ABSTRACT
BACKGROUND
Stroke is one of the problems that can lead to either disability or death and this will increase the social and economic burden.
OBJECTIVE
To analyze the effects of motor relearning program (MRP) in comparison with other treatment technique on quality of life (QoL) among stroke patients
DATA SOURCES
This systematic review includes Randomized Controlled Trials (RCT) for patients suffering from stroke. The articles were retrieved from Google Scholar, research gate, HEC digital library, ProQuest, Iingenta and PubMed. Articles were also accessed from Journals.
STUDY SELECTION
Data belonged from 2000 to 2015 were included. RCTs that focus on motor relearning program or its task-oriented activity as rehabilitation program of stroke patients were included in this review.
RESULTS
Total 12 studies were included in this review with 378 patients. Among them, 191 had received MRP, whereas, 187 had received any other treatment technique for stroke rehabilitation. Analysis of Berg Balance Scale (BBS) and Barthel Index shows that studies favor MRP, while result is slightly insignificant (0.008) with BBS and not significant (0.67) for Barthel Index.
LIMITATIONS
RCTs used different outcome measurement tools, their items or scores. Multiple accessible RCTs with results of individual items of scales are negligible. More RCTs focusing on individual item of scales are needed to better assess the effects of MRP in comparison with other treatments by review studies.
CONCLUSION
Effect of MRP on Quality of Life is not significant from selected studies, after assessing BBS and Barthel Index.
KEYWORDS
Motor Relearning Program (MRP), Stroke, Quality of Life, Task-oriented Activity, Activities of Daily Living (ADL), Systematic Review
Ghazla Noor Nizami
Assistant Professor
Ziauddin College of Physical Therapy
Ziauddin University
Nazish Rafique
Senior Lecturer
Ziauddin College of Physical Therapy
Ziauddin University
[Nizami GN, Rafique N. Effect of Motor Relearning Program on Quality of Life among Stroke Patients: A Systematic Review. Pak. j. rehabil. 2016;5(2):4-18]
INTRODUCTION
Stroke or cerebrovascular accident occurs due to impairment of blood supply of brain and results in paralysis. Stroke can be either hemorrhagic or ischemic depending on the problem in blood vessels 1,2. Stroke is one of the problems that can leads to either disability or death and this will increase the social and economic burden. According to report of American Heart Association, approximately 01/19 deaths occurred due to stroke in 2010 in United States. Average estimation showed that one person got stroke every 40 seconds and one person died by stroke every 4 minutes3. 17.3 million death occurred due to cardiovascular diseases in 2008. Among them, 7.3 million deaths were from heart attacks and 6.2 million deaths were from stroke4. The global disease burden of disability- adjusted life years (DALYs) due to cardiovascular diseases was 10% in 20114. The contribution of stroke to global cardiovascular diseases burden was 29% in males and 33% in females4. Stroke is the main public health problem among developing countries of South Asia too5. In low-income and middle-income countries, it is one of the leading causes of disability4. Pakistan lies in lower middle income countries6. Stroke is also common in our population. However, unfortunately the studies that highlight National stroke burden are negligible7,8. The estimation given by the Pakistan Stroke Society about the incidence of stroke is about 250 for every 100000 population and furthermore, 350000 new patients are adding every year9. A study of 2003 shows that 596 stroke patients were registered in a known tertiary care hospital of Karachi during an interval of 22 months10.
Stroke not only affects the physical and mental state of patients but also have emotional and economic impact on their families11. It also affects the quality of life (QoL) of patients12. Motor impairment is the main and most common problem for stroke patients. As a result of that they have problem in accomplishing their activities of daily living and in mobility 13,14. A study of Portugal assessed life satisfaction of patients after two years of stroke. They stated that patients with impaired motor functions have lower life satisfaction level15. The goal of stroke rehabilitation is to achieve functional independence during activities of daily living, along with the improvement in balance, movement and walking 13,16. For this purpose, early physical therapy intervention is important for patients suffering from acute stroke. It will also help them in decreasing their disability and restoring movements 17,18. Hence, selection of appropriate interventions and rehabilitation techniques are very important for early and better recovery17. Different treatment techniques that can be used are the Bobath, the Brunnstrom and Rood, the Proprioceptive Neuromuscular Facilitation (PNF), the Motor Learning or Relearning Program. Motor Relearning Program (MRP) was proposed by Carr in 1980s. It focuses on active participation of patient13. These patients are capable to relearn the motor tasks that they were performing before stroke19. Physical therapists identify the problem in different individual tasks and then help the patient to learn them, through task specificity, task repetition, type of practice, type of feedback, retention testing20-22. There are four sequential steps in MRP: 1) identification of the missing performance components, 2) training using remedial exercises, 3) training using functional task components, 4) transfer of skills to functional task performance 20,21. Examples of those tasks are catching things, picking up objects, feeding, buttoning, wearing clothes, bathing, grooming in sitting or standing, balance, sit to stand, indoor walking, outdoor walking, stair climbing and so on 20,23,24. Different assessment tests and methods are used to assess the motor function, movements, strength, functional independence and quality of life of these patients. Some of them are Motor Assessment Scale (MAS), Sodring Motor Evaluation Scale (SMES), Functional Independence Measure (FIM), Berg Balance Scale (BBS), Barthel ADL Index, Instrumental Activities of Daily Living (IADL) test, Nottingham Health Profile (NHP), Fugl-Meyer Assessment (FMA) score, Timed Up and Go Test, modified Ashworth scale, Stroke Rehabilitation Assessment of Movements (STREAM) Scale, Purdue Pegboard test score, grip strength by Dynamometer, and more over 25-31.
The one of the main features of neurological rehabilitation is the application of theory of motor learning. Helm stated that literature is less about task related training to illustrate better neural plasticity and locomotion of stroke patients32. Furthermore, a study conducted on monkeys with brain ischemia, showed improved neural repair, regeneration, angiogenesis and neurological function in them after using motor relearning program33. Multiple studies or Randomized control trials (RCT) compared motor relearning program or any task-oriented activity with other interventions. This systematic review aims to analyze the effects of motor relearning program in comparison with other treatment technique on quality of life among stroke patients.
METHODOLOGY
Data Sources and Search Strategy
The literature was searched by reviewers using Google Scholar. The initial search was done by using keywords of Stroke, Motor Relearning program, Quality of Life. The articles were retrieved from Google Scholar, research gate, HEC digital library, ProQuest, Ingenta and PubMed. Articles were also accessed from Journals. Literature was searched from inception to 2015. We have used PRISMA guidelines.
Study Selection and Data Extraction
Searched literature was filtered by time frame. Data belonged from 2000 to 2015 were included. Eligibility criteria for the studies that were to be included in this review were Randomized Controlled Trials (RCT) for patients suffering from stroke. It included those studies who address motor relearning program as rehabilitation program. However, all 4 parts of motor relearning program or task-oriented activities were the main focus among all studies. We included RCTs comparing two types of interventions techniques, in that one would be MRP. The RCTs that compared motor relearning program or its any task-oriented activity with control group were also considered. Completely reviewed trials were addressed rather than summary of the articles. The quality of life was assessed through functional goals, activities of daily living, postural control, use of assistive devices, length of stay in hospital, physical mobility, and social interaction. Therefore, our outcome measures of interest were motor functions, quality of movement, functional independence, activities of daily living, social interaction, activities of arm or leg, sitting, standing, walking, Motor Assessment Scale (MAS), Barthel ADL Index, Berg Balance Scale, Ashworth scale, Sodring Motor Evaluation Scale (SMES). The assessment time or follow up can be varied in studies, such as 2 weeks, 6 weeks, 3 months, one year, or four years. The groups of all these studies that had received MRP or any task related MRP are considered as Experimental group. Those who received any treatment other than MRP are taken as Control group in this systematic review.
Quality Appraisal
Reviewers analyze the quality of data and risk of bias. They assessed the source of article, patient blindness, dropouts and intervention details.
Statistical Analysis
This systematic review was conducted to compare the outcomes of motor relearning program and other treatment technique using Review Manager (RevMan) Version 5.3 for windows (The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen). It was conducted to assess the common outcomes of studies. Heterogeneity among the studies was assessed using Cochrane’s Q test and I2. The mean difference of an outcome was calculated by the finding the difference between follow-up and baseline mean. Standard deviations (SD) for the mean differences were calculated using Cochrane Handbook for Systematic Reviews of Interventions34 and using 0.5 conservative correlation of coefficient (r) 35. Weighted mean difference was used for continuous outcomes at 95% confidence interval (CI). P-value <0.05 was considered as significant. Forest plots were plotted to show the analyses of common outcomes of interventions.
RESULTS
Study Selection
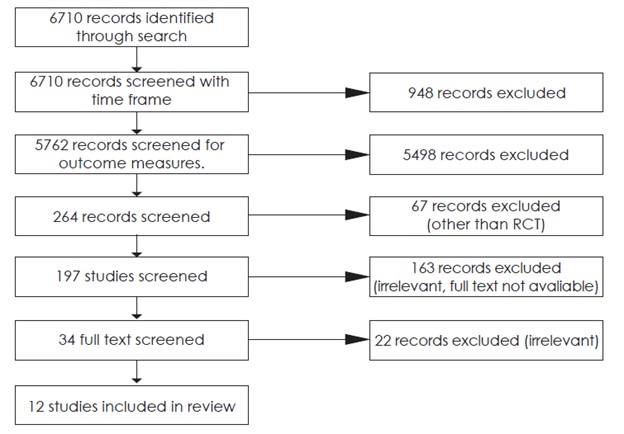
Initial search using keywords of Stroke, Motor Relearning program, Quality of Life, showed 6710 articles from beginning till 2015. This data was filtered by time frame that is from 2000 to 2015. The available data during this time frame was 5762 articles. This search was further narrow down by focusing on outcome measures, such as, motor functions, quality of movement, functional independence, activities of daily living, social interaction, activities of arm or leg, sitting, standing, walking, Motor Assessment Scale (MAS), Barthel ADL Index, Berg Balance Scale, Ashworth scale, Sødring Motor Evaluation Scale (SMES). The available data having any of these outcome measures was found 264. Excluding researches other than Randomized Control Trial (RCT), there were 197 citations. After reviewing the abstracts or titles, the researches that were found irrelevant, were excluded. Researches that found relevant from abstract but their full text was not available were also excluded from our review. 34 full texts were screened for final selection. When we selected and reviewed the study by Langhammer et al, published in 201124, we had to go through their previous studies published in 200025 and 200326. Due to the continuation of the same work, all reviewers decided to incorporate all these studies 24-26 in this review. Hence, total 12 studies were included in this review after the decision of all reviewers. Summary of study selection is shown in Figure 1.
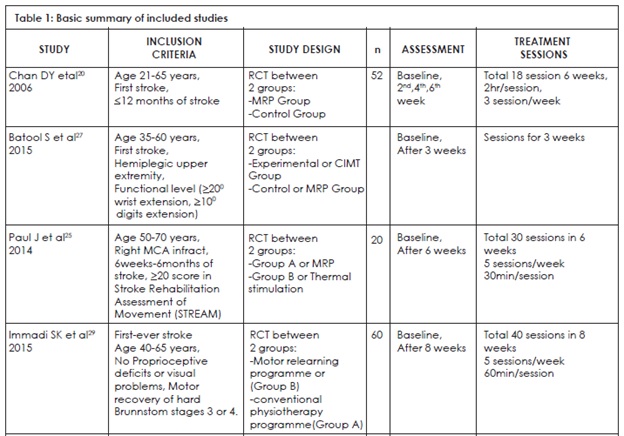
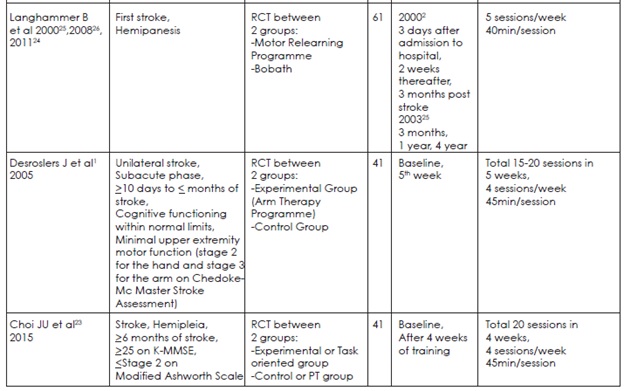
Study Characteristics
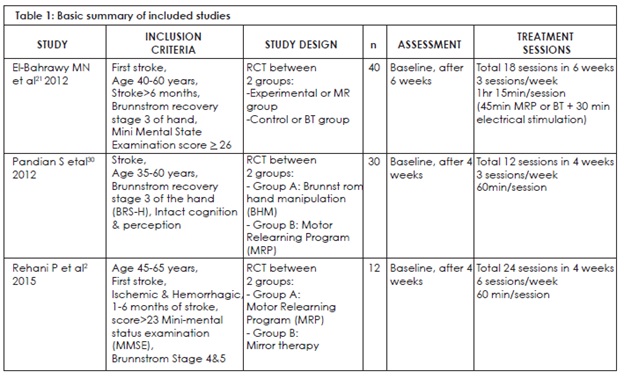
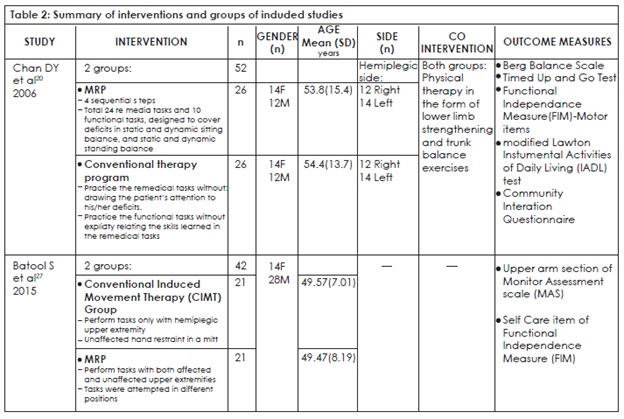
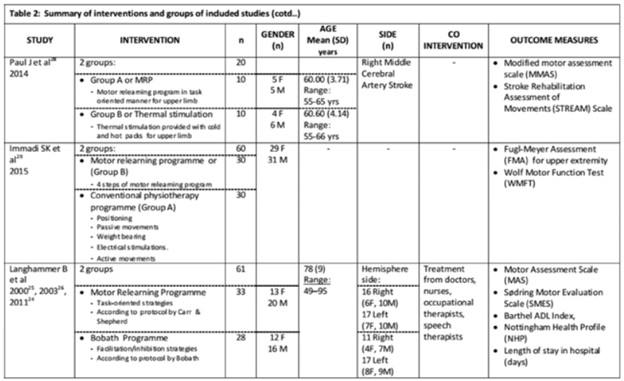
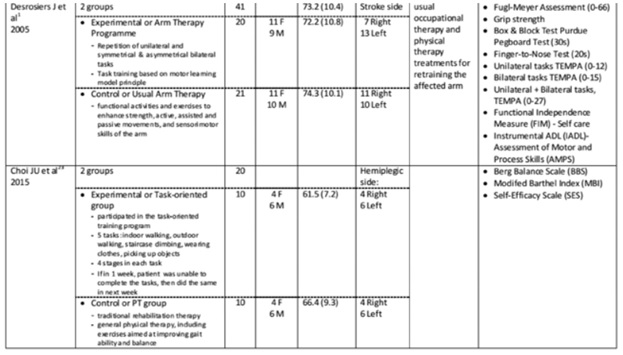
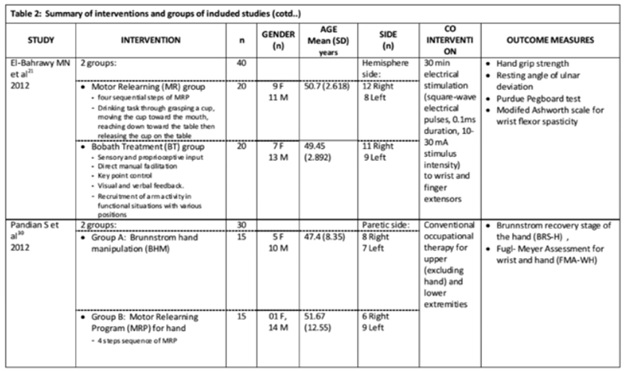
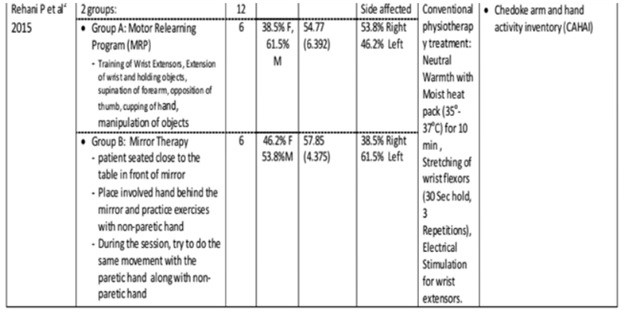
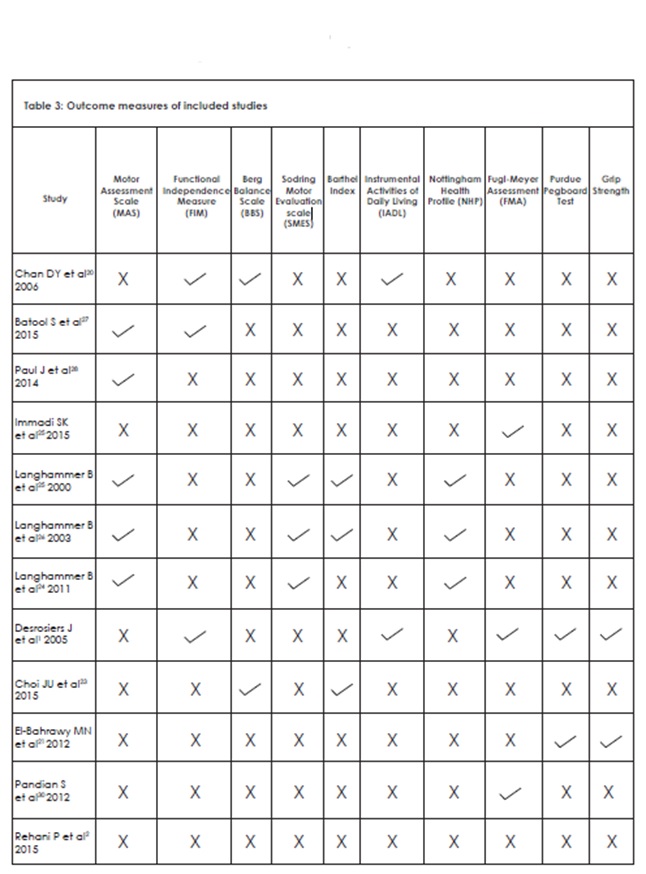
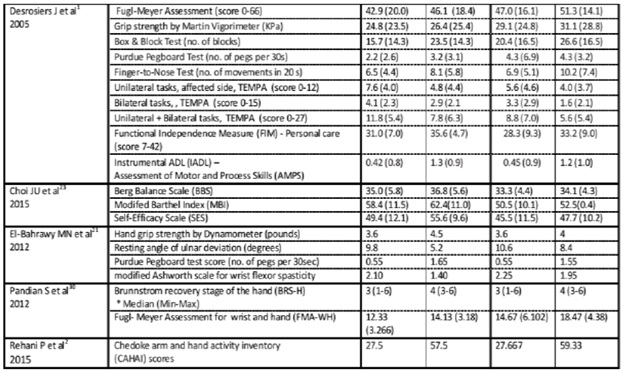
Study characteristics include participants’ characteristics, interventions and outcome measures, shown in Table 1,2,3.
- Participants’ Characteristics:
As the selected 12 studies were done on stroke patients, the most of the included studies had mentioned in inclusion criteria that patients who had first stroke were the part of the study 2,20,21,24-27,29. Post stroke duration was also mentioned in inclusion criteria of 6 studies, but it varies among them. One study mentioned maximum post stroke duration (12 months20), two mentioned minimum post stroke duration (6 months 21,23), whereas, three studies set the range for inclusion (10 days to 2 months1, 1 month to 6 months2, 6 weeks to 6 months28). Among all these studies, 8 studies showed stages or scores of different scales in inclusion criteria. 7 studies had mentioned range of age in inclusion criteria. The overall ranges of these studies for selection criteria were vary between 21 to 70 years. Brief inclusion criteria of the studies were shown in Table 1. The mean age of the patients that were participated in the individual study ranges from 47.4 to 74.3 years. Total 378 patients were participated in 10 studies. Among them, 191 had received MRP or any task relation MRP, whereas, 187 had received any other treatment technique for stroke rehabilitation. Out of 12 studies, 3 studies were done by Birgitta Langhammer and Johan K Stanghelle24-26 on same stroke patients. That’s why these patients were counted once in total number of patients. The gender representation among 366 patients illustrates that there were 171 females and 195 males. 12 patients of study of Rehani P et al2 are not included in this gender distribution because they stated percentages only without describing the frequencies. Table 2 shows the summary of demographical results of individual studies.
- Intervention:
In the included studies, motor relearning program was compared with other intervention techniques among stroke patients. A summary of these interventions for both groups is shown in Table 2. Frequency of treatment sessions and assessment timelines are also mentioned in Table 1. The intervention of the Experimental group of this systematic review was MRP. Studies vary in tasks or body regions that were involved in MRP. For example, studies focused on arm 1,2,21,27-29, hand30, 5 tasks23, 24 remedial and 10 functional tasks20, or drinking task21. The intervention of the control group of this systematic review varies, including any one from Bobath Technique 21,24-26, Constraint Induced Movement Therapy27 (CIMT), Thermal stimulation28, Brunnstrom hand manipulation30, Mirror therapy2, or Conventional or Usual therapy 1,20,23,29. An individual study, done by Batool S et al27, applied MRP to control group in comparing CIMT and MRP.
- Outcome Measures:
Different outcome measures were used in the selected studies, mentioned in Table 2. Table 3 summarizes the outcome measures that are common in them.
Figure 1: Study Selection Process
Results of Individual Studies
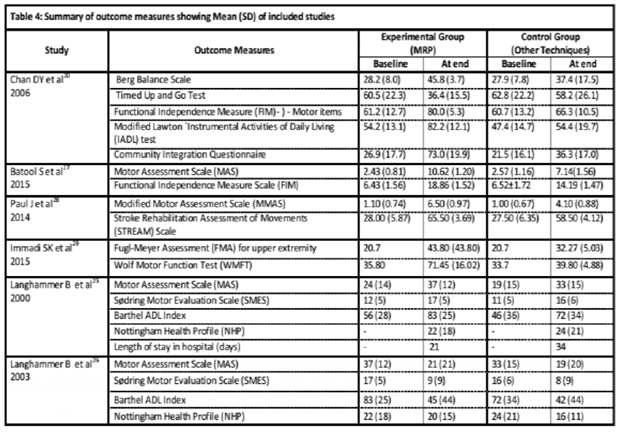
Table 4 summarizes the results of included studies for different outcome measures.
Chan DY et al 20, Paul J et al 28 , Choi JU et al 23 and Immadi SK et al29 found MRP better than other treatments. Desrosiers J et al1 reported the similar results in both groups. Whereas, Rehani P et al2 found statistically insignificant results, but found improvement in patients of both groups. Pandian S. et al30 showed that Brunstorm technique was better than MRP. Batool S. et al27 found CIMT statistically significant than MRP.
Most of the results were reported as Mean (SD). Study by Immadi SK et al29 shown their before-treatment results in form of Mean only. Whereas, SD were mentioned in after-treatment results.
The longitudinal study conducted by Langhammer B and Stanghelle JK was based on two treatment methods, MRP and Bobath. The study published in 200025 focused on acute stroke patients. The outcome measures of the patients were assessed three times that were, 3 days after admission to hospital (results shown as ‘Baseline’ in Table 4), 2 weeks thereafter, and then 3 months after it (results shown as ‘At end’ in Table 4). They found MRP better than Bobath in this study. Their research published in 200326 was the continuation of the same study. The outcome measures of the patients were reported at 3 months (results shown as ‘Baseline’ in Table 4), 1 year, 4 year (results shown as ‘At end’ in Table 4). They found decline in both groups when compared their results. They also observed the mortality rate in long-term follow-up. The number (no.) of patients in the study were 33 (MRP group) and 28 (Bobath group) in the starting. The number of patients existed at three months, were 29 (MRP group) and 24 (Bobath group) because of the death of 4 patients in each group. At 1 year, 6 and 7 patients died from MRP and Bobath groups, respectively. At 4 years, further 12 patients had been died from each group. As it was a long-term study, therefore they compared scores of 4 years from baseline. Therefore, they stated that there were no significant differences between the groups in any of the tests, and the scores at 4 years were similar to their first scores. In their study published in 201124, there was detail about Mean ± SD of items of MAS and SMES that were assessed at three follow-up occasions (at admission, after 3 weeks and after 3 months). Thus, they found MRP better than Bobath technique, as in study of 200025. Statistical analyses of items of Nottingham Health Profile were also included in that study. Due to result of individual items, this result is not shown in Table 4.
El-Bahrawy MN et al21 conducted a research on motor relearning (MR) in comparison with Bobath (BT) for improving hand function in chronic stroke patients. They showed mean of outcome measures through figures (graphs) instead of tables. Therefore, the mean values showed in Table 3 were estimated from those figures. They stated that there were significant differences in mean values of hand grip strength, Purdue pegboard test and the resting angle of ulnar deviation before and after treatment of MR and BT. Whereas, in modified Ashworth scale, there was no significant difference with BT, and significant difference with MR. When comparing after treatment means of both groups, there was significant result (P=0.0001) of MR group in improving hand grip strength and the resting angle of ulnar deviation. Moreover, results with Purdue pegboard test and modified Ashworth scale were not significant (P>0.05).
They concluded that MR method was better than BT for improving hand functions of stroke patients.
Synthesis of Results
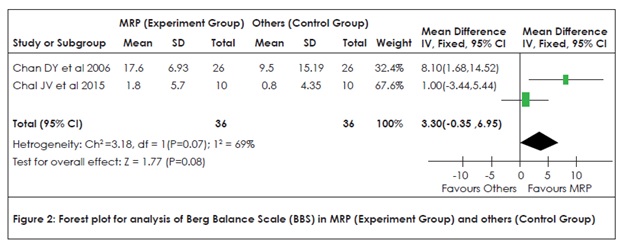
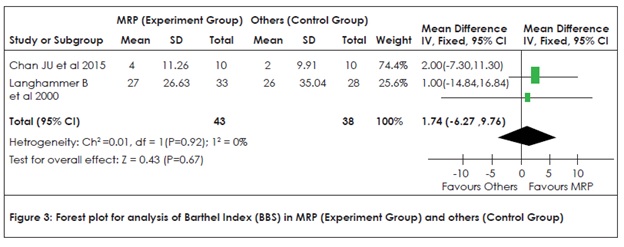
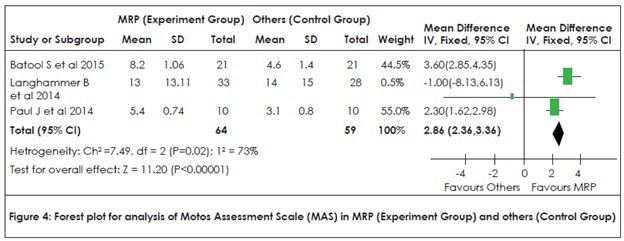
Statistical analysis of outcomes of interventions was done by assessing Heterogeneity among the studies and shown by Forest plots (Figure 2, 3 and 4).
Analysis of Berg Balance Scale (BBS) in MRP (Experimental Group) and Others (Control Group) was shown by Forest plot in Figure 2. Both studies20,23 favor MRP. Study by Choi JU et al23 weighted more in its favor than study by Chan DY et al20. Furthermore, p-value (0.008) shows that the result is slightly insignificant.
Analysis of Barthel Index in MRP (Experimental Group) and Others (Control Group) was shown by Forest plot in Figure 3. Both studies23,25 favor MRP. Study by Choi JU et al23 weighted more in its favor than study by Langhammer B et al25. Furthermore, p-value (0.67) shows that the result is not significant.
Analysis of Motor Assessment Scale (MAS) in MRP (Experimental Group) and Others (Control Group) was shown by Forest plot in Figure 4. Studies of Batool S. et al27 and Paul J et al28 favor control group. Whereas, study of Langhammer B. et al25 favors experimental group with wider CI and very small size of box. But their items for scores are not similar.
DISCUSSION
The selected 12 studies were done on stroke patients. Hence, most of them included first stroke patients. Other 4 studies did not mention this in selection criteria, but their text reflects that they had also included first stroke patients.
El-Bahrawy. et al21 showed mean of outcome measures through figures (graphs) instead of tables. The mean values showed in Table 3 were estimated from those figures after keen focusing on level of bars and may vary from exact values of the study. Outcome measures that were used in two or more studies should be compared statistically. But actually, we couldn’t able to do. There was a difference in outcome measures and their scores, as shown in table 3 and 4. Due to this, there was a problem in selecting the data for statistical analysis and forest plot. When we found an assessment scale in more than one study, the scale was either used in a modified form or its selected items were applied. For example, Functional Independence Measure (FIM) scale is used by three studies. Desrosiers J. et al1 used FIM scores for self-care assessment. Self-care comprises 6 items and score of 6 items can range from 6-42. Chan DY. et al20 used 13 motor items, whereas Batool S. et al27 used 5 items of self-care. FIM36 is 7-point scale consisting 18 items and score ranges from 18 to 126. All three studies used selected items of FIM instead of using all items and even did not use the same items. Therefore, their results cannot be compared statistically.
Berg Balance Scale (BBS)23 is a 5-point scale and contains 14 items (score 0-56). Score less than 5 shows the risk of fall, which is a major problem in stroke patients. See figure 2 for the analysis of BBS. Both studies 20,23 favor MRP. Study by Choi JU et al23 weighted more in its favor than study by Chan DY et al20 with bigger size of box. The diamond for overall result crosses the ‘line of no effect’ a little and p-value (0.008) is slightly higher than >0.05, therefore it is slightly not significant.
Barthel Index is used for ADL assessment. As we assessed we found that both Choi JU et al23 and Langhammer B. et al24 used same Barthel Index of score 0-100. Moreover, Choi JU. et al23 stated that he used Modifed Barthel Index (MBI) of Shah version. See figure 3 for the analysis of Barthel Index. Both studies23,25 favor MRP. Study by Langhammer B et al25 weighted less in its favor with comparatively wider CI and small size of box than study by Choi JU et a. The diamond for overall result crosses the ‘line of no effect’ and it shows that calculated difference between groups is not significant. P-value (0.67) also shows that the result is not significant.
Modified forms of scales can be used in RCTs to analyze the outcomes. But they are not helpful when you want to compare them statistically for review studies. The mean values of Motor Assessment Scale (MAS) of study of Batool S. et al27 and Paul J et al28 lies between 1-11. Batool S. et al27 stated that they used 3 items whereas Paul J et al28 stated it as modified. Langhammer B et al 25,26 used all 8 item and their mean scores lie in 19-37. Their study published in 201124 also showed scores for individual items. We plotted one forest plot to see how it shows when these types of scales are compared. See figure 4 for the analysis of MAS. It shows that studies of Batool S. et al27 and Paul J et al28 favors control group. Whereas, study of Langhammer B et al25 favors experimental group with wider CI, very small size of box and values shows that it has less influence on overall result. Furthermore, this study25 applied all items of scale, irrespective of both other studies 27,28.
Another scale, Fugl-Meyer Assessment (FMA) was used by three studies, Immadi SK et al29, Desrosiers J et al1, Pandian S. et al30. Immadi SK. et al29, Desrosiers J et al1, used FMA for Upper extremity motor assessment (score 0-66). Whereas, Pandian S. et al30 used FMA for only wrist and hand (score 0-30). But we cannot compare statistically the results of both studies 1,29 because Immadi SK et al29 did not show SD for before treatment means.
Upper extremities are mostly affected after stroke, leading to motor deficits and decreased ability to perform activities of daily living. Motor recovery of upper extremity is crucial for patients to become independent in performing their self-hygiene and grooming activities. In the selected studies, we found that most of the studies focused on upper extremity 1,2,27-29 or task involving upper extremity21 or only hand30.
RCTs used different outcome measurement tools, their items or scores. Multiple accessible RCTs with results of individual items of scales are negligible. More RCTs focusing on individual item of scales are needed to better assess the effects of MRP in comparison with other treatments by review studies.
More review studies focusing on individual item of scales are recommended. Unfortunately, multiple accessible RCTs with results of individual items of scales are negligible. For this reason, further RCT studies should be conducted to assess the effects of MRP in comparison with other treatments. These RCTs should draw their results from individual items of measurement scales. A better review can be conducted after comparing statistically the results and scores of same items of the multiple studies, and hence, a clearer picture can be drawn about MRP in comparison with other treatments.
CONCLUSION
Effect of MRP on Quality of Life is not significant from selected studies, after assessing Berg Balance Scale (BBS) or Barthel Index, and further researches are suggested.
REFERENCES
- Desrosiers J, Bourbonnais D, Corriveau H, Gosselin S, Bravo G. Effectiveness of unilateral and symmetrical bilateral task training for arm during the subacute phase after stroke: a randomized controlled trial. Clin Rehabil. 2005;19(6):581-593
- Rehani P, Kumari R, Divya Midha. Effectiveness of motor relearning programme and mirror therapy on hand functions in patients with stroke-a randomized clinical trial. IJTRR. 2015;4(3):20-24
- Alan SG, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Blaha MJ, et al. Heart Disease and Stroke Statistics—2014 Update. A Report from the American Heart Association. Circulation. 2014;129(3):e28–e292
- Mendis, Shanthi, Pekka Puska, and Bo Norrving. Global Atlas On Cardiovascular Disease Prevention and Control. Geneva: World Health Organization in collaboration with the World Heart Federation and the World Stroke Organization, 201
- Majid A, Reeves MJ, Birbeck GL. The epidemiology of stroke in Pakistan: past, present, and future. Int J Stroke. 2009;4(5):381-38
- The World Bank [Internet]. Data Pakistan [cited 2015 Mar 16]. Available from: http://data. worldbank.org/country/pakistan Khealani BA, Hameed B, Mapari UU. Stroke in Pakistan. J Pak Med Assoc. 2008;58(7):400-40
- Khealani BA, Wasay M. The burden of stroke in Pakistan. Int J Stroke. 2008;3(4):293-296
- Pakistan stroke society. [Internet]. [cited 2015 Mar 16]. Available from: pakstroke.com
- Syed NA, Khealani BA, Ali S, Hasan A, Akhtar N, Brohi H et al. Ischemic stroke subtypes in Pakistan: the Aga Khan University Stroke Data Bank. J Pak Med Assoc. 2003;53(12): 584-588
- Feigin VL, Barker-Collo S, McNaughton H, Brown P, Kerse N.Long-term neuropsychological and functional outcomes in stroke survivors: current evidence and perspectives for new research. Int J Stroke. 2008;3(1):33-40
- Opara JA, Jaracz K. Quality of life of post–stroke patients and their caregivers. J Med Life. 2010; 3(3):216–220
- Pollock A, Baer G, Campbell P, Choo PL, Forster A, Morris J, et al. Physical rehabilitation approaches for the recovery of function and mobility following stroke. Cochrane Database Syst Rev. 2014;22;(4):CD00192
- Wade DT, Collen FM, Robb GF, Warlow CP. Physiotherapy intervention late after stroke and mobility. BMJ. 1992;304(6827):609-613
- Baumann M, Lurbe K, Leandro ME, Chau N. Life satisfaction of two-year post-stroke survivors: effects of socio-economic factors, motor impairment, Newcastle stroke-specific quality of life measure and World Health Organization quality of life: brief of informal caregivers in Luxembourg and a rural area in Portugal. Cere- brovasc Dis. 2012;33(3):219-230
- Langhammer B, Lindmark B, Stanghelle JK. Stroke patients and long-term training: is it worthwhile? A randomized comparison of two different training strategies after rehabilitation. Clin Rehabil. 2007;21(6):495-510
- Bhalerao G, Kulkarni V, Doshi C, Rairikar S, Shyam A, Sancheti P. Comparison of motor relearning program versus bobath approach at every two weeks interval for Improving activities of daily living and ambulation in acute stroke rehabilitation. Int. J Basic Appl. Med. Sc. 2013;3(3):70-77
- Ernst E. A review of stroke rehabilitation and physiotherapy. Stroke. 1990 Jul; 21(7):1081-1085
- Seneviratne CC. A Comparison of Two Rehabilitation Therapies in the Elderly Stroke Population. Indian Journal of Gerontology. 2013;27(1):162–177
- Chan DY, Chan CC, Au DK. Motor relearning programme for stroke patients: a randomized
- controlled trial. Clin Rehabil. 2006;20(3):191-200
- El-Bahrawy MN, El-Wishy AAB. Efficacy of motor relearning approach on hand function in chronic stroke patients. A controlled randomized study. It J Physiotherapy 2012;2(4):121-27
- Ahmed AB. Dynamics of functional connectivity within cortical motor network during motor learning in stroke – correlations with “True” motor recovery. [PhD Thesis] University of Kansas: ProQuest LLC; 2013
- Choi JU, Kang SH. The effects of patient-centered task-oriented training on balance activities of daily living and self-efficacy following stroke. J Phys Ther Sci. 2015; 27(9):2985-2988
- Langhammer B, Stanghelle JK. Can physiotherapy after stroke based on the Bobath concept result in improved quality of movement compared to the motor relearning programme. Physiother Res Int. 2011;16(2):69-80
- Langhammer B, Stanghelle JK. Bobath or motor relearning programme? A comparison of two different approaches of physiotherapy in stroke rehabilitation: a randomized controlled study. Clin Rehabil. 2000;14(4):361-369
- Langhammer B, Stanghelle JK. Bobath or motor relearning programme? A follow-up one and four years post stroke. Clin Rehabil. 2003;17(7):731-734
- Batool S, Soomro N, Amjad F, Fauz R. To compare the effectiveness of constraint induced movement therapy versus motor relearning programme to improve motor function of hemiplegic upper extremity after stroke. Pak J Med Sci. 2015;31(5):1167-1171
- Paul J. Comparative study on the effect of task oriented motor relearning program and thermal stimulation over upper limb motor function among stroke subjects. Int J Physiother. 2014;1(4): 227-232
- Immadi SK, Achyutha KK, Reddy A, Tatakuntla KP. Effectiveness of the motor relearning approach in promoting physical function of the upper limb after a stroke. Int J Physiother. 2015;2(1):386-390
- Pandian S, Arya KN, Davidson EW.Comparison of Brunnstrom movement therapy and Motor Relearning Program in rehabilitation of post-stroke hemiparetic hand: a randomized trial. J Bodyw Mov Ther. 2012;16(3):330-337
- Chung BPH. Effect of different combinations of physiotherapy treatment approaches on functional outcomes in stroke patients: A retrospective analysis. HKPJ. 2014; 32:21-27
- Helm EE. Mechanisms of motor learning and brain plasticity post stroke. [PhD Thesis] University of Delaware: ProQuest LLC; 2015
- Yin Y, Gu Z, Pan L, Gan L, Qin D, Yang B, Guo J, Hu X et al. How does the motor relearning program improve neurological function of brain ischemia monkeys? Neural Regen Res. 2013;8(16):1445–1454
- Higgins J, Green S. Cochrane handbook for systematic reviews of intervention: Cochrane book series. Chichester: John Wiley and Sons, Ltd; 2008
- Follmann D, Elliott P, Suh I, Cutler J. Variance imputation for overviews of clinical trials with continuous response. J Clin Epidemiol. 1992;45(7):769-73
- Keith RA, Granger CV, Hamilton BB, Sherwin FS. The functional independence measure: a new tool for rehabilitation. Adv Clin Rehabil. 1987;1:6-18