ABSTRACT
To determine the frequency of common musculoskeletal disorders complications among type 1 and type 2 diabetic mellitus patients and to find the association with BMI. Also, to assess the level of awareness about Physical Therapy among diabetic patients.
METHOD
A cross-sectional (descriptive) survey of diabetic patients aged above 35 years with a history of minimum 5 years of disease, taken from physical therapy unit of Karachi Pakistan. It was conducted through self-administered structured Performa, 375 patients fulfilling the inclusion criteria were selected and studied. Analysis was carried out using the statistical package for social sciences.
RESULT
There were 42.1% males and 57.9% females participated in the study. More than 90% participants were type 2 diabetics. The most common manifestations were osteoarthritis affecting both extremities (n=238), frozen shoulder (n=176), tendinitis (n=55) and fibromyalgia (n=50) noticed in both types of DM. A significant association was found between BMI and the duration of disease with respect to type 2 DM. More than half of the participants were aware of the various effects of physical therapy in diabetes.
Keywords
Musculoskeletal Disorder, Diabetes, Bmi, Physical Therapy, Hyperglycemia, Insulin.
Subhan-ur-Rehman Barki
Physiotherapist
Al-Umeed Rehabilitation Association
Hira Munawwar Khan
Senior Physiotherapist
Dr. Ziauddin Hospital
Syeda Mehreen Jilani
Physiotherapist
Dr. Ziauddin Hospital
Muhammad Nooruddin
Physiotherapist
Dr. Ziauddin Hospital
[Barki S, Khan HM, Jilani SM, Nooruddin M. Common Musculosekeltal Disorders in Diabetes Mellitus Patients.Pak. j. rehabil. 2013;2(1):35- 41].
INTRODUCTION
Insulin, a hormone that is produced by the pancreas, controls the blood glucose levels. Due to the malfunctioning of this hormone in any aspect that is, either in its production or its action or both, leads to high blood glucose levels. The inability of insulin to control the blood glucose level leads to a situation known as “Diabetes Mellitus” or hyperglycemia, which is a group of metabolic diseases1. It is a chronic condition of high morbidity and mortality2. For DM, according to American Diabetes Association classification system, there are four basic types of DM that is, “Type I DM”, “Type II DM”, “Gestational Diabetes Mellitus” (GDM) and “other specific types”. These terms emphasize on the management and treatment of DM rather than the cause of the disease3. Among these types, Type 1 DM and Type 2 DM are the most common and usually seen. In Type 1 DM, the absence of insulin leads to poor metabolism of protein, fat and carbohydrate. Type 2 DM represents approximately 90% of all cases. These patients have insufficient amount of insulin production or the amount is not balanced for their level of glycemia with primary defect in insulin resistance3.
Diabetes mellitus affect connective tissues in many ways and causes different alterations in periarticular and skeletal systems4. It can cause chronic damage which is unalterable and progressive affecting various organs and systems of the body. Although the precise cause of diabetes related musculoskeletal (MSK) disorders and complications remains uncertain, there is confirmation that hyperglycemia alters the structural matrix and mechanical properties of tissues by accelerating non-enzymatic glycosylation and abnormal collagen deposition in periarticular connective tissues leading to diffuse arthrofibrosis1. It may alter or modify the presentation, severity and pathophysiology of many musculoskeletal syndromes. Common therapies, treatments and management may differ in their effects and actions for patients with other diseases as compared to diabetic patients. Diabetes mellitus affects the musculoskeletal system of the human body, as a result, various musculoskeletal complication is seen affecting the limbs, feet and spine as a whole. Musculoskeletal complaints (MSCs) are among the major health problems worldwide and the most frequent cause of long-term sickness run off in Norway5 Increased mortality has been reported among individuals with chronic widespread MSCs, which further emphasizes that this group of patients may constitute an important public health problem. A survey was done which showed that DM was associated with higher prevalence of chronic MSCs, in particular chronic widespread MSCs6. Diabetes mellitus (DM), a worldwide high prevalence disease, is associated with a large variety of rheumatic manifestations. It acts as a base for many musculoskeletal disorders and complications, causing pain, disease or even disability which later on affects and disturbs the quality of life of an individual. If it is left untouched than the awful part is the fact it acts as a food to many rheumatic conditions and associated circumstances which becomes the major cause of crippling deformities and other disabilities for many diabetic patients. But if it is correctly diagnosed it is usually controllable by the particular handling and management given by a multidisciplinary team work7. The selected disorders are: burning of feet and numbness of feet, delayed wound healing, Callosities formation, pressure ulcers and incidence of fracture. Other musculoskeletal problems occur with increased frequency in diabetic patients, including Dupuytren’s disease, carpal tunnel syndrome, adhesive capsulitis of the shoulder.8 tendinitis, synovitis, osteoarthritis involving both, upper and lower extremities, rheumatoid arthritis, fibromyalgia and Systemic Lupus Erythematosus.
In 2004, the National Health Interview Survey determined that 58% of diabetic patients would have functional disability. Recent data show that the prevalence of MSK manifestations in the hands and shoulder in patients with type 1 or type 2 diabetes is 30%9. Statistics show increase burden of MSK diseases in diabetic patients such as degenerative joint diseases were more common (53.2%) than inflammatory arthropathies (20.1%). These manifestations, which are some of the causes of chronic disability, involve not only joints, but bones and the soft tissues as well. These manifestations are closely linked to age, prolonged disease duration and vascular complications in the form of retinopathy9. The percentages of diabetic patients with functional disability are increasing day by day as the number of diabetic patients are increasing, and hence can create a major public health problem. Physical therapy can be the mainstay treatment for diabetics suffering from musculoskeletal problems. Results from a study conducted by Hooper4 et al showed patients with diabetes mellitus can get benefit through pure immersion in a heated pool at 37 to 40 0, reduction in medication, weight and a good glycemic control were some of the benefits that were observed. Physical therapy manages the pain caused by the rheumatic manifestations and associated problems, it can also treat these musculoskeletal tribulations and at the same time works on the postural correction, stretching’s and strengthening of weak and shortened muscles in order to prevent the resulting deformities and disabilities so as to improve the different activities of daily living of diabetic patients making them independent and improving their quality of life. Most of these disorders can be diagnosed clinically, but some radiological inspection may help, especially in differential diagnosis. No definite treatment is available, and treatments used in the general population are also recommended for diabetic subjects10. A physical therapist is specially trained to decide the best option available for individual diabetic patients and some of the benefits that can be observed are Improve glucose levels, drop off use of oral hypoglycemic agents, reduce body fat and stress, and improve functioning of the circulatory system. There is a definite improvement in balance and ultimately decrease risk of fall5.
Most previous studies related to the association between diabetes and musculoskeletal syndrome have not included a control group or differentiated between type 1 and type 2 diabetes or included only a single musculoskeletal syndrome8. Therefore, no previous studies had been conducted to assess the prevalence of musculoskeletal disorders manifestations in diabetic patients or to evaluate the predisposing factors of Diabetes in Pakistan. So, the purpose of our study was not specific and covering single aspect rather, various aspects were analyzed and examined that is, to determine the frequency of most common musculoskeletal disorders among diabetic patients, which musculoskeletal disorders are more common among Type 1 DM and Type 2 DM, to find the association between DM and body mass index and to assess the level of awareness regarding effect of physical therapy to them.
METHHODOLOGY
Study Design and Setting
This was a descriptive cross-sectional study design. Theparticipants were taken from physiotherapy unit of hospitals during one year.
Sample Size and Technique
The sample size of 375 participants which was calculated by using the formula for calculating sample size on the basis of prevalence.
Prevalence was taken at 50% because no relevant data was available. The bound of error was taken at 5% with 95% confidence interval. Sample was selected through convenience sampling technique.
Inclusion Criteria
– Patients with both genders
– DM since 5 years
– Age above 35 years
Data Collection Method
Data was collected through self-administered structured Performa in Standard English language. The Performa was divided into three sections. Firstly, the demographic data was collected for all the diabetic patients including their age, gender and BMI. Secondly, the clinical information including: duration of disease (in years), type of diabetes (type 1 or 2), MSK disease found in an individual such as; Carpal Tunnel Syndrome, Osteoarthritis, Frozen Shoulder, Tendinitis, Synovitis, Rheumatoid Arthritis, Systemic Lupus Erythematosus, Fibromyalgia and Dupuytren’s Contracture, and other possible problems related to diabetes including Fracture, Burning Feet, Numbness of Feet, Delayed Wound Healing, Pressure ulcer and Callosities formation. Finally, six questions were asked to assess the level of awareness regarding the role of Physical therapy in DM.
Data Entry and Analysis
For data analysis the data was entered on SPSS version 17. Percentages and frequencies were calculated for the categorical data whereas mean and standard deviation was calculated for numerical data. Chi square was used as test of significance for finding association between different variables. P-value less than 0.05 was taken as significant.
Ethical Consideration
Participants who were fulfilling the inclusion criteria were explained the nature of the study and verbal consent was obtained from the participants. They were informed that their identity will be kept anonymous.
RESULT
A total of 375 Diabetic mellitus patients filled the Performa during the study period. The mean age of the patients including 158(42.1%) male patients while 217(57.9%) patients were female. Patient suffering DM since 5 years or more included in the study, Type 1 DM was in 57(15.2%) patients included 21 males and 36 females while Type 2 DM was in 318(84.8%) included 136 males and 182 females.
TABLE 1
The most common musculoskeletal manifestations were located among diabetic patients in respect to their specific type and it came across that osteoarthritis was affecting both upper and lower extremities (n=238), frozen shoulder (n=176), and tendinitis (n=55) fibromyalgia (n=50) were the most widespread diabetic complications noticed in both type 1 and type 2.
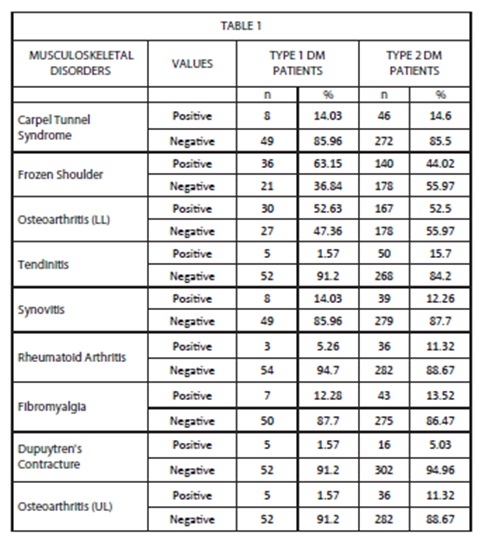
TABLE 2
The awareness concerning various effects of physical therapy, mixed association was seen. More than half of the population (83.2%) believed that physical therapist can help in relieving pain, while half of the population (48%) was aware of physical therapist role in identifyingearly changes in area at risk and in deformity prevention. Apart from fewer cases reported as shown in table 2, most of the population was unaware of physical therapist role in increasing muscle movement and strength, enhancing wound healing and maintaining blood circulation by recommending different exercises.
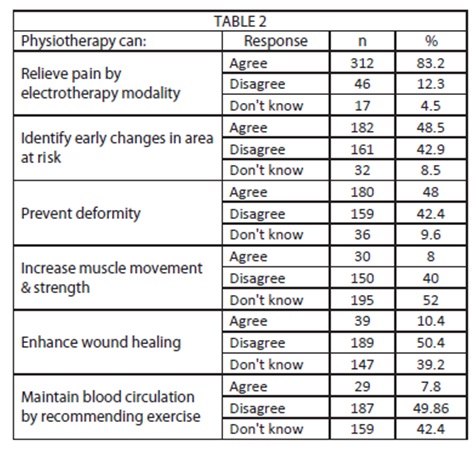
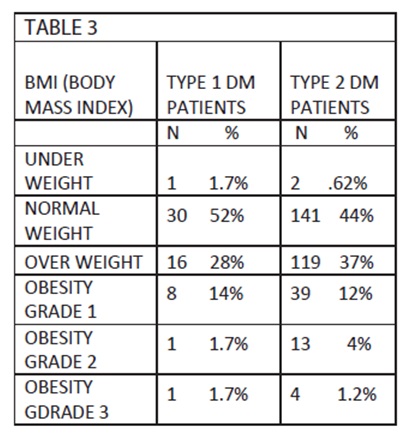
TABLE 3
A significant association was seen between the BMI and duration of DM, out of 375 diabetic patients, 175patients with overweight and obesity presented with type 2 DM whereas 143 patients were with normal weight and underweight.
No connection was seen between long standing type 1DM and overweight as minimum number of diabetes patients (n=26) were reported as overweight and obese. Hence according to table 3 patients with overweight and obesity may have a risk of type 2 DM.While studying the related disorders in diabetic patients we came across that foot problems are added observed with other major manifestations. These includes burning foot, numbness of foot, pressure ulcers and callosities formation. Among these, numbness of foot (n=173) and burning of foot (n=125) were the most frequent.
DISCUSSION
This fact cannot be denied that Diabetes mellitus is a complex disease to understand and intricate to manage. Fulfilling our aims of study, some most prevalent musculoskeletal complications (MSK) were seen in diabetic patients irrespective to its particular type. These manifestations include Adhesive capsulitis of shoulder, Osteoarthritis affecting both extremities: upper and lower, tendinitis, Fibromyalgia and Carpal tunnel syndrome as shown in table 1. A study conducted by Perttu E T Arkkila in Turku, Finland evaluated 425 diabetic patients and found a significant association in both types of diabetes mellitus and MSK complications11.
These expanding complications in diabetic patients are more often due to their highly affected muscles performance and lower limb mobility 7,11,12,13,14. This is why osteoarthritis affecting lower extremity was most frequently seen in present study as a foremost complication of Diabetes mellitus. A similar study conducted in Kolkata from November 1991 to November 2000 found an association between osteoarthritis of specifically lower extremity and diabetes mellitus15. Another study also conducted in Kolkata from 2003-2005, 80 patients were studied out of which 43 patients presented with rheumatological disorders. Among these diabetic patients’ frozen shoulder, carpal tunnel syndrome and limited joint mobility were more general13. Reported by P E Arkkila in his cross-sectional study on diabetic patients revealed frozen shoulder as the common diabetic complication present in both types of DM11.
In our study most common diabetic complication associated to type 1 DM were frozen shoulder, osteoarthritis affecting lower extremity, carpal tunnel syndrome and synovitis were present with similar frequency and fibromyalgia whereas no significant association was seen in tendinitis and osteoarthritis affecting upper extremity with type 1 DM. According to one study conducted by Singh R at Auckland, New Zealand reported a strong association between risk of developing carpal tunnel syndrome and type 1 DM16.
A strong relation was seen in type 2 DM and diabetic manifestations including frozen shoulder15, carpal tunnel syndrome and osteoarthritis affecting lower extremity15. Some disorders were strongly linked to type 2 DM than type 1 DM that is, these disorders were more frequent in type 2 DM than type 1 DM such as tendinitis(n=50 Vs n=5), rheumatoid arthritis(n=36 Vs n=3) and fibromalgia(n=43 Vs n=7). Apart from frozen shoulder and Osteoarthritis affecting lower extremity, few cases of musculoskeletal complications were seen in type 1 DM. Therefore, we concluded that type 1 diabetic patients are comparatively less affected with MSK disorders9,17. Similar results were also obtained by a study done by Suzan. M. attar in which MSK complications were more common in type 2 DM, 252 patients were included in the study 45 patients suffered from musculoskeletal complications, maximum patients (91%) had type 2 DM. Their findings also suggested frozen shoulder and carpal tunnel syndrome as the most frequent manifestation in type 2 DM9. Similar study conducted in Giaziantep, turkey also found frozen shoulder as the most common complication1.
A pilot study carried out at Hippokration University Hospital in Thessaloniki, Greece revealed osteoarthritis as the most frequently encountered MSK complication in type 2 diabetic patients4. Another cross-sectional study carried out at Adnan Menderes University Hospital in Giaziantep, turkey observed 102 patients and found dupuytren’s contracture the most frequent MSK complication in type 2 diabetic patients1. According to some similar studies dupuytren’s contracture was found as the most frequent diabetic complication present in both types of diabetes with almost equal ratio. (14,18) but in agreement with the present study dupuytren’s contracture (n=21) was not found to be the most common complication and it was comparatively more common in type 2 diabetes.
According to Yanmaz MN and Mert M fibromyalgia was more common in patients suffering from type 2 DM as compared to type 1 DM19. Similarly in the present study fibromyalgia was more frequently seen in type 2 DM patient than type 1 (n=43 Vs n=7) where as another study conducted in Zerifin, Israel, found an association between fibromyalgia and DM20 According to them fibromyalgia was almost equally significant in both types of DM, in contrast to our study we found its significance more in type 2 DM.
A strong correlation between tendinitis and type 2 diabetes was suggested by the study of M E Mavrikakis conducted at Alexandra General Hospital in Athens, Greece, who enrolled 824 adult type 2 diabetics and deep-rooted an association between the tendinitis and type 2 diabetes21 as also observed in the present study.
In the present study it was analyzed that more cases of degenerative disorders such as osteoarthritis reported comparatively than inflammatory disorders such as carpal tunnel syndrome, tendinitis and synovitis. A similar study conducted at Bangabandhu Sheikh Mujib medical university, Dhaka to find the pattern of MSK disorders, 2062 patients were examined and came to a conclusion that degenerative disorders are more frequent than inflammatory ones of MSK in diabetic patients22. Similar results were also observed in our study that with in 375 patients, degenerative disorders such as osteoarthritis were more common in diabetic patients than inflammatory disorders such as carpal tunnel syndrome, tendinitis and synovitis. In the current study we found an association linking MSK manifestations and its features with long term diabetes mellitus. In such patients, with the growing age, amplified number of MSK problems were seen as also previously reported in some studies 23,24,25. In company with the prevalence of common MSK complication in long standing diabetes mellitus, we also merged one more aspect of related problems in our questionnaire in order to further investigate common complications and related MSK disorders of foot. It is usually observed that diabetic patients typically go through foot problems along with major MSK manifestations and it is also noticed in our study as well that maximum number of diabetic patients reported several foot problems in which burning feet (n=125) and numbness of feet (n=173) were the most widespread. In previous studies it has been established that foot complications account for 20% of all diabetic patients because of disturbed sensibility7. According to another study, diabetic foot complications were the most common and serious manifestation in diabetic patients noticed14.
Another association was established in the present study between the body mass indexes (BMI) and chronic diabetes mellitus as shown in table 3. We found that about 60% (n=175) of diabetic patients were overweight or obese and presented with type 2 DM. Whereas a small number of obese diabetic patients (n=26) were categorized in type 1 DM. Overweight or obese people may have a danger of developing DM. In relation to one cross-sectional epidemiologic study conducted covering rural, suburban and urban areas of Greece between 1996-1999, accomplished a strong association connecting type 2 DM and obesity26. A survey done by CDC in United States to unearth the prevalence of overweight and obesity among diabetic adults. The report was based on two surveys done by “Third National Health and Nutritional Examination” (NHANES III), 1998-1994 and NHANES III 1999-2002. They indicated that the mainstreams of adults with diagnosed DM were cluster into overweight or obese and their dominance was 85.2%27.
In our part of the world, due to lack of proper education and consistent awareness programs, it is hard to assess the level of awareness regarding physical therapy and its various effects. As shown in table 2, most of the population were aware from the general effects of physical therapy that is, physical therapist can relieve pain by using electrotherapy modalities but conversely, people are still unaware from the advantageous and therapeutic effects of physical therapy in variety of aspects that is, either we talk about its role in prevention or in maintenance or even in increasing muscles movement and strength. Unfortunately, no prior studies were performed to assess the level of awareness concerning effects of physical therapy. Therefore, present study would be of assistance in terms of providing a snap shot of the present awareness status regarding field of physical therapy so that further recommendations can be taken consequently.
The limitation of the study is that only those cases of diabetes were included in the study which visited to the tertiary care hospital, diabetic centers and nearby residents otherwise more actual snap shot of the musculoskeletal disorders could be observed as most of the patient visits private clinics.
REFERENCE
- Aydeniz A, Gursoy S, Guney E. Which musculoskeletal complications are most frequently seen in type 2 diabetes mellitus?. Journal of International Medical Research 2008;36(3):505-511
- Serban AL, Udrea GF, Parhon CI. Rheumatic manifestations in diabetic patients. Journal of Medicine and Life Available at URL: http://www.medandlife.ro/medandlife727.html
- Wyatt, Lawrence H. and Randy J. Ferrance. The musculoskeletal effects of diabetes mellitus. The Journal of the Canadian Chiropractic Association 2006;50(1):43
- Douloumpakas I, Pyrpasopoulou A, Triantafyllou A et al. Prevalence of musculoskeletal disorders in patients with type 2 diabetes mellitus. Hippokratia. 2007 Oct-Dec;11(4):216–218
- Report of a WHO Scientific Group. The burden of musculoskeletal conditiona at the start of the new millinium, WHO Technical Report Series 919.2003. Available at URL: http://whqlibdoc.who.int/trs/WHO_TRS_919.pdf
- Hoff, Ole M et al. The association between diabetes mellitus, glucose, and chronic musculoskeletal complaints. Results from the Nord-Trøndelag Health Study. BMC musculoskeletal disorders 2008;9(1):160.
- Ahmad I, Nadeem D, Aziz A. Musculoskeletal disorder in long-standing DM Cases. JPOA 2008 FEB;20(1):38
- Cagliero E, Apruzzese W et al. Musculoskeletal disorders of the hand and shoulder in patients withdiabetes mellitus. Coronary artery disease 2002;7(40):0-01
- Attar, Suzan M. Musculoskeletal manifestations in diabetic patients at a tertiary center. Libyan Journal of Medicine 2013;7(1)
- Arkkila PE, Gautier J. Musculoskeletal disorders in diabetes mellitus: an update. Best practice &research. Clinical rheumatology 2003;17(6):945
- Arkkila PE, Kantola IM, Viikari JS ,et al., Shoulder capsulitis in type I and II diabetic patients: association with diabetic complications and related diseases. Ann Rheum Dis 1996;55:907–914
- Giacomozzi C, D’Ambrogi E, Cesinaro S et al. Muscle performance and ankle joint mobility in long-term patients with diabetes. BMC musculoskeletal disorders 2008;9(1):99
- Sarkar RN, Banerjee S, Basu AK et al. Rheumatological manifestations in diabetes mellitus. J Indian Med Assoc 2008;106(9):593-4.
- Vencovský J. Rheumatologic manifestations in diabetes]. nitr n l kar stv 2006;52(5):481.
- Sarkar RN, Banerjee S, Basu AK et al. Rheumatological manifestations in diabetes mellitus. J Indian Med Assoc 2008;106(9):593-4.
- Singh R, Gamble G, Cundy T. Lifetime risk of symptomatic carpal tunnel syndrome in Type 1 diabetes. Diabetic medicine 2005;22(5):625-630
- Ramchurn N, Mashamba C, Leitch E, etl. Upper limb musculoskeletal abnormalities and poor metabolic control in diabetes. European Journal of Internal Medicine 2009;20(7):718-721
- Renard E, Jacques D, Chammas M et al. Increased prevalence of soft tissue hand lesions in type 1 and type 2 diabetes mellitus: various entities and associated significance. Diabete & metabolisme 1993;20(6):513-523
- [19] Yanmaz MN, Mert M, Korkmaz M. The prevalence of fibromyalgia syndrome in a group of patients with diabetes mellitus. Rheumatology international 2012;32(4):871-874
- Tishler M, Smorodin T, Vazina-Amit M et al. Fibromyalgia in diabetes mellitus. Rheumatology international 2003;23(4):171-173
- Mavrikakis M, Drimis S, Kontoyannis D et al. Calcific shoulder periarthritis (tendinitis) in adult onset diabetes mellitus: a controlled study. Annals of the rheumatic diseases 1989;48(3):211-214
- Khan S, Shakoor, Islam Q et al. Pattern of Musculoskeletal Disorders among Diabetic Patients Attending a Tertiary Care Hospital in Dhaka. Ibrahim Medical College Journal 2008;2(2):65-66.
- Nathan D. Long-term complications of diabetes mellitus. New England Journal of Medicine 1993;328(23):1676-1685
- Bañón S, Isenberg DA. Rheumatological manifestations occurring in patients with diabetes mellitus. Scandinavian journal of rheumatology 2013;42(1):1-10.
- Saadi H, Carruthers S, Nagalkerke N et al. Prevalence of diabetes mellitus and its complications in a population-based sample in Al Ain, United Arab Emirates. Diabetes research and clinical practice 2007;78(3):369-377.
- Tentolouris N, Andrianakos A, Karanikolas G,et al. Type 2 diabetes mellitus is associated with obesity, smoking and low socioeconomic status in large and representative samples of rural, urban, and suburban adult Greek populations. Hormones (Athens, Greece) 2012;11(4):458.
- Eberhart MS, Ogden C, Engelgau M et al. Prevalence of Overweight and Obesity among Adults with Diagnosed Diabetes—United States, 1988–1994 and 1999–2002. Morbidity and Mortality Weekly Report 2004;53(45):1066-1068.
