ABSTRACT
OBJECTIVE
Post stroke foot is inability to lift foot at ankle joint due to paralysis of ankle dorsiflexor muscles. It is a common problem faced by stroke survivors. To determine the effect of ankle joint taping combined with functional electrical stimulation on post stroke foot drop.
METHODS
It was an experimental study. 10 stroke patients with foot drop were enlisted for the study by convenience sampling and randomized into two groups. The group A or treatment group (n-5) received kinesiotaping of ankle joint and functional electrical stimulation while group B or control group (n-5) received functional electrical stimulation only. Clinical assessment was done before and after study. Outcome measures were Manual Muscle Testing, active ankle dorsiflexion and time up and go test.
RESULTS
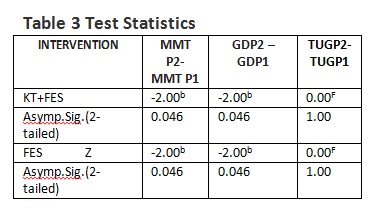
Improvement was recorded in both kinesiotaping of ankle joint with functional electrical stimulation and functional electrical stimulation groups for MMT and active range of ankle dorsiflexion and there was no significant improvement in time up and go test. But statistically non-significant difference between both groups is observed (Z=-2.000, p=0.46).
CONCLUSIONS
These results indicate that there is no clear benefit of ankle joint taping combined with functional electrical stimulation for correction of post stroke foot drop.
Keywords
Foot Drop, Functional Electrical Stimulation, Ankle Joint Taping, Kinesiotaping, Dorsiflexion, Manual Muscle Testing.
Amna Aamir Khan
Assistant Professor
Ziauddin College of Physical Therapy
Ziauddin University
Hassan Abbas
Principal
Liaquat National School of Physical Therapy
Liaquat National Hospital
Rabbia Naseer Ahmed
DPT Student
Ziauddin College of Physical Therapy
Ziauddin University
Maria Sanam
DPT Student
Ziauddin College of Physical Therapy
Ziauddin University
[Khan AA, Abbas H, Naseer R, Sanam M. Therapeutic Effects of Ankle Joint Taping combined with Functional Electrical Stimulation for the Correction of Post Stroke Foot Drop. Pak. j. rehabil.2015;4(2):15-20]
Whenever there is lack of blood supply to the brain it results in loss of neuronal functions, it is called stroke. There are two major forms of stroke named as hemorrhagic stroke and ischemic stroke. Hemorrhagic stroke occurs whenever the vessels which are supplying blood to brain gets ruptured and blood present in these vessels flows out causing compression on neural structures1. The other most common type of stroke is ischemic stroke which takes place as a consequence of clot, blockage or disruption in blood flow. About 80% of individuals suffer from this type of stroke. This type of stroke has severe impact on the life of survivor. Three out of four patients face difficulty in executing activities of daily living (ADLs)2.
Such a stroke usually leads to impaired balance and incomplete control. It is linked with high incidents of falls which leads to reduced interest in independent walking and further reduces overall activities of the sufferer. One of the consequences of stroke is the paralysis which is the inability of a muscle or group of muscles to move on their own. After suffering a stroke, signals from the brain to different muscles fail to work properly. As a result of this harm one side of body become paralyzed and as time passes it become spastic. Spasticity is a failure of muscle to stretch. Indeed, it does have an impact on the patient’s fingers, arms and/or legs. It further leads to a stiff knee, a tight fist or an arm being pushed against the chest or a pointed foot or foot drop that interferes with walking. Concurrently, it may cause occurrence of painful muscle spasm. In clinical terms, the basic principle of rehabilitation of hemiplegic patients faced with stroke is the revival of individual’s balance and gait capacity3. The stroke patients also face a general problem in ankle dorsiflexion, which leads to foot drop, since dorsiflexion is not easily controllable because it frequently enhances the muscle tone of triceps surai4.Spastic foot drop is a functional disfigurement which usually leads to extensive morbidity by impairment in patient’s walk. It limits ones day to day activities due to ankle dorsiflexion during the gait cycle because it is dangerous for foot clearance; patient may fall down due to foot drop and face severe injury. Another cause for existence of spastic foot drop is the combination of weak ankle dorsiflexors and hyper activity of planter flexors (primarily gastrocnemius and soleus) 5,6. Apart from the problems with patient’s walking restrictions, critical patients with severe problem due to spastic foot drop may limit their movement even in the presence of supporters due to unstable contact on the ground. Moreover, when ankle posture becomes uneven it may cause severe aching points within the shoe (or against the mattress) which can further lead to breakdown of the patient’s skin7. The most important consideration of the rehabilitation is improving the way a patient’s walks. Even after the recovery of patient’s ambulatory function to a few degrees, the remaining gait defects also lead to sluggish walk movements, leading to high energy costs8.
According to the results of conventional assessment about 20% stroke patients experience spastic foot drop9. The topic that deals with the impact of ankle stabilizers on proprioception is quite controversial. A number of researchers have strong faith in taping and stimulating proprioceptive activity due to enhanced motivation of cutaneous mechanoreceptors10. Jerosch et al reported that when proprioception was analyzed utilizing angle reproduction tests, mistakes in proprioception diminished in a bunch of patients with ankle harm to which taping was connected11. While some others have unfavorable activity due to tape and support 12,13. According to a study of Raymond et al who conducted meta-analysis, the ankle brace or ankle tape have no significant impact on proprioceptive activity in participants having functional ankle instability14.
Despite of the fact Kinesiotape is being extensively used for the purpose of rehabilitation protocols and also to prevent sports injuries in the healthcare field i.e. by physical therapists and athletic trainers. Evidence for the efficacy of Kinesiotape is yet limited15. According to SzczeGielniak J, et al who have assessed the effect of corrective foot positioning using KT application on gait velocity in patients after stroke by making using of a 100 meter walk test; the benefit of KT‘s corrective application in supporting neurological physiotherapy in patients after cerebrovascular stroke is quite significant. The use of KT is different for different conditions according to nature of tape or the muscle16. According to the Callaghan et al. that taping fundamentally enhanced the proprioception in those with generally poor proprioception in spite of the fact that it had little impact on those with abnormal proprioception17. Taping is known to enhance proprioception and by coming into contact with the skin, give increased skin proprioceptor signals18. Many interventions are used in the physical therapy hospitals for the treatment of foot drop. The most widely recognized treatment for foot drop has been the utilization of a lower leg foot orthosis (AFO). An AFO is an orthosis put on the paralyzed leg which latently holds the foot at around 90o from the shaft of the tibia which allows the foot to clear ground during the swing phase of the gait cycle. Studies examining the use of an AFO for the treatment of foot drop have reported reduced energy consumption during ambulation, enhanced postural sway, expanded standing symmetry, and an enhanced gait patter, particularly changes in step length and walking speed19. The disadvantage of using an AFO cause limitation in foot movement, contractures of planter flexors inability to ambulate over uneven surfaces, and the distress of wearing the orthosis20.
Functional Electrical Stimulation (FES) is another intervention for the treatment of foot drop post-stroke. FES utilizes electrical incitement to enhance the lower leg dorsiflexior muscles and produce a muscle contraction during the swing period of gait. A typical FES unit found in the writing is the Walk Aide. The most common placement of the active electrode is over the common peroneal nerve, simply distal and dorsal to the head of the fibula allowing a combination of ankle movements, specifically ankle dorsiflexion and eversion21. Disadvantages to an electrical stimulator unit incorporate the high cost, which may not be secured under protection, vague position of terminals, discontinuous substitution of electrodes, and necessity of a starting set-up and re-adjustment all through the utilization of the unit19. Stroke patients generally experience a problem in ankle dorsiflexion due to paralysis of ankle dorsiflexors which result in foot drop. Improvement of walking pattern in the stroke patients is the most important factor. For the treatment of foot drop many physical therapy interventions are used. This study may help in understanding the role of ankle joint taping combined FES for the foot drop correction.
METHODOLOGY
Research Design and Sample Size The present study is an experimental study. The participants of this study were ten stroke patients (n-10) including males and females with foot drop were included by their convenience from different hospitals in Karachi. The subjects were divided into two groups A and B for the purpose. Inclusion Criteria
- Patients with post stroke foot drop more than 90 days.
- Age 40-80 years.
- Unilateral hemiplegia.
- Medically stable.
- Ankle dorsiflexiors of no more than 3/5 on Manual Muscle Testing.
- If patient is using an AFO willing to remove it and comply with study needs.
Exclusion Criteria
- Requires KAFO to maintain knee in stable extended position during stance phase of gait.
- Pedal edema of affected lower extremity which interferes with the effective use of kinesiotape and FES.
- Known skin allergies and breakdown of skin of affected limb.
- Absent sensation.
- Severely impaired cognition and communication skills.
- Fixed planter flexor contractures
Procedure
The study period consisted of 3 months from August-September and general characteristics of subjects were surveyed before applying kinesiotape and functional electrical stimulation. Kinesiotape was applied to the foot using spring-assist technique also known as functional correction for ankle joint taping. This technique works while providing sensoriomotor and mechanical stimuli to promote dorsiflexion. Affected foot was shaved before applying kinesiotape to increase contact area. Firstly, the affected foot was positioned in full dorsiflexion passively then tape was applied from mid shaft of tibia to heads of metatarsals with 50-70% tension then foot was positioned in full planter flexion passively and tape was rubbed to activate the adhesive power of tape. Because of this technique when the ankle moves in more planter flexion it will increase tension in tape and provide more stimulus to dorsiflexiors. Ankle joint taping was done for four weeks and tape was changed after 5 days of application.
Four electrodes of FES unit were applied on the motor points of dorsiflexors of affected foot using 300pps, ramp up time 3 seconds and ramp off time 6 seconds. After application of FES, participants were asked to walk 20 meters with their normal speed 5 days a week for four weeks. They were allowed to use assistive device during walk.
Outcome Measures
The outcome measures included Manual Muscle testing primarily, Goniometry of ankle dorsiflexion and Time Up and Go test secondarily.
Data Analysis
Data was entered and analyzed on SPSS version 20 for windows. All quantitative variables such as age were presented in frequency and percentage. To check the significance of the treatment, Wilcoxon ranked sum test was applied with p value less than 0.05 considered as significant.
Ethical Consideration
As a part of this study protocols, written consent was taken from all the participants after reading participants information sheets. They were allowed to withdraw at any time. Confidentiality of participant’s personal information was maintained. Physical risks, psychological harms were minimized and patient privacy hygienic factors were given due importance.
RESULT
All participants completed the study. At the fourth week, results were extracted from the data collected from 10 patients (5 in kinesiotaping combined with FES group and 5 in FES group). No serious side effect was seen in any of the patient during the study.
There were 5 males and 5 females in our study. And 5 participants had left sided paralysis while 5 had paralysis of right side.
The level of function of participants of study was; two out of 1o patients were independent and they exercise regularly while 8 out of 10 were independent before stroke but they do not perform regular exercise.
Table 1 shows walking patterns of patients. Most of patients drag there foot during walk, few patients adopted compensatory gait pattern that is; 2 patients hike hip during walk and 3 patients walk with hip circumduction to clear ground. Half of the participants present with unstable foot contact.
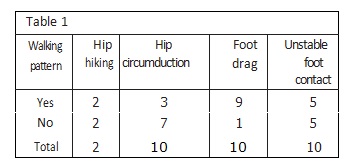
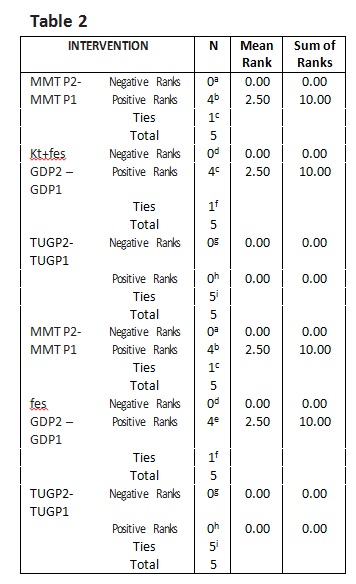
Table 2 shows data of pre and posts treatment scores of MMT, range of active dorsiflexion, and TUG test of both case and control group.
A Wilcoxon Rank sum test shows that 4 week of treatment with ankle joint taping combined with FES and FES only elicit a statistically non-significant difference in correction of foot drop in individuals. (Z.-2.000, p=0.46) both group shows similar results as shown in the table 3.
DISCUSSION
The survivor of stroke who are managed with rehabilitation have fewer complications and they achieve a greater level of independence as compared
to those who do not follow any rehabilitation program, if the natural recovery process do not occur rehabilitation is expensive but only appropriate therapy program can be justified. Only variety of rehabilitation techniques and protocols prove good quality of the rehabilitation in terms of expenditure and psychological advantages.
This study assessed the therapeutic effects of ankle joint taping combined with FES on muscle strength, ankle dorsiflexion and TUG test and compared it with the control group who receive FES only in patients with post stroke foot drop. No significant difference in results was found between both groups. Different methods are used to increase the strength of ankle dorsiflexors and to improve active range of ankle dorsiflexion including PNF techniques, strengthening exercises, electrical stimulation or implantable FES. Although combined FES with rehabilitative treatment is accepted, but it cannot be said which treatment is more effective. Effectiveness of tapping has been mentioned in some studies, frequency of tape application and technique. So further studies are needed in future just as kinesiotaping group without FES to identify clear role of ankle joint taping with kinesiotape.
The person suffering from this stroke have gait problems which is one of the leading impairments. It is recommended in our review that the FES therapy can be used with kinesiotapping in the post-stroke rehabilitation process of patient with foot drop. The results of the study suggest, the combination of FES and the spring-assist kinesiotape contain a positive therapeutic effect on the activation, recovery of strength, functional mobility and gait but there was minimal increase in the amount of ankle dorsiflexors strength, being only a half grade increase. Even though a gain in strength is minimal but depicts a sign of a positive prognostic which results in gaining functional strength. No significant result was obtained within the required period of TUG test. To be comparative to initial trials the times taken by the subject to complete the test were same or increase in many of the subjects. Therefore in this study, no specific measures concerning gait parameters were performed. At the end of the study, request was made to the patients with the kinesiotape complaint to continue the treatment. The patient or subject did not complain of discomfort or any type of diverse skin reaction at taping side. FES is an acceptable treatment of foot drop despite of its many drawbacks. High coast, placement and replacement of electrodes and requirement of initial setup of FES unit are included in the treatment through FES. The patient or subject did not complain of discomfort or any type of adverse skin reaction at taping site. FES is an acceptable treatment of foot drop despite of its many drawbacks.
High coast, placement and replacement of electrodes and requirement of initial setup of FES unit are included in the treatment through FES. Those subjects who were trialed with both FES and kinesiotape are said to have an improved ability for the movement of their ankle with comfort and can walk comfortably in a normal way. Patient also reported that decreased energy expenditure was required during ambulation.
Although TUG score showed no improvement on the basis of normative data still high risk of falling is present in the patient as a number of movement activities like sitting standing and moving ahead and turning around 180 degrees is involved.
Research investigation to increase muscle strength, function and mobility by kinesiotape and FES therapy seems to be quit less and inconsistent as there are no articles in the literature on combined therapy concerning lower extremity. A single reported case found in the literature documenting the use of kinesiotape for the intervention of shoulder subluxation in a post stroke patient. The report says that kinesiotape may contribute to decrease pain better than glenohemural joint alignment and enhanced neuromuscular recruitment of the rotator cuff muscles22.
Marmara University School of medicine, Istanbul examined the combine effect of kinesiotaping with botulinum toxin to improve spasticity of ankle planter flexors and find no significant decrease in spasticity.
Studies that examine the therapeutic application of kinesiotape to a population with prior muscle weakness report positive results. This trend shows that kinesiotape give more subtle muscular effect which centers more on increasing neuromuscular recruitment rather than increasing healthy muscle strength.
Cheng J.S et al. studied the therapeutic effect of combined electrical stimulation with active ankle dorsiflexion while standing on rocker board with spastic foot drop and their results suggest that ankle
spasticity can decrease with repeated electrical stimulation plus ankle movement in stroke. Whereas another study compared the conventional therapy and multifunction FES and find improvement in MFES combined with conventional therapy as compared with conventional therapy alone and these better results were achieved by enhancement of motor learning by MFES.
A study was conducted in Republic of Korea on effects of lower leg kinesiotaping on balance abilities of stroke patients with foot drop in which they use kinesiotape to shaft of tibia and ankle and supportive anchors were applied for stability. They use BBS for assessment of balance ability and concluded that temporary kinesiotape application have good effect on stationary balance however, in our study we use kinesiotape for 5 days per week for four weeks and assessed the strength of dorsiflexiors 23-25.
Therefore to quantify the treatment effects and to examine the degrees in which the kinesiotape and FES facilitated improvements longer studies are required. Research should also investigate the influence of kinesiotape and FES therapy on specific gait parameters.
CONCLUSION
Application of kinesiotape and FES seems to be an effective addition to stroke rehabilitation. After periods of FES training and kinesio tape application patients show carry over effects. The results indicate that the combined treatment of kinesiotape and FES effectively improved function, muscle strength and walking ability in the management of foot drop with stroke patients, however further research is needed and encouraged, especially with FES systems.
REFERENCES
[1] O’Sullivan S, Schmitz TJ, Fulk GD. Physical Rehabilitation. 6th ed. United States of America. F. A. Davis Company; 2014.
[2] Jorgensen HS, Nakayama H, Rancho HO, Olsen TS. Neurologic and functional recovery: the Copen-hagen stroke study. Phys Med Rehabil Clin N Am. 1999;10(4):887–906.
[3] Michelle MO, Nathan KL, Jonathan FB, Edward PJS, Walter RF, Roger AF. High-intensity resistance training improves muscle strength, self-reported function, and disability in long-term stroke survivors. Stroke. 2004;35:1404-1409.
[4] Burridge JH, Taylar PN, Hagan SA. The effects of common peroneal stimulation on the effort and speed of walking: a randomized controlled trial with chronic hemiplegic patients. Clin Rehabil. 1997;11(3):201-21.
[5] Royal Collage of Physicans, British Society of Rehabilitation Medicine, Chartered Society of Physiotherapy, Association of Chartered Physiotherapists Interested in Neurology. Spasticity in adults: management using botulinum toxin. National guidelines. London (UK): RCP; 2009.
[6] Adams J, Perry J. Gait analysis: clinical application. In: Rose J, Gamble J, editors. Human Walking. Baltimore (MB): Williams and Wilkins; 1994.
[7] Mayer N, Esquenazi A, Childers M. Common patterns of clinical motor dysfunction. In: Brashear A, Mayer N, editors. Spasticity and other forms of muscle overactivity in the upper motor neuron syndrome. Bronx (NY): We Move; 2008:27–38.
[8] Olney SJ, Monga TN, Costigan. PA: Mechanical energy of walking of stroke patients. Arch Phys Med Rehabil 1986;67:92-98.
[9] Johnson CA, Burridge JH, Strike PW, Wood DE, Swain ID. The effect of combine botulinum toxin type a and functional electrical stimulation and the treatment of spastic foot drop after stroke: a preliminary investigation. Arch Phys Med Rehabil. 2004;85(6):902-909.
[10] Feuerbach JW, Grabiner MD, Koh TJ. Effect of an ankle orthosis and ankle ligament anesthesia on ankle joint proprioception. Am J Sports Med. 1994;22(2):223-229.
[11] Jerosch J, Hoffstetter I, Bork H. The influence of orthoses on the proprioception of the ankle joint. Knee Surg Sports Traumatol Arthrosc. 1995;3(1):39–46.
[12] Refshauge KM, Kilbreath SL, Raymond J. The effect of recurrent ankle inversion sprain and taping on proprioception at the ankle. Med Sci Sports Exerc. 2000;32(1):10–15.
[13] Refshauge KM, Raymond J, Kilbreath SL. The effect of ankle taping on detection of inversion– eversion movements in participants with recurrent ankle sprain. Am J Sports Med. 2009;37(2):371–375.
[14] Raymond J, Nicholson LL, Hller CE, Refshauge KM. The effect of ankle taping or bracing on proprioception in functional ankle instability: a systematic review and meta‐analysis. J Sci Med Sport. 2012;15(5):386–392.
[15] Kaya E.,Zinnuroglu M, Tugcu I. Kineiotapping compared to physical therapy modalities for the treatment of shoulder impingment syndrome. Clin Rheumatol. 2011;30(2):201-207.
[16] Szczegielniak J, Banik D, Łuniewski J, Bogacz K, Śliwiński Z The effect of Kinesiology Taping application on the result of 100 meter walking test in patients after cerebrovascular stroke. Med Sports Press. 2012;1(4):71-75.
[17] Callaghan MJ, Selfe J, Bagley PJ, Oldham JA. The effects of patellar taping on knee joint proprioception. J Athl Train. 2002;37(1):19-24.
[18] Kim CI, Kwon OY, Lee CH. Effect of taping on ankle range of motion and proprioception. J University Trained Phys Ther. 2001;8(3):43-52.
[19] Simonsen EB, Moesby LM, Hansen LD, Comins J, Alkjaer T. Redistribution of joint moments during walking in patients with drop-foot. Clin Biomech. 2010;25(9):949-53.
[20] Bulley C, Shiels J, Wilkie K, Salisbury L. User experiences, preferences and choices relating to functional electrical stimulation and ankle foot orthosis for foot-drop after stroke. Physiotherapy. 2011;97(3):226-233.
[21] Sabut S, Lenka P, Kumar R, Mahadevappa M. Effect of functional electrical stimulation on the effort and walking speed, surface electromyography activity, and metaboli responses in stroke subjects. J Electromyo Kinesio. 2010;20:1170-1177.
[22] Stein RB, Everaert DG, Thompson AK, Chong SL, Whittaker M, Robertson J. Long-term therapeutic and orthotic effects of a foot drop stimulator on walking performance in progressive and nonprogressive neurological disorders. Neurorehabil Neural Rep. 2010;24:152-167.
[23] Jaraczewska E, Long C. Kinesio tape in stroke : improving functional use of the upper extremity in hemiplegia. Stroke Rehabil .2006;13:31-42.
[24] Bea YH, Kim HG, Kyung SM, Lee SM. Effect of lower leg kinesiology taping on balance ability in stroke patients with foot drop. Evid Based Comp Altern Med. 2014;1-5.
[25]Yoshida A, Kahanov L. The effect of kinesio taping on lower trunk range of motions. J Res Sports Med. 2007;15(2):103-112.
