Zoha Sabir[i], Rimsha Hassan[ii], Maria Bashir[iii], Rida Akhtar[iv], Ayesha Mehmood[v], Sana Bashir[vi]
DOI: 10.36283/pjr.zu.11.2/012
ABSTRACT
Background and Aim: Polycystic Ovarian Syndrome is an endocrine problem and its prevalence is on rise day by day in Pakistan, so the study aimed to determine occurrence of Anxiety and Depression among women with Polycystic Ovarian Syndrome and to check whether quality of life gets poor or not in relation to Polycystic Ovarian syndrome.
Methodology: It was a descriptive cross-sectional study, data was sampled using non-probability convenient sampling technique and analyzed on SPSS v. 20.0. Study was done on 150 participants, from Fauji Foundation Hospital and different private setups of Rawalpindi/Islamabad. Data was collected through Beck Depression Inventory, Beck Anxiety Inventory and SF-36 Questionnaires respectively.
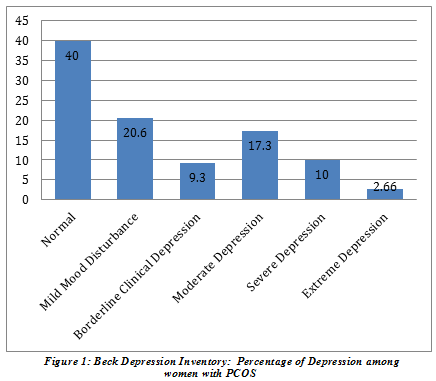
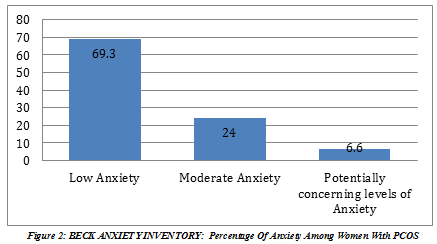
Results: Mean age of the all patients was (24.7±5.9), and BMI was (23±5.1). Out of 150 participants, (40%) were normal, (20.60%) had mild mood disturbance, (17.3%) had moderate depression and (2.66%) had extreme depression. Similarly, (69.3%) of the participants had normal anxiety level and only (6.60%) had potentially concerning levels of anxiety. Mean and standard deviation for different domain of SF-Questionnaire was: physical functioning (70.1±25), physical health limitations were (50±34), emotional problems limitations (42.9±37), energy/fatigue (49.7±15.2), for emotional wellbeing was (55±14.7), for social functioning was (65±24.5), pain (65.6±23), and general health were (51.2±18) respectively.
Conclusion: Study concluded that occurrence of anxiety and depression among women with poly cystic ovarian syndromes was low, hence and their quality of life was not much affected.
Keywords: Polycystic ovarian syndrome (PCOS), quality of life (QOL), social phobia, anxiety, infertility, depression.
Introduction
Anxiety is defined as an immoderate and improper concern that is continuous and incapacitating1. Epidemiological surveys have found that one third population is affected by Anxiety during their life time. Its prevalence was found to be highest during the midlife, and is more common in women2.The possible causes of anxiety among women with PCOS include obesity, social phobia, hirsutism, panic attacks, infertility and obsessive compulsive disorder that may require further screening3. By definition, depression is an illness that involves the body, mood, and thoughts and that affects the way a person eats, sleeps, feels about himself of ineffectiveness and dependence with narcissistic desires4.Exercise has found to have a major antidepressant effect upon people with depression5.
Polycystic Ovarian Syndrome (PCOS) is an endocrine condition with multiple characteristic signs and symptoms that are grouped together into a disorder with varying presentation among different individuals. The primary features of PCOS are irregular menstruation, high levels of androgens, and PCOS. Affected individuals presents with infrequent menstruation or absence of menstruation, excess body hair, increased weight and inability to conceive6. It involves several body systems that are responsible for metabolic and reproductive complications risk factors associated with PCOS includes type 2 DM, cardiovascular events (hypertension) and mental health problems, depression and anxiety etc.7.Occurrence of PCOS is found to be notably high in women in Pakistan (8) The prevalence of PCOS among females in Pakistan is 52% higher as compared to white population (20-25% in UK)9. The frequency of Polycystic Ovarian Syndrome extends between 66-10% according to the National Institute of Health10. The Rotterdam diagnostic criteria established in 2003 aiming to guide the clinicians a proper diagnosis of PCOS, according to which a PCOS patient must present with at least two of these three symptoms (anovulation or oligo ovulation, polycystic ovaries on ultrasonography, biochemical or clinical signs of hyperandrogenism) (11). Females with Polycystic Ovarian Syndrome have high possibility of developing clinically relevant anxiety, comorbid anxiety and depression, anxiety has found to be contributing to impaired QOL among PCOS population12. Another study had reported that females with Polycystic Ovarian Syndrome have increased chance for acquiring depression related problems13. Another study also showed that PCOS women, were associated with high probability of mood swings, along with high risk for depression (14) Another study suggested that depression and anxiety is more common in females with PCOS as compared to the healthy females, and depression may be associated with obesity, metabolic abnormalities including dyslipidemia and insulin resistance15 Women afflicted with PCOS suffer from mental health problems, which ultimately affect their functioning in activities of daily living. Poor psychological QOL was found to be associated with hirsutism, anxiety and depression among PCOS women. (16) Both weight loss and use of oral contraceptive pills lead to significant changes in multiple physical and mental realms linked to QOL syndromes of depression and anxiety disorders, and combined treatments offer additional benefits for overweight/obese females with PCOS17 A cohort study conducted in 2017, found strong association between MDD (major depressive disorder), Neuroticism with Polycystic Ovarian Syndrome18. A longitudinal review conducted on January 2020 also concluded that females with PCOS complain of poor life satisfaction, decreased HRQOL and inferior health status19. Another study conducted in year 2019, also concluded that, occurrence of depression and anxiety in females with PCOS was greater compared to the non-PCOS women. Moreover, increased testosterone levels were correlated with mood disorders and anti-androgen treatment tended to reduce emotional processing in women with PCOS20 A study conducted in year 2020 stated, that aerobic exercise tends to improve sexual function and also enhances individual’s psychological state by reducing anxiety and depression among PCOS women21.
Methodology
Study Design
It was a descriptive cross sectional study.
Study Duration
Study was held within duration of 6 months, i.e. July 2019-December 2019.
Study Setting
The data was collected from Fauji Foundation Hospital and different private setups within Rawalpindi and Islamabad.
Sampling Technique
Non-probability purposive sampling was performed.
Inclusion Criteria
Females medically diagnosed with PCOS (conferring to Rotterdam Criteria a female should have 2 of the following 3 attributes): Raised androgenic hormonal levels, distended ovaries containing at least 12 follicles each, ovulatiory Irregularities, Females belonging to the reproductive age group of 18 to 35 years old.
Exclusion Criteria
Females not medically diagnosed with Polycystic Ovarian Syndrome or not belonging to the reproductive age group of 18 to 35 years old.
Data Collection Tools
Beck Depression Inventory (BDI): It is a 21 itemed questionnaire, used for measuring depression, each of the questions had 4 options with a scoring ranging from (0-3), and the higher the score the greater would have been depression, it had helped classifying depression into six levels based on scores: • 1-10: Normal • 11-16: Mild Mood Disturbance • 17-20: Borderline Clinical Depression • 21-30: Moderate Depression • 1-40: Severe Depression • 40: Extreme
Beck Anxiety Inventory (BAI): It is a 21 itemed questionnaire, used to measure anxiety levels, each of the questions had 4 options with a scoring ranging from (0-3), and the higher the score the greater would have been anxiety, it had helped classifying anxiety into three levels based on scores: • Low Anxiety • Moderate Anxiety • Potentially Concerning Levels of
Short Form Survey (SF36) RAND: The tool comprises of eight domains concluding two main measures: physical and mental health. Physical health included four scales of physical functioning (10 items), bodily pain (2items), general health (5 items) and role physical (4 items). The mental health comprised of social functioning (2 items), role emotional (3 items), vitality (4 items) and mental health (5 items). The scoring was done using a standardized scoring algorithm to obtain scoring ranging from 0 to 100. The greater the scores the better will be the Quality of Life.
Data Collection Procedure
Research Committee of Foundation University Islamabad gave ethical approval for the study. Then, an official permission letter was attained by Institutional Research Committee. After collecting the informed consent and providing explanation regarding the study
Data Analysis Procedure
Statistical Analysis was done using SPSS v. 21.
Ethical Concerns
As per university guidelines, “The ethical review committee of Foundation University” made sure that there were no ethical violations in the research. In addition, ethical principles of honesty, consistency and consent form an integral part of research safety, for which informed consent was obtained from our study participants. Before acquiring data from individual participants, permission was taken from HOD’s of respective hospitals. Participants were given complete freedom to withdraw from the study.
Results
Total numbers of study participants were 150. It was female (women) based study.
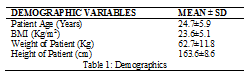
BDI included six categories and our results showed the percentages as: 40% normal, 20.67% mild mood disturbance, 9.33% borderline clinical depression, 17.33% severe depression and 10% extreme depression respectively.
69.33% of the participants had low anxiety, 24% had moderate anxiety and 6.6% had potentially concerning levels of anxiety.
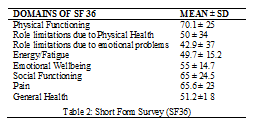
RAND 36-Item Health Survey was used to asses’ quality of life, lowest and highest possible scores of each domain range from 0 to 100 and higher scores indicate more satisfactory health status. The results of this study showed that, mostly affected domain with comparatively low scores were role limitations due to emotional problems with mean ± standard deviation of 42.9 ± 37, followed by energy and fatigue of 49.7 ± 15.2 and least affected domain with better functional outcomes was physical functioning with mean ± standard deviation of 70.1 ± 25.
OUTCOME MEASURES (TOOLS)
- Beck Depression Inventory (BDI)
- Beck Anxiety Inventory (BAI)
- Short Form Survey (SF36) RAND
Discussion
According to this study, prevalence of anxiety was found to be less, with only 7% within females suffering from PCOs. A similar study conducted on prevalence of anxiety, cognitive and depression evaluation among young adolescents and healthy girls with PCOS, revealed that, anxiety and depression among them was found to be low. (1)The findings of which directly correspond with our study results.
Otherwise, according to latest evidences from various studies people with PCOS suffer from increased occurrence of depression and anxiety, social phobia and poor quality of life (2) Also females with PCOS are at an increased jeopardy of anxiety linked mood disorders; which pose them to have increased risk of generalized anxiety disorders (3). Women with PCOs are more likely to develop clinically relevant anxiety, comorbid anxiety and depression, anxiety among these contributing conditions, stands out to be most closely linked to impaired QOL among PCOS population (4). Another similar study, showed increased mood disorders risk (as per DIAGNOSTIC AND STATISTIC MANUAL IV) and concluded with high rates of depression in females with PCOS. (5). Evidences also report that, increased risk of anxiety and depression among women with PCOs is correlated directly with emerging signs and symptoms such as infertility, hirsutism and obesity. Therefore, majority of PCOS females present with obesity, social phobia, hirsutism, panic attacks, infertility and obsessive compulsive disorders (6). These symptoms ultimately tend to weaken or reduce patient’s self-esteem, moral and social confidence, which in turns poorly affect their health status and Quality of life in general (7) So, altogether, all of these studies’ findings contradict with the findings of our study.
Hence, it can be commented on the fact that, if stress levels get higher, quality of life gets poor ultimately but in our PCOS population, contradictory results were found in this regard, as levels of depression and anxiety were found to be low that’s why they had good quality of life as well yet.
Conclusion
The findings of our research have concluded that occurrence of anxiety and depression is low in the population particularly in Rawalpindi and Islamabad which might be due to increasing awareness among women regarding this disease. As a result, their QOL in females with PCOS, including physical, psychological, social, sexual and medical aspects, is not as severely compromised as previous studies around the globe have shown.
Acknowledgment
We will especially appreciate the substantial efforts of our mentor Dr. Muhammad Ehab Azim, for sharing generously and humbly, his vast knowledge, experience and skills with us
References
- Kabadayi Sahin E, Turan G, Neselioglu S, Can SS, Atagun MI. Thiol-disulphide homeostasis in patients with general anxiety disorder and panic disorder. Dusunen Adam The Journal of Psychiatry and Neurological Sciences. 2019;32(4):289.
- Bandelow B, Michaelis S. Epidemiology of anxiety disorders in the 21st century. Dialogues in clinical neuroscience. 2015;17(3):327.
- Zafar U, Memon Z, Moin K, Agha S, Hassan JA, Zehra D. Prevalence of PCOS with associated symptoms and complications at Tertiary Care Hospital of Karachi. Journal of Advances in Medicine and Medical Research. 2019:1-9.
- Chaudhari AP, Mazumdar K, Mehta PD. Anxiety, depression, and quality of life in women with polycystic ovarian syndrome. Indian journal of psychological medicine. 2018;40(3):239-46.
- Schuch FB, Vancampfort D, Richards J, Rosenbaum S, Ward PB, Stubbs B. Exercise as a treatment for depression: a meta-analysis adjusting for publication bias. Journal of psychiatric research. 2016;77:42-51.
- Hart R. Generational health impact of PCOS on women and their children. Medical Sciences. 2019;7(3):49.
- Kollmann M, Klaritsch P, Martins W, Guenther F, Schneider V, Herzog S, et al. Maternal and neonatal outcomes in pregnant women with PCOS: comparison of different diagnostic definitions. Human Reproduction. 2015;30(10):2396-403.
- Akram M, Roohi N. Endocrine correlates of polycystic ovary syndrome in Pakistani women. J Coll Physicians Surg Pak. 2015;25(1):22-6.
- Rao M, Broughton KS, LeMieux MJ. Cross-sectional Study on the Knowledge and Prevalence of PCOS at a Multiethnic University. Progress in Preventive Medicine. 2020;5(2):e0028.
- Coutinho EA, Kauffman AS. The role of the brain in the pathogenesis and physiology of polycystic ovary syndrome (PCOS). Medical Sciences. 2019;7(8):84.
- Arentz S, Smith CA, Abbott J, Bensoussan A. Perceptions and experiences of lifestyle interventions in women with polycystic ovary syndrome (PCOS), as a management strategy for symptoms of PCOS. BMC women’s health. 2021;21(1):1-8.
- Moghadam ZB, Fereidooni B, Saffari M, Montazeri A. Measures of health-related quality of life in PCOS women: a systematic review. International journal of women’s health. 2018;10:397.
- Greenwood EA, Yaffe K, Wellons MF, Cedars MI, Huddleston HG. Depression over the lifespan in a population-based cohort of women with polycystic ovary syndrome: longitudinal analysis. The Journal of Clinical Endocrinology & Metabolism. 2019;104(7):2809-19.
- Koivuaho E, Laru J, Ojaniemi M, Puukka K, Kettunen J, Tapanainen J, et al. Age at adiposity rebound in childhood is associated with PCOS diagnosis and obesity in adulthood—longitudinal analysis of BMI data from birth to age 46 in cases of PCOS. International Journal of Obesity. 2019;43(7):1370-9.
- Kakoly N, Moran L, Teede H, Joham A. Cardiometabolic risks in PCOS: a review of the current state of knowledge. Expert review of endocrinology & metabolism. 2019;14(1):23-33.
- Mirghafourvand M, Charandabi SM-A, Aliasghari F. Predictors of depression in Iranian women with polycystic ovarian syndrome. Community mental health journal. 2018;54(8):1274-83.
- Çoban ÖG, Tulacı ÖD, Adanır AS, Önder A. Psychiatric disorders, self-esteem, and quality of life in adolescents with polycystic ovary syndrome. Journal of pediatric and adolescent gynecology. 2019;32(6):600-4.
- Standeven LR, Olson E, Leistikow N, Payne JL, Osborne LM, Hantsoo L. Polycystic Ovary Syndrome, Affective Symptoms, and Neuroactive Steroids: a Focus on Allopregnanolone. Current psychiatry reports. 2021;23(6):1-10.
- Karjula S, Morin-Papunen L, Franks S, Auvinen J, Järvelin M-R, Tapanainen JS, et al. Population-based data at ages 31 and 46 show decreased HRQoL and life satisfaction in women with PCOS symptoms. The Journal of Clinical Endocrinology & Metabolism. 2020;105(6):1814-26.
- Sukhapure M. Androgens and the Female Brain: The Relationship between Testosterone Levels, Depression, Anxiety, Cognitive Function, and Emotion Processing in Females with Polycystic Ovarian Syndrome: University of Otago; 2019.
- Kogure GS, Lopes IP, Ribeiro VB, Mendes MC, Kodato S, Furtado CLM, et al. The effects of aerobic physical exercises on body image among women with polycystic ovary syndrome. Journal of affective disorders. 2020;262:350-8.
- Greenwood E, Pasch L, Legro R, Cedars M, Huddleston H. Quality of life and depression in polycystic ovary syndrome. Fertility and Sterility. 2017;108(3):e64-e5.
- Abdollahi L, Mirghafourvand M, Babapour JK, Mohammadi M. Effectiveness of cognitive-behavioral therapy (CBT) in improving the quality of life and psychological fatigue in women with polycystic ovarian syndrome: a randomized controlled clinical trial. Journal of Psychosomatic Obstetrics & Gynecology. 2019;40(4):283-93.
- Kerchner A, Lester W, Stuart SP, Dokras A. Risk of depression and other mental health disorders in women with polycystic ovary syndrome: a longitudinal study. Fertility and sterility. 2009;91(1):207-12.
- Azizi Kutenaee M, Amirjani S, Asemi Z, Taghavi S-A, Allan H, Kamalnadian S-N, et al. The impact of depression, self-esteem, and body image on sleep quality in patients with PCOS: a cross-sectional study. Sleep and Breathing. 2020;24(3):1027-34.
The Ziauddin University is on the list of I4OA (https://i4oa.org/) & I4OC (https://i4oc.org/).
![]() This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY 4.0). https://creativecommons.org/licenses/by/4.0/
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY 4.0). https://creativecommons.org/licenses/by/4.0/
Conflict of Interest: The author (s) have no conflict.
[i] Demonstrator, Foundation University Institute of Rehabilitation Sciences (FUIRS)
ORCID ID: 0000-0001-6018-9544
[ii] Student, Foundation University Institute of Rehabilitation Sciences (FUIRS)
ORCID ID: 0000-0002-4805-1283
[iii] Student, Foundation University Institute of Rehabilitation Sciences (FUIRS)
ORCID ID: 0000-0001-6832-662X
[iv] Student, Foundation University Institute of Rehabilitation Sciences (FUIRS)
ORCID ID: 0000-0001-8341-5663
[v] Student, Foundation University Institute of Rehabilitation Sciences (FUIRS)
ORCID ID: 0000-0002-9974-7002
[vi] Senior Lecturer Foundation University Institute of Rehabilitation Sciences (FUIRS) Foundation University Islamabad (FUI)
ORCID ID: 0000-0002-3472-8564
