ABSTRACT
BACKGROUND AND AIM
Early mobilization practices in critical care settings are safe, effica-cious and evidently proven treatment to reduce morbidity as well as mortality. Inactivity adversely affects pulmonary and cardiovascular systems. Despite of widely available evidences, barriers to early mobilization still exist in critical care settings. Hence the present study aims to identify the barriers related to early mobilization perceived by physiotherapist in critical care settings.
METHOD
A cross-sectional survey among 99 physiotherapists working in a critical care setting of different tertiary care hospitals of Karachi, Pakistan was conducted in which a self-administered questionnaire related to perceived barriers for early mobilization was introduced.
RESULTS
The descriptive statistics revealed that 87% of physician requisition is required for mobilization, 74% response rate was received by PT for unawareness to identify the suitable patient for early mobilization, and 68% showed lack of staffing resources. 56% response rate was received regarding requirement of adequate training to facilitate early mobilization. Moreover, lack of decision making and safety concerns were 68% respectively.
CONCLUSION
Perceptions received by physical therapist reveals that the barriers identified should be considered important in the tertiary care hospi-tals as mobilization is found to be potentially beneficial in improving patients’ functional outcomes. It is recommended to conduct further studies in future that can evaluate the role of knowledge transformation in modifying these barriers.
KEYWORDS
Early mobilization, patients, Intensive care, Ambulation, Physical therapy Barriers, Perception, Critical care, Consequences of Bed-Rest, Mechanical ventilation
Saima Ali
Physiotherapist
Aga Khan University Hospital
Muhammad Ather Hashmi
Lecturer
Ziauddin College of Rehabilitation Sciences
Ziauddin University
[Ali S, Hashmi MA. Barriers to Early Mobilization in Critical Care Settings A Perception Based Survey among Physical Therapist. Pak. j. rehabil. 2018;7(1):42-47]
It was the first time, in World War II, when early ambulation of hospitalized soldiers was introduced as an effort to accelerate their recovery and quick return to battlefields. In 1944, a number of confer-ences were held for the first time in history, on the issue of Bed Rest. Moreover, leading international journals published their editorial highlighting the complications of bed-rest and revealing the bene-fits of early mobilization. Consequently, the intensive care units were established, years later. An illustrat-ed report was published by University of Colorado in 1972 that focused on benefits of early mobilization in mechanically ventilated patients. It has clearly demonstrated the increased general strength and well- being of the patients as a result of physical activity1.
There are multifactorial causes of neuromuscular weakness. Overwhelmingly, the critical illness polyneuropathy and myopathy are well-known etiologies1. Moreover, inflammatory conditions like sepsis may be the cause of muscular dysfunction. Bed-rest is counted as another important etiology as various experimental studies claim 4% to 5% decline in muscular strength per week as well as reduction in bone mineral density and muscle mass2.
Early mobilization has direct impact in modifying the deleterious effects of bed rest by targeting muscle fiber, inflammatory markers and metabolism, both structurally and functionally3. Muscle activity plays a crucial role as an anti-inflammatory agent in inflam-mation mediated diseases by producing myokines4.
Adding to this, experiments proved that insulin resistance and microvascular-dysfunction devel-oped in healthy individuals just after 5 days of bed rest. Musculoskeletal is not the only system that is affected due to immobility. Instead, cardiopulmo-nary system is also badly affected by bed-rest result-ing in tachycardia, orthostatic hypotension, decrease in stroke volume, cardiac output and VO2 max. Moreover, prolonged recovery duration is required in these individuals to restore their baseline status after the termination of bed-rest.1
Another study was aimed to investigate the feasibili-ty of body weight supported treadmill training in critical patients in intensive care setting. A treadmill was customized to be used in medical and surgical ICU which was body weight supported. The feasibili-ty of treadmill training was estimated through eligibility, number of successful attempts of BWSTT, required man power, complication, number of patients that were unable to walk without BWSTT, level of satisfaction and anxiety during intervention. The study further reported that among 20 patients there was no unfavorable event occurred through-out 54 sessions in which all of the medical supportive equipment was kept connected. 74% patients were unable to ambulate without BWSTT5.
This study supported the use of BWSTT as it seems to be safe and facilitate the initiation of early ambula-tion in critically ill patients with severe muscle weak-ness5.
Patients’ admission to neurological ICUs makes them prone to multiple cognitive and physical disabilities and impairments, as well as high risk of mortality. Moreover, at several occasions certain clinical decisions are made despite their unpredict-able outcomes. Patients presenting with neurologi-cal conditions like Cerebrovascular Accident (CVA) and traumatic brain injury are restricted from mobili-ty due to their illness. Furthermore, certain barriers like invasive line, monitoring devices and initial bed rest due to therapeutic restriction, are unavoidable. Consequently, the effects of immobility are detri-mental. Diseases like Acute Respiratory Distress Syndrome prolong the length of stay in ICU which results in critical illness myopathies. Even at discharge patient has poor functional status. Poor outcomes of hospital stay including prolonged intubation, recurrent chest infections, delayed recovery and even, death, are associated with intensive care acquired weakness. The quality of life and functional status are severely compromised due to prolong ICU stay6.
A randomized control trial was conducted recruit-ing 150 patients with an ICU stay of 5 days or more. These patients had no neurological insult and were randomized to receive usual care or intervention. The patients in intervention group received inten-sive exercises in all levels of care including ICU, wards and OPDs. Participant were assessed using Six-minute Walk Test(6MWT), Timed Up and Go Test and the Physical Function in ICU Test on recruitment, ICU-admission, hospital discharge and at the intervals of 3, 6, and 12 months. The Short Form 36 Health Survey, version 2 (SF-36v2) and Assessment of Quality of Life (AQoL) Instruments were used for assessing Patient outcomes. There were no intra-group differences in hospital data and demo-graphic details, which includes acuity and length of stay (LOS) (Acute Physiology and Chronic Health Evaluation II score: 21 vs. 19; hospital LOS: 20 vs. 24 days). Primary out comes of 6MWT revealed no significant differences at the 12th month of hospital discharge. However, exploratory analyses demon-strated the rate of change over time and mean inter-group differences in 6MWT were greater in the intervention group comparing to initial assessment7.
A prospective study with duration of four weeks was conducted on 106 patients, admitted in ICU. The variables focused in this study were total patients enrolled, frequency and type of mobilization, and the reasons for keeping the patient immobile. The result showed that there are many potential barriers which are avoidable like vascular access device in femoral region, timings of different procedures and agitation or reduced level of consciousness. It was concluded that intervention to enhance mobiliza-tion in ICU are careful management of proce-dures-schedule, site of catheter insertion and seda-tion protocol development8.
A cross sectional survey research was conducted among the ICU physicians and physiotherapist in Canada. It was a perception based postal survey which was self-administered. The results of the study revealed the importance of early mobilization in the perception of participants and identified various notable barriers related to medical institutions, health care providers and patients. Furthermore, it notified significant gaps in the knowledge and skills of health care providers to handle complexities that might occur during the early mobilization, particu-larly, with patients receiving mechanical ventilator support, high and unplanned doses of sedative medications resulting in poor patient-cooperation, limited or over occupied staffing, unavailability of desired supporting equipment and lack of well-de-fined protocols9.
Similarly, a bi-national, multi-center, prospective cohort study conducted in 12 ICUs in Australia and New Zealand. Patients enrolled were likely be on ventilatory support for more than 48 hours and expected to be functionally independent previous-ly The outcome measures were assessed are as follow: mobilization during invasive ventilation, depth of sedation using the Richmond Agitation and Sedation Scale (RASS), co-interventions, days on mechanical ventilator, ICU-acquired weakness (ICUAW) at discharge from ICU, status at day 90, and 6-month functional recovery including return to work. Muscle strength using MRC scale was assessed in 94 out of 156 ICU survivors. MRC score is high in 48% patients with ICU acquired weakness who were mobilized while mechanically ventilated. Despite of these drastic results early mobilization was uncommon due to numbers of barriers; more than 50% of patients discharged from the ICU had developed ICU-acquired weakness10.
Conclusively, the significance of early mobilization has been clearly established under provided evidences. Therefore, the present study aimed to investigate and identify the possible barriers to the early mobilization in critical care setting of tertiary care hospitals of Karachi in accordance with the perceptions of physical therapy professionals.
Research Design
The aims of study were achieved through descrip-tive analysis. The study was investigative and discussed the opinions and perceptions of partici-pants among the study group. Therefore, it was primarily a survey based study.
Sampling Technique
Random sampling was used thus the participants were selected randomly from tertiary care hospitals.
Sample Size
The sample size was 100.
Inclusion Criteria
- Physiotherapist from tertiary care hospitals having different types of intensive care units
- Physiotherapists who are working as inpatient therapist.
Exclusion Criteria
- Physiotherapist working in outpatient
- Physiotherapist working as home based therapist
- Physiotherapist working in small hospitals having general services and no Intensive care units
Study Duration
The study duration was 6 months
Procedures
The survey study was conducted in Karachi Pakistan with participants from tertiary care hospitals.100 participants were selected randomly and question-naire was introduced. The questionnaire was consisted of three sections that had closed ended questions regarding perceived barriers in mobilizing critically ill adults at institutional level, health care provider level and patient level. All data was analyzed at SPSS version 20.
Data Analysis
The data, collected through questionnaires were assigned numbers and recorded on Microsoft Excel Database. All data was analyzed on SPSS 20.
Ethical Consideration
Ethical approval has been taken from the institu-tional review board of the concerned hospital settings before conducting the research. Moreover, an informed consent was given to the participants before completing the questionnaire.
Response rate and respondents:
99 respondents were responded to the survey ques-tionnaire of the research conducted within tertiary care hospitals of Karachi.
Perceived institutional barriers to early mobilization: Overall respondents perceived that with respect to institutional barriers, the most common barriers to early mobilization are physician order required for early mobilization (87%), need of proper guidelines and protocols (78%), insufficient equipment for mobilization (78%) and routine bed rest order in admission notes (68%).The least common institution-al barrier observed is that administrator perceived to be an expensive intervention (32%), as represent-ed in Fig.1 below.

Perceived health care provider related barriers to early mobilization:
Overall respondents perceived that with respect to health care provider related barriers; the most common perceived barriers are inability to recog-nize suitable patients for mobilization (74%), lack of decision making authority (68%) and safety concerns (68%).Furthermore, lack of adequate training that is needed to facilitate early mobiliza-tion is identified as significant barrier (56%). The least common perceived health care provider related barrier is lack of coordination to facilitate mobiliza-tion (53%), as demonstrated in fig.2.

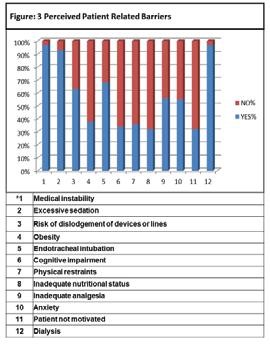
Perceived patient related barriers to early mobiliza-tion:
Overall response rate by respondents to perceive patient related barriers to early mobilization recom-mended that most common barriers are medical instability (97%), patient on dialysis (97%), excessive sedation (93%) endotracheal tube (68%), poor nutritional status (68%) and patient not motivated (68%).The least common patient related mobiliza-tion observed is inadequate nutritional status of patient (32%), as shown in figure.3.
Majority of our participants though consider impor-tance of early mobilization of critically ill patients but stated number of barriers at the levels of institution, healthcare provider and patients.
This type of study was not conducted yet in Pakistan, even though we have high level tertiary care hospitals in high numbers especially in all big cities of Pakistan. However, identification of barriers to early mobilization is the objective of recent international researches that identified multiple important domains to facilitate early mobilization and rehabilitation of mechanically ventilated patients11.
It was observed that the early mobilization did not seem to be of importance although being a health care provider, everyone aware about the compli-cations of bedridden status if kept without reason. International researches suggest that early mobiliza-tion should start as soon as the patient’s cardiopul-monary condition becomes stable. Early mobiliza-tion is considered as an integral aspect of multidisci-plinary focus in ICU routine practices. It begins as soon as physiological stability is attained by the patient that though varies throughout published studies but usually includes cardiovascular, respira-tory and neurological status12. Moreover, some clinicians consider endotracheal tube (ETT), vascu-lar access devices, or other equipment as the limita-tion to the feasible mobilization13. Conversely, 5 patients with ETT were reported to have participat-ed in 593 activities by a prospective cohort study, which ranged from sitting on the bed side up to complete ambulation14.
Similarly, there were no accidental extubation reported, despite the fact that all events involved ambulation. However, only a single incident of feed-ing tube dislodgment had occurred out of total 1449 events of physical activity. Furthermore, the same protocol was applied to a sample of 145 intubated patients and no incident of accidental equipment dislodgment was reported. Therefore, early mobilization is supported to feasible in ICU by these aforementioned studies15.
With respect to the institutional level barriers, the need of physicians’ order prior to mobilization was identified as the most observable barrier by the physiotherapists working in tertiary care hospitals of Karachi as they are considered secondary contact and need referral orders from the physicians. Physio-therapist were though trained and educated, yet they are unable to initiate early mobilization without the physicians’ consent. This concludes that further education in order to overcome the gaps in knowl-edge as well as technical skills is significant for emer-gency medicine facilitators in intensive cares.
Others less rated barriers but important ones are need of proper guidelines and protocols and sufficient equipment for mobilization16. Another study prompts to develop proper guidelines by which patients’ safety during early mobilization in ICUs of tertiary care hospitals will be promoted17.
A well-equipped healthcare team including mem-bers of varied disciplines and all necessary support-ing equipment such as portable ventilators, oxime-ter, bag-valve-mask with supplemental oxygen, suction devices and wheel chairs is essential to deliver safe physiotherapy treatment18.
The need of proper equipment should be consid-ered the most important factor for safety mobiliza-tion19. Therefore, unavailability of required equip-ment is also discussed as a significant barrier to mobilization of critical patient20. Provision of proper equipment by administration of hospital should be the main priority in hospitals.
Routine bed rest orders on admission paper are another barrier which should be reevaluated after patient becomes stable medically21.
Recent prominent studies highlighting improve-ments in functional outcomes and cost savings in prospective studies of early mobilization for critically ill patients have focused the awareness of ICU acquired weakness1, 22. Our survey demonstrates strong enthusiasm for early mobilization, particularly among physiotherapists and where mobility cham-pions exist. Mobility can also be limited by safety concerns, delays in the recognition of suitable patients, low prioritization for this aspect of care, poor inter-disciplinary communication and coordi-nation23.
Similar to other surveys, we found that excessive sedation medical instability were important patient related barriers to early mobilization24 . Sedation breaks should be given to the patient to access the patient conscious status through GCS scoring and evaluate the patient for mobilization if medical condition allowed.
Another important barrier is the dialysis25. The mutual understanding and communication between the ICU staffs is necessary so that the patient can be mobilizing during the period of off dialysis25. In Previ-ous study, the different barriers for mobilization were identified by physical therapists and nurses; hemo-dynamic instability and renal replacement therapy were barriers rated higher by nurses, whereas neurologic impairment was rated higher by physical therapists13.
Endotracheal tube is another major barrier which is identified but we can handle this barrier and through the good coordination and provision of champions in rehabilitation the mobilization of patient with ETT can be made possible26, 27.
An observational study was conducted, targeting the perceptions of physical therapist and nurses, regarding mobilization in intensive care units and barriers related to it. The study enrolled 63 critically ill patients, which were mobilized by both physiother-apist and nurses. The opinions of physical therapist and nurses appeared to be different in identifying the severity of the barriers that hurdle early mobiliza-tion of critically ill patients. Physiotherapists regard-ed neurological impairment as the higher barrier while the nurses identified renal impairment and hemodynamic instability as the major limitation for early mobilization28. The result outcomes demon-strated that the physical therapists are more involved in the mobilization and rehabilitation of their critically ill patients. Therefore, the role of physi-cal therapist in the rehabilitation and mobilization of critical patient is integral13.
Our research suggests that there are many barriers identified at institutional level, health care provider and patient related barriers. However, a great number of these identified barriers can be modified and manipulated through different techniques suggested earlier. Consequently, it implies that the need of further studies still persist in order to investi-gate these barriers more specifically, in the future. Moreover, future researches should focus on the development of strategies and protocols that ensure safe early mobilization despite these poten-tial barriers, especially in Pakistani context.
- Needham DM. Mobilizing patients in the intensive care unit: improving neuromuscular weak-ness and physical function. JAMA. 2008;300(14):1685-1690
- Parry SM, Puthucheary ZA. The impact of extended bed rest on the musculoskeletal system in the critical care environment. Extrem Physiol Med. 2015;4(16)
- Kress JP, Hall JB. ICU-acquired weakness and recovery from critical illness. N Engl J Med. 2014;370(1):1626-35
- Benatti FB, Pedersen BK. Exercise as an anti-in-lammatory therapy for rheumatic diseas-es-myokine regulation. Nat Rev Rheumatol. 2015;11(1):86-97
- Sommers J, Wieferink DC, Dongelmans DA, Nollet F, Engelbert RHH, Schaaf MVD. Body weight-supported bedside treadmill training facilitates ambulation in ICU patients: An interventional proof of concept study. Crit Care. 2017;41(1):150-155
- Creutzfeldt CJ, Hough CL. Get out of bed: immobility in the neurologic ICU. Crit Care Med. 2015;43(4):926-927.
- Denehy L, Skinner EH, Edbrooke L, Haines K, Warrilow S, Hawthorne G, et al. Exercise rehabili-tation for patients with critical illness: a random-ized controlled trial with 12 months of follow-up. Crit Care 2013;17(4)R156
- Leditschke IA, Green M, Irvine J, Bissett B, Mitch-ell IA. What are the barriers to mobilizing inten-sive care patients? Cardiopulm Phys Ther J. 2012;23(1):26-29.
- Koo KK, Choong K, Cook DJ, Herridge M, Newman A, Lo V, et al. Early mobilization of critically ill adults: a survey of knowledge, perceptions and practices of Canadian physi-cians and physiotherapists. CMAJ Open. 2016;4(3):448-454
- Berney SC, Harrold M, Webb SA, et al intensive care unit mobility practices in Australia and New Zealand: a prevalence study. Crit care resuac 2013;15(4)260-265
- Francis JJ, Duncan EM, Prior ME, MacLennan G, Marshall AP, Wells EC et al. Comparison of four methods for assessing the importance of attitu-dinal beliefs: An international D elphi study in intensive care settings. British journal of health psychology. 2014;19(2):274-91.
- Morris PE, Goad A, Thompson C, Taylor K, Harry B, Passmore L, et al. Early intensive care unit mobility therapy in the treatment of acute respi-ratory failure. Crit Care Med. 2008;36(8):2238-43.
- Garzon-Serrano J, Ryan C, Waak K, Hirschberg R, Tully S, Bittner EA, et al. Early mobilization in critically ill patients: patients’ mobilization level depends on health care provider’s profession. PM & R. 2011;3(4):307-313
- Truong AD, Fan E, Brower RG, Needham DM. Bench-to-bedside review: mobilizing patients in the intensive care unit – from pathophysiology to clinical trials. Crit Care. 2009;13(4):216.
- Bailey P, Thomsen GE, Spuhler VJ, Blair R, Jewkes J, Bezdijan L, et al. Early activity is feasible and safe in respiratory failure patients. Crit Care Med 2007;35(1):139-45
- Zomorodi M, Topley D, McAnaw M. Developing a mobility protocol for early mobilization of patients in surgical or trauma ICU. Crit Care Res Pract. 2012;2012.
- Hodson CL, Stiller K, Needham DM, Tipping CJ, Harrold M, Baldwin CE, et al. Expert consensus and recommendations on safety criteria for active mobilization of mechanically ventilated critically ill adults. Crit Care. 2014;18(6):658. Available from: https://www.ncbi.nlm.nih.gov-/pmc/articles/PMC4301888/
- Hashem MD, Nelliot A, Needham DM. Early mobilization and rehabilitation in ICU: Moving back to the future. Resp. Care. 2016;61(7):971-979
- Adler J, Malone D. Early mobilization in the intensive care unit: A systematic review. Cardio-pulm Phys Ther J. 2012;23(1):5-13
- Wieczorek B, Ascenzi J, Kim Y, Lenker H, Potter C, Shata NJ. PICU Up!: Imacpt of a quality improvement intervention to promote early mobilization in critically ill children. Pediatr Crit Care Med. 2016;17(2):559-566
- Hoyer EH, Brotman DJ, Chan K, Needham DM. Barriers to early mobilization of hospitalized medicine patient. 2015;94(4):304-312
- Dubb R, Nydahl P, Hermes C, Schwabbauer N, Toonstra A, Parker AM. Barriers and strategies for early mobilization of patients in intensive care units. Ann. Am. Thorac. Soc. 2016;13(5):721-730
- Appleton RTD, MacKinnon M, Booth MG, Wells J, Quasim T. Rehabilitation within Scottish intensive care units: a national survey. JICS. 2011;12:221-227
- Jolley SE, Reggan-Baggs J, Dickson RP, Hough CL. Medical intensive care unit clinician attitudes and perceived barriers towards early mobilizations of critically ill patients: a cross sectional survey study. BMC Anesthesiol. 2014;14(1):84
- Wang YT, Haines TP, Ritchie P, Walker C, Ansell TA, Rayan DT, et al. Early mobilization on contin-uous renal replacement therapy is safe and may improve filter life. Crit Care. 2014;18(4):161
- Nydahl P, Ruhl AP, Bartoszek G, Rolf D, Silke F, Hans-Jurgen F, et al. Early mobilization of mechanically ventilated patients: a 1-day point prevalence study in Germany. Crit Care Med 2014;42:1178-86
- Harrold ME, Salisbury LG, Webb SA, Allison GT. Early mobilization in intensive care units in Australia and Scotland: a prospective, observa-tional cohort study examining mobilization practices and barriers. Crit. Care. 2015;19(1):336.
- Garzon-Serrano J, Ryan C, Waak K, Hi et al. Early mobilization in critically ill patients: patients’ mobilization level depends on health care provider’s profession. PM & R. 2011;3(4):307-313
