alone did not provide signifi-cant result in the management of lymphatic drain-age27.
According to the results of our study we found that Manual Lymphatic drainage techniques effectively reduced the lymphedema of the effected limb, 45-60 minutes of session given to the patient based on three different lymph drainage techniques improved the patient perception towards devel-oped lymphedema, however other studies also suggested that no such significant difference in term of reduction of circumference has been noticed while applying the Manual Lymphatic drainage technique alone. Jeanette Ezzo et al in 2016 revealed that MLD with standard physiothera-py does not reduce the lymph circumference whereas MLD with compression bandage reduces 30% to 38.6% post treatment28.
A study conducted by Sheila H et al in 2013 MLD alone is beneficial in reduction of volume however alone it was a time consuming process and that if the technique used in conjunction with other physi-cal therapy management approached the same result could be achieved much earlier29. Similarly, it was also evident from researches that Manual lymphatic drainage effectively reduced the volume of the underlying lymph but the technique in combination with other approaches like Low level laser therapy could turn out to be more effective30. Further in two studies the incidence of lymphedema was determined among breast cancer patients who underwent manual lymphatic drainage and it was found that a high relative risk 0.63 was found with the reoccurrence occur in just 1 to 3 months after the completion of the session that suggested that weak long term effect of the effect of the tech-nique in the management of lymphedema31-32.
The finding of our study was in consistent with the finding of the study conducted in the various time periods however authors believed that more studies in this regards are required for further confirmation of the findings. Our study had some limitations six weeks of training protocol with the frequency of three days per week was not fully appropriate for measuring the acute effects of the therapy minimum 5 to 6 days per week of intervention is required but MLD is an expensive treatment proto-col as well as there was no follow-up to check the prolong effects of MLD. Furthermore, MLD can only be provided by trained physiotherapist that may limit the intervention done in any other setting. Due to lack of time the study was done in a single hospi-tal. Moreover, for the purpose of the generalizability of the methodology equipped lab with trained personnel is required along with the collection of data from multiple physical therapy setups is also needed therefore authors recommend a large scale study with bigger effects size to be done in order to get more preciseness in the results.
The strength of the study includes use of standard scale which can evaluate the Quality of life as well as determine the impairment level among the participants.
Hence, the favorable effects of Manual Lymphatic Drainage in the improvement of psychological, physical and functional component of Lymphatic life impact scalewhich ultimately improve the Quali-ty of Life among women with breast cancer related lymphedema. This allows us to assume that MLD is an effective method complementing the methods of lymphedema treatment that have been used till now.
Our study concluded that six weeks of Manual Lymphatic drainage was found to be effective in improving the Quality of life among women with breast cancer related lymphedema measured on Lymphedema Life Impact Scale furthermore, it is also helpful in decreasing impairment among the population. Future researches are still required to get more concrete results.
- Martín ML, Hernández MA, Avendaño C, Rodrí-guez F, Martínez H. Manual lymphatic drainage therapy in patients with breast cancer related lymphoedema. BMC cancer. 2011;11(1):94.
- Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA: a cancer journal for clinicians. 2011;61(2):69-90.
- Ferlay J, Héry C, Autier P, Sankaranarayanan R. Global burden of breast cancer. InBreast cancer epidemiology 2010 (pp. 1-19). Springer, New York, NY.
- Jung KW, Won YJ, Kong HJ, Oh CM, Cho H, Lee DH, Lee KH. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2012. Cancer research and treatment: official journal of Korean Cancer Association. 2015;47(2):127.
- Asif HM, Sultana S, Akhtar N, Rehman JU, Rehman RU. Prevalence, risk factors and disease knowledge of breast cancer in Pakistan. Asian Pac J Cancer Prev. 2014;15(11):4411-6.
- Badar F, Faruqui ZS, Uddin N, Trevan EA. Man-agement of breast lesions by breast physicians in a heavily populated South Asian developing country. Asian Pac J Cancer Prev. 2011;12(3):827-32.
- Taghian NR, Miller CL, Jammallo LS, O’Toole J, Skolny MN. Lymphedema following breast cancer treatment and impact on quality of life: a review. Critical reviews in oncology/hematol-ogy. 2014;92(3):227-34.
- Paskett ED, Dean JA, Oliveri JM, Harrop JP. Cancer-related lymphedema risk factors, diag-nosis, treatment, and impact: a review. Journal of Clinical Oncology. 2012;30(30):3726-33.
- DiSipio T, Rye S, Newman B, Hayes S. Incidence of unilateral arm lymphoedema after breast cancer: a systematic review and meta-analysis. The lancet oncology. 2013;14(6):500-15.
- Fu MR, Axelrod D, Cleland CM, Qiu Z, Guth AA, Kleinman R, Scagliola J, Haber J. Symptom report in detecting breast cancer-related lymphedema. Breast Cancer: Targets and Therapy. 2015;7:345.
- Maree JE. Yes, breast cancer related lymphoe-dema can be managed. Health SA Gesond-heid. 2011;16(1).
- Mwiinga-Kalusopa V, Ngoma C, Lishimpi K. Health related quality of life among breast cancer patients with unilateral arm lymphede-ma at cancer diseases hospital in Lusaka, Zambia. Journal of Cancer Research and Experimental Oncology. 2016;8(3):26-32.
- Togawa K, Ma H, Sullivan-Halley J, Neuhouser ML, Imayama I, Baumgartner KB, Smith AW, Alfano CM, McTiernan A, Ballard-Barbash R, Bernstein L. Risk factors for self-reported arm lymphedema among female breast cancer survivors: a prospective cohort study. Breast Cancer Research. 2014;16(4):414.
- Fu MR. Breast cancer-related lymphedema: Symptoms, diagnosis, risk reduction, and man-agement. World journal of clinical oncology. 2014;5(3):241.
- Testa A, Iannace C, Di Libero L, Caracciolo F. Strengths of early physical rehabilitation programs in surgical breast cancer patients: results of a randomized control study. InBMC proceedings 2013 (Vol. 7, No. 1, p. O5). BioMed Central.
- Weiss J, Daniel T. Validation of the Lymphede-ma Life Impact Scale (LLIS): a condition-specific measurement tool for persons with lymphede-ma. Lymphology. 2015;48(3):128-38.
- Ridner SH. Pathophysiology of lymphedema. InSeminars in oncology nursing 2013 (Vol. 29, No. 1, pp. 4-11). WB Saunders.
- Fu MR. Breast cancer-related lymphedema: Symptoms, diagnosis, risk reduction, and man-agement. World journal of clinical oncology. 2014;5(3):241.
- Huang TW, Tseng SH, Lin CC, Bai CH, Chen CS, Hung CS, Wu CH, Tam KW. Effects of manual lymphatic drainage on breast cancer-related lymphedema: a systematic review and meta-analysis of randomized controlled trials. World journal of surgical oncology. 2013;11(1):15.
- Crisóstomo RS, Candeias MS, Armada-da-Silva PA. Venous flow during manual lymphatic drainage applied to different regions of the lower extremity in people with and without chronic venous insufficiency: A cross-sectional study. Physiotherapy. 2017;103(1):81-9.
- Roth C, Stitz H, Roth C, Ferbert A, Deinsberger W, Pahl R, Engel H, Kleffmann J. Craniocervical manual lymphatic drainage and its impact on intracranial pressure–a pilot study. European journal of neurology. 2016;23(9):1441-6.
- Togawa K, Ma H, Sullivan-Halley J, Neuhouser ML, Imayama I, Baumgartner KB, Smith AW, Alfano CM, McTiernan A, Ballard-Barbash R, Bernstein L. Risk factors for self-reported arm lymphedema among female breast cancer survivors: a prospective cohort study. Breast Cancer Research. 2014;16(4):414.
- de Oliveira MM, Gurgel MS, Amorim BJ, Ramos CD, Derchain S, Furlan-Santos N, dos Santos CC, Sarian LO. Long term effects of manual lymphatic drainage and active exercises on physical morbidities, lymphoscintigraphy parameters and lymphedema formation in patients operated due to breast cancer: A clinical trial. PloS one. 2018;13(1):e0189176.
- Bongi SM, Del Rosso A, Passalacqua M, Miccio S, Cerinic MM. Manual lymph drainage improv-ing upper extremity edema and hand function in patients with systemic sclerosis in edematous phase. Arthritis care & research. 2011;63(8):1134-41.
- Williams AF, Vadgama A, Franks PJ, Mortimer PS:A randomized controlled crossover study of manual lymphatic drainage therapy in women with breast cancer-related lymphoedema. Eur J Cancer Care. 2002, 11: 254-261. 10.1046/j.1365-2354.2002.00312.x.
- Szolnoky G, Lakatos B, Keskeny T, Varga E, Varga M, Dobozy A, Kemény L: Intermittent pneumatic compression acts synergistically with manual lymphatic drainage in complex decongestive physiotherapy for breast cancer treatment-related lymphedema. Lymphology. 2009, 42: 188-194.
- Huang TW, Tseng SH, Lin CC, Bai CH, Chen CS, Hung CS, Wu CH, Tam KW. Effects of manual lymphatic drainage on breast cancer-related lymphedema: a systemat-ic review and meta-analysis of randomized controlled trials. World journal of surgical oncology. 2013;11(1):15.
- Ezzo J, Manheimer E, McNeely ML, Howell DM, Weiss R, Johansson KI, Bao T, Bily L, Tuppo CM, Williams AF, Karadibak D. Manual lymphatic drainage for lymphede-ma following breast cancer treatment. The Cochrane database of systematic reviews. 2015(5):CD003475.
- Ridner SH, Poage-Hooper E, Kanar C, Doersam JK, Bond SM, Dietrich MS. A pilot randomized trial evaluating low-level laser therapy as an alternative treatment to manual lymphatic drainage for breast cancer-related lymphedema. InOncology nursing forum 2013 (Vol. 40, No. 4). NIH Public Access.
- Omar MT, Ebid AA, El Morsy AM. Treatment of post-mastectomy lymphedema with laser therapy: double blind placebo con-trol randomized study. Journal of Surgical Research. 2011;165(1):82-90.
- Devoogdt N, Christiaens MR, Geraerts I, Truijen S, Smeets A, Leunen K, Neven P, VanKampen M. Effect of manual lymph drainage in addition to guidelines and exercise therapy on arm lymphoedema related to breast cancer: randomised con-trolled trial. Bmj. 2011;343:d5326.
- Lacomba MT, Sánchez MJ, Goñi ÁZ, Merino DP, del Moral OM, Téllez EC, Mogollón EM. Effectiveness of early physio-therapy to prevent lymphoedema after surgery for breast cancer: randomised, single blinded, clinical trial. Bmj. 2010;340:b5396.
