ABSTRACT
Acute back pain is the fifth most common reason for visiting the physicians and practitioners. It is one of the most common musculoskeletal problems in the society. This research has been conducted on experimental method by using sample size of 60 patients including both the genders. The participants have been selected from the OPD of physical therapy and rehabilitation of the tertiary care hospital. 60 patients was divided into two groups where Group A was treated with hot packs at low back for 25 minutes with low back strengthening exercises and whereas Group B was treated with SWD (continuous mode) for 15 minutes with the exercises. Exercises were started from the 4th day of treatment in both conditions after being relieved from acute back pain and spasm. Both groups received 5 sessions per week for consecutive 3 weeks. Therefore, the symptoms have been reassessed at 8th and 15th day of treatment. After analyzing the data, it was found that, the patients in group A treated with hot packs and back strengthening exercises were relieved from pain more quickly and efficiently than the group B treated with short wave and exercises.
Keywords
Short Wave Diathermy, Exercises, Hot Pack, Acute LBP, Deep Heating, Musculoskeletal Problem, Spasm, Physical Therapy, Rehabilitation
Samreen Yasmeen
Assistant Professor
Ziauddin College of Physical Therapy
Ziauddin University
Syeda Amool Sakeena Rizvi
Lecturer
Ziauddin College of Physical Therapy
Ziauddin University
[Yasmeen S, Rizvi SAS. Effects of Short Wave Diathermy and Hot Pack with Back Strengthening Exercises in the Management of Acute Low Back Pain. Pak. j. rehabil. 2013;2(2):10-14]
INTRODUCTION
Low Back Pain (LBP) is defined as an uncomfortable sensation in the lumber and buttock region due to some injury as well as irritation of spinal neurons originating from spinal canal1. In LBP, lower spine is usually involved. The back pain can be classified as both nonspecific back pain and specific back pain depending on the factors either known or unknown2. It may be due to radiculopathy (nerve root involvement) or discogenic disease2. In a recent study, it has been revealed that the direct cost of back pain related to medical services and diagnostic test were estimated to be US $91 billion3 while the indirect cost related to occupation and household activities were estimated between US $7 billion and US $20 billion 4-6.
A number of causes such as lifting heavy objects, sudden twisting motion on back and prolong sitting in one position and using computer leads to LBP6. Upright sitting up to 90 – degree causes more strain on the back than sitting in a 135-degree position. There are several sources in low back that may cause LBP, the most often being spasms of the large, supportive muscles along with spine.
The incidence and prevalence rate of LBP is very high; the pain improves significantly but does not resolve completely during 4 – 6 weeks7. In many cases the pain persists for several months7. The LBP can be managed in primary care. In Australia, LBP is the eighth most common conditions which can be managed by GPs8. In European guidelines, it is stated that 90% of patients with LBP improves in 6 weeks9. When compared with other studies, it shows that in patients with acute LBP; recovery ranges from 39% to 76%10-11.
In controlling acute LBP, physical therapy treatment is very significant12,13, it is suggested that, remaining being active is more effective than on bed rest14,15. Evidence shows that, there are varied physical therapy treatments in controlling acute LBP12,13,16-21.
Therefore, we considered two different modes of heat therapies, which help in relieving LBP such as Short-Wave Diathermy (SWD) and hot packs. Heat therapy helps in relieving LBP by several mechanisms. Heat therapy dilates the blood vessels of the muscles around the lumbar spine, thus, it increases the oxygen supply and also nutrients of that region so as to increase healing of the injured tissues. The receptors beneath the skin are also stimulated by heat which decreases the transmission of pain signal to the brain and helps in decreasing the perception of pain. Heat facilitates stretching in the muscles, connective tissues, and adhesions. With the heat therapy, flexibility and comfort level will be increased immensely, hence, decreasing stiffness and injuries. Therefore, to maintain healthy back, flexibility is found to be essential22.
Heat has been used for many years to treat injured muscle tissue. In clinical settings, two types of heating modalities are being used: superficial heating modality, such as; hot packs, paraffin baths, and whirlpools and deep heating modality, such as; diathermy and ultrasound. Superficial heating modality provides heat to the skin and subcutaneous tissues up to 1 cm below the skin surface while the deep heating modality provides heat to the deep tissues up to 3-5 cm without over heating the skin and subcutaneous tissues. The transfer of heating mechanism defined in literature, are of 3 types of heat transfer: conduction, convection, and conversion23,24.
Conductive heat is the transfer of heat through the direct contact between hotter and cooler areas (two objects touching each other). Hot pack, ice massage and electric heating packs are commonly utilized23. Conductive heat is usually a considered as superficial heat whereas convectional heat is the transfer of heat by the movement of a medium (air, liquid) between regions of unequal temperature. Whirlpool is one of the most common examples. Conversion heat is when the energy is changed from one form to another such as ultrasound, and diathermy 23,24.
SWD has been a viable modality in physical therapy. The concept of producing deep heat within the tissue, beyond the reach of hot packs and other form of superficial heat is appreciated by clinicians. Superficial heat is also an effective form of treatment for a number of problems, such as, musculoskeletal strain/ ligamentous sprain, pain and spasticity.
The SWD is a deep heating modality and applied sufficiently to provide heat to the deep tissues. It has been used for therapeutic purpose since 1928. The commercial unit used for this purpose has frequency of 27, 12 MHZ and the wave length of 11.06m25. Two different modes are commonly used where continuous also termed as constant mode has been used to provide heat to the deep tissues while the pulse mode provide intermittent heating and have less heating effects. It also enhances the non-thermal effects of radio frequency energy26,27. SWD with continuous mode can help in managing pain and relieve muscle spasm with resolve inflammation and also reduce swelling. It also promotes vasodilation with increase blood flow and the compliance of connective tissue, increase joint range and decrease joint stiffness.
A number of researches has been conducted on the effect of SWD in comparison with different modalities; ultrasound, microwave, infra-red and TENS but the effect of hot pack has never been compared with it in acute back pain problem. The main purpose of this study is to compare the effectiveness of superficial and deep heating with low back exercises in controlling acute LBP and also to find the cost effectiveness between these two methods of treatment because the short wave is an expensive modality and hardly available at home. This is the reason that the patients visit the physical therapy clinics for the treatment that is costly for those who are unable to afford.
METHODOLOGY
Study Design
The research has been conducted on experimental method by using sample size of 60 patients of both genders. All the subjects were randomly divided into two groups; A and B, to collect the information before fulfilling the requirements of the study with the written consent whereas, group A was treated with hot pack with back strengthening exercises as well as hot pack was used for 25 minutes once a day with 5 back strengthening exercises, 5 repetitions for each exercise twice a day.
While Group B was treated with SWD (continuous mode) with back strengthening exercises. Short wave applied at low back for 15 minutes once a day with 5 back strengthening exercise, 5 repetitions for each exercise twice a day. Pain intensity was measured through Visual Analog Scale (VAS) on 1st, 8th and 15th day of treatment. VAS rating from 0 to 10 in which 0 and 1 was taken as remarkable improvement28.
Study Duration
The study was conducted over a period of 8 months.
Inclusion Criteria
Patients suffering with localize acute LBP with spasm and mild to moderate spinal degenerative changes. Secondly, those patients that fall into the age bracket of 25 to 50 years were included in the study.
Exclusion Criteria
Patients suffering with ruptured or herniated disc with radiculopathy (sciatica) poor alignment of the vertebrae, strain or tears of the muscles or ligaments supporting the back, abnormal spine curvatures (like scoliosis), spinal stenosis, peripheral vasculopathy, acute heart problem, pregnant women, and post spinal surgery/ instrumentation were excluded from the study. Medical “Red Flags29” such as fracture, rheumatoid arthritis, osteoporosis, and tumor) prolonged steroid use and bone tissue infection or malignancy.
Data Collection Procedure
A sample size of 60 patients was taken and divided into two groups. 12 patients were unable to complete the treatment sessions due to some problems. Group A consisted of 27 patients that were treated with hot packs and back strengthening exercises while group B consisted of 21 patients that were treated with SWD (continuous mode) and back strengthening exercises twice a day. There were 15 sessions of treatment (5 sessions per week for consecutive 3 weeks) for each group. Exercises commenced from 4th day of treatment in both groups after relieving acute back spasm. Brochures were given to the patients to perform all the exercises correctly at home. Before starting the treatment, assessment was completed through physical examination and all information was recorded in the assessment form that was designed for the research. Re-assessment was done on the 8th and the 15th day of the treatment. Improvement in pain was measured through Visual Analog Scale (VAS) in both groups. Correct postural education was also given to the patients and they were provided with the correct posture chart as well, to perform daily life activities.
RESULTS
The following results were analyzed carefully from research, that is, improvement in back pain is rated through VAS. After collecting the data, it is plotted as a graph.
After completion of treatment, those patients whose pain rating on VAS, recorded between 1 and 0 was considered as remarkable improvement.
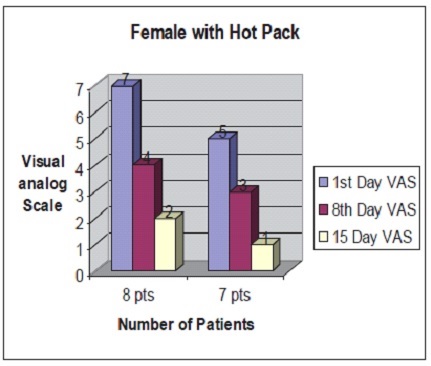
The figure 1 shows that the visual analog scale of 8 patients on first visit lies on 7; this indicates the severity of pain. After 8 sessions of treatment, the intensity of pain decreases from 7 to 4 and at 15th session, the pain remains negligible and visual analog scale declines to 2. Similarly, other 7 patients initially lied on VAS 5 then finally declined on 1 after completion of treatment.
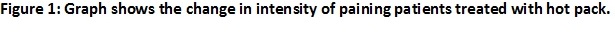
In figure 2, VAS of 8 patients initially lies on 7 whereas for other 4 patients, it lies on VAS 4. After completing 15 sessions of treatment; it falls to 2 and 0 respectively.
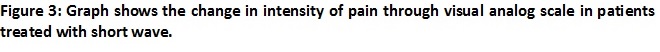
The Figure 3 shows that the intensity of pain on VAS of 6 patients lies on 8, whereas for other 7 patients it lies on 5, while after completion of 15 session of treatment through short wave, the intensity of pain drops to 3 and 2 respectively.
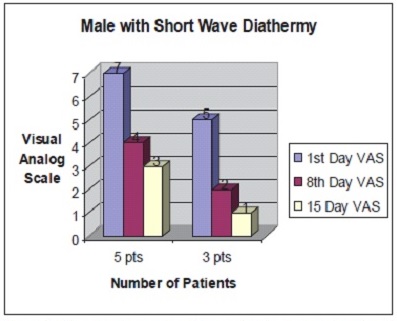
The Figure 4 shows that the VAS of 5 patients lies on 7 and for other 3 patients, it lies on 5 in first visit, while after completion of treatment, it drops to 3 and 1 respectively.
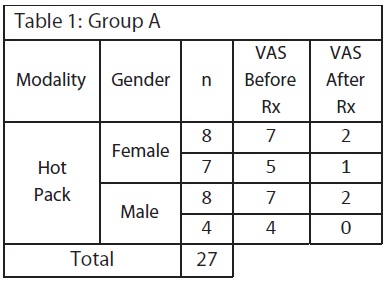
After gathering of all data, it exhibits that, group A comprises 11 out of 27 patients basing on VAS such as, 40.74% patients, fell on 1 or 0, which is remarkable improvement. The visual analog scale of remaining 16 patients such as, 59.25% patients that fell on 2; hence, showing good improvement.
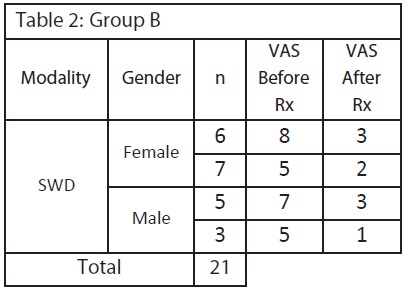
In group B, 3 out of 21 patients, that is, 14.28% patients fell on VAS 1 thus, indicating remarkable improvement. On the other hand, 7 patients, that is, 33.3% patients fell on VAS 2 that is good improvement while remaining 11 patients, that is, 52.38% patients their VAS after treatment fell on 3, that is, moderate improvement.
DISCUSSION
After completion of treatment, we found that, both the groups having the rate of improvement from acute LBP. Group A, treated with hot pack with back strengthening exercise which is greater than the patients of group B, who has been treated with shortwave diathermy (continuous mode) and back strengthening exercises.
The data also showed that in Group A, 15 out of 27 patients were females and their VAS after treatment fell on 2 and 1. Whereas in 12 males, it fell on 2 and 0 so it is depicted that, males have more tendency to control pain with hot pack which is considered to be more effective than females.
While in Group B, 13 out of 21 patients were females and their VAS after treatment dropped on 3 and 2 whereas VAS of 8 males was dropped on 3 and 1. This also indicates that the tendency of controlling acute LBP in males is more effective than females.
Therefore, it is analyzed that, hot pack is more effective than the short wave in controlling acute LBP meanwhile it is found to be more cost effective as well and is easily manageable at home.
A postal survey had been conducted on 116 senior physiotherapists in 41 Irish hospitals-based physiotherapy departments to find the efficacy of SWD with continuous mode and pulsed mode. The analysis showed that, respondents used both modes of treatment but pulsed mode of SWD was the preferred mode of treatment and 27% of respondents used PSWD more than once daily30.
Another study of cross-sectional survey had been conducted in Thailand, to collect the information on physiotherapists, LBP patients, and treatment interventions. 559 physiotherapists were included (77.2% response rate), and 502 of these were involved in LBP management. Results showed that, commonly used modalities by hospital-based physiotherapist in controlling acute LBP were hot packs 64%, ultrasound 61%, and mechanical traction 61% whereas physiotherapists in university-based hospitals and private clinics were more likely to use manual therapy31. Our results shows that the group A (N= 27) hot pack with back strengthening exercise give more effective results in the management of acute LBP as compare to the group B (N=21) which was treated with SWD and back strengthening exercise.
CONCLUSION
The acute LBP is found to be the most common problems in the society and the major cause of the acute LBP is acute spasm due to poor postural activities. The physician referred the patients to the physiotherapist for the postural correction and for the back strengthening exercises. In clinical practice, the patients with acute LBP is treated with shortwave diathermy which is deep heating modality and also with hot packs which have superficial heating effects with back strengthening exercises. The physical therapy is an expensive treatment and it is not affordable by everyone to take 15 sessions of treatment. After this research, it is concluded that, hot pack with back strengthening exercises is more effective than the SWD so, it can easily be managed at home. Physiotherapist can help in learning postural correction and exercise if visited twice a week which can otherwise be conducted at home.
RECOMMENDATIONS
This research was conducted with continuous mode of treatment of short wave and can also be done with pulse mode. Hot pack is used for superficial heating while SWD is a deep heating modality. Ice pack is also used to reduce spasm and acute pain with superficial effects, therefore in future hot pack can be compared with cold pack. This research is conducted on acute back pain and should also be carried out on chronic back pain. Along with the previous limitations similar study should be carried on large scale and the samples to be drawn from different hospitals and communities. The problem of acute LBP can also be decreased through awareness programs of postural correction and by improving the activities of daily routine.
REFERENCE
- Wedderkopp N, Leboeuf-Yde C. Preventing back pain. BMJ 2008;336(7641):398.
- Deyo RA, Weinstein JN. Low Back Pain. N Engl J Med 2001;344(5):581-85.
- Pivec R, Stokes M, Abhishek S, Paulino CB, Harwin SF, Mont MA. Clinical and Economic Impact of TENS in Patients with Chronic LBP: Analysis of a Nationwide Database. Orthopedics 2012;36(12):922-928.
- Ricci JA, Stewart WF, Chee E, Leotta C, Foley K, Hochberg MC. Back pain exacerbations and lost productive time costs in United States workers. Spine 2012;31(26):3052–3060.
- Stewart WF, Ricci JA, Chee E, Morganstein D. Lost productive time, and cost due to common pain conditions in the US workforce. JAMA 2003;290(18):2443–54.
- Dagenais S, Caro J, Haldeman S. A systematic review of low back pain cost of illness studies in the United States and internationally. Spine 2008;8(1):8–20
- Gulati S, Jakola AS, Solheim O, Gabrielsen S, Godø PA, Skogstad B, et al. Assessment of referrals to a multidisciplinary outpatient clinic for patients with back pain. J Man Manip Ther 2012;20(1):23–27.
- Australian Institute of Health and Welfare (2004) Australia’s Health 2004. AIHW,
- Canberra 4. Gellhorn AC, Chan L, Martin B, Friedly J. Management Patterns in Acute LBP: the Role of Physical Therapy. Spine 2012;37(9):775–782.
- Bekkering GE, Hendriks HJM, Koes BW, Oostendorp RAB, Ostelo RWJG, Thomassen JMC, et al. Dutch Physiotherapy Guidelines for LBP. Physiotherapy 2003;89(2):82-96.
- Wand BM, Bird C, McAuley JH, Dore CJ, MacDowell M, De Souza LH. Early intervention for the management of acute LBP: a single-blind randomized controlled trial of bio-psychosocial education, manual therapy, and exercise. Spine 2007;29:2350–56.
- Deyo RA, Diehl AK, Rosenthal M. How many days of bed rest for acute LBP? A randomized clinical trial. N Eng J Med 2008;315:1064–7016.
- Chou R, Qaseem A, Snow V, Casey D, Cross JTJ, Shekelle P, et al. Diagnosis and treatment of LBP: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med 2007;147:478–491.
- Hart LG, Deyo RA, Cherkin DC. Physician office visits for LBP: frequency, clinical evaluation and treatment patterns from a US national survey. Spine 1995;20:11–19.
- Cherkin DC, Sherman KJ, Hogeboom CJ, Erro JH, Barlow WE, Deyo RA, et al. Efficacy of Acupuncture for Chronic LBP; Protocol for Randomized Control Trial. Trials Journal 2008;9:10 doi:10.1186/1745-6215-9-10
- Farrar JT, Young JP, LaMoreaux L, Werth JL, Poole RM. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. IASP 2001;94(2):149-158.
- Hurleya DA, McDonoughb SM, Baxterb GD, Dempsterc M, Moor AP. A descriptive study of the usage of spinal manipulative therapy techniques within a randomized clinical trial in acute LBP. J Man Ther 2005;10:61–67.
- Pinnington MA, Miller J, Stanley I. An evaluation of prompt access to physiotherapy in the management of LBP in primary care. Fam Pract 2004;21(4):372–80.
- VanTudler M, Becker A, Bekkering T, Breen A. Gil de Real M, Hutchinson A. Chapter 3 European guidelines for the management of acute nonspecific LBP in primary care. Eur Spine J 2006;15:169-191.
- Pengel LHM, Refshauge KM, Maher CG, Nicholas MK, Herbert RD, McNair P. Physiotherapist-directed exercise, advice, or both for sub-acute LBP: a randomized trial. Ann Intern Med 2007;146:787–796.
- Pengel LH, Herbert RD, Maher CG, Refshauge KM. Acute LBP: systematic review of its prognosis. BMJ 2003;327:323327.
- Mooney V. Benefits of heat therapy for lower back pain [internet]. 2003 March 20. Available at: h t t p : / / w w w . s p i n e – h e a l t h . c o m / t r e a t – m e n t / h e a t – t h e r a p y – c o l d – t h e r a – py/benefits-heat-therapy-lower-back-pain Black KM, Korn H, Nordin M. Association between sitting and occupational LBP. Eur Spine J 2007;(2):283-298.
- Lehman JF, De Lateur BJ. Therapeutic heat. In: Therapeutic Heat and Cold. 4th Ed. Baltimore, Md: Williams & Wilkins; 1990;417-581.
- Srinivasan SN. Electrotherapeutic agents manual. Jaypee-New Delhi, India, 2011.
- Belanger AY. Therapeutic Electro-physical Agents. 2nd Ed. China: Lippincott Williams and Wilkins 2009;405-6.
- Solomon DH, Bates DW, Panush RS, Katz Jn. Costs, Outcomes, and Patient Satisfaction by Provider Type for Patients with Rheumatic and Musculoskeletal Conditions: A Critical Review of the Literature and Proposed Methodologic Standards. Ann Inter Med 1997;127(1):52-60.
- Kandiah P, Tahmassebi JF. Comparing the onset of maxillary infiltration local anesthesia and pain experience using the conventional technique VS the wand in children. BDJ 2012;213(9):460-1 doi:10.1038/sj
- Koes BW, van Tulder MW, Thomas S. Diagnosis and Treatment of LBP. BMJ 2006;332(7555):1430-4.
- Shields N, Gormley J, O’Hare N. Short-wave diathermy: current clinical and safety practices. Physiother Res Int 2002;7(4):191–202.
- Foster EN, Baxter GD, McDonough SM. Physiotherapy management of LBP in Thailand: a study of practice. Physiotherapy Research International 2005;10(4):201–212.
