Muhammad Shahzad Qadree[i] , Syed Shakil-ur-rehman[ii] , M Usman Riaz[iii] , Mehwish Anees[iv] , Hira Islam Rajput[v]
DOI: 10.36283/pjr.zu.11.2/013
ABSTRACT
Background: Sciatica or more commonly sciatic nerve pain is characterized by low back pain that radiates down towards knee or below knee, paresthesia associated with tingling or numbness and weakness of muscles of foot and leg. Most important cause of sciatica is herniated disc which cause nerve root entrapment. Other causes may include lumbar stenosis or spinal tumors. The goal of the study is to determine the effects of graston instrument technique soft tissue mobilization in patients with sciatic nerve entrapment.
Methods: Patients were recruited and allocated randomly in two groups. Group A (Lumbar traction with neural mobilization) and Group B (Graston technique along with lumbar traction and neural. 4 weeks of intervention were given to both groups.
Results: The 4 weeks treatment session resulted in a significant improvement in pain reduction and improved MODI in patients of group B (Graston technique along with lumbar traction and neural mobilization), which was not more apparent in the group A (lumbar traction with neural mobilization manipulation group). Graston technique along with lumbar traction and neural mobilization was found to be more effective than lumbar traction and neural mobilization alone.
Conclusion: This study concluded that Graston technique together with neural mobilization and lumbar traction was successful in alleviating pain and impairment in patients with sciatic nerve entrapment. Together with neural mobilization and lumbar traction, the Graston technique considered more superior to neural mobilization along with lumbar traction alone in terms of the aforementioned outcome measures dependent on means.
Keywords: Sciatica, low back pain, traction, impairment, NPRS, MODI
Introduction
Sciatica or more commonly sciatic nerve pain is characterized by low back pain that radiates down towards knee or below knee, paresthesia associated with tingling or numbness and weakness of muscles of foot and leg1. Comorbidities such as depression and anxiety in low back pain are linked to neuropathic pain2. Most important cause of sciatica is herniated disc which cause nerve root entrapment. Other causes may include lumbar stenosis or spinal tumors3. It is for the most part evaluated that 5%-10% of populace with low back pain have sciatica while the lifetime pervasiveness of low back pain ranges from 49%-70%. Yearly pervasiveness of sciatica related with IVD is assessed at 2.2%4. Sciatic nerve entrapment may occur between pelvis and distal thigh. Most instances of entrapment happen between more noteworthy sciatic notch and ischial tuberosity5. Medical management of sciatica includes anti-inflammatory drugs (NSAID’s), skeletal muscle relaxant, opioid analgesics, anti-depressants, benzodiazepines and corticosteroids6.Conservative treatment for sciatic nerve entrapment includes manual therapy, stretching and strengthening exercises, aerobics and cognitive behavioral education. Neural mobilization is a technique of manual therapy that improves neurodynamic by nerve movements and surrounding structures. Soft tissue mobilization is also manual therapy intervention and is applied at musculo-tendinous structures affecting the nerves. Soft tissue mobilization administered with specialized instrument7. For the treatment of radiating pain that is related to intervertebral disc pathology nerve mobilization techniques have been used and particularly, nerve mobilization for sciatic nerve is used. These components can mitigate low back pain. With the assistance of neural-mobilization strategies, harms to the sciatic nerves might be expelled or reduced, torment might be diminished, scope of movement might be expanded, and dynamic flexibility of the sensory system might be uplifted, serving to patients to utilize their bodies without obstruction8.Various techniques for lumbar traction for example mechanical, mechanized or with the assistance of gravity are normally fused in clinical practice to oversee different lumbar conditions. The components are dubious however, it was expected that lumbar traction isolates vertebral bodies to make space and lessens compressive powers on the disc, diminishes the pressure on nerve root by expanding the size of the intervertebral foramen, and assists with restoring the herniated plates to their unique situation by creating strain on spinal tendons. Given it’s across the board use in clinical practice, the clinical impacts of lumbar traction on low back agony related with intervertebral disc herniation are dubious9. Instrument assisted soft tissue mobilization (IASTM) is a requesting treatment for myofascial limitation. The strategy of IASTM is applied by uniquely created instruments. They give an activating mobilizing impact to scar tissue and also in adhesions that may shape in muscles and belt. Various IASTM instruments and strategies are accessible, for example, the graston strategy. The method of IASTM is applied by utilizing uncommonly created instruments to give a mobilizing impact to delicate tissue (e.g., scar tissue, myofascial adhesions) to lighten torment and improve scope of movement (ROM) and functional capacity10. The clinical utilization of instruments that may incorporate in treatment appears to upgrade treatment adequacy, especially in regions of fibrosis. The actuation of tissue microtrauma is accepted to bring out a nearby incendiary reaction that advances breakdown of scar tissue, adhesions, blend of new collagen, and connective tissue renovating11. There are a few unique ideas of IASTM, every one of which gives their own instruments and accreditation or preparing programs. Graston Technique and Tecnica gavilan are two of the most mainstream draws near. The literature on IASTM is yet creating, with the significant piece of the exploration on case reports and contextual investigations with barely any controlled trials12. Moon JH colleagues conducted a study on instant effects of graston technique for improving flexibility of hamstrings muscles in people suffering from non-specific low back pain. Twenty-four patients (27-46 years of age) with nonspecific low back pain participated in this study. In experimental group the technique of graston was used, while in control group static stretching was performed. Sit and reach test is used to assess hamstring extensibility, and to measure pain intensity numeric pain rating scale was used. A notable increase in sit and reach test and NPRS scores was observed (p<0.05) when graston technique was used. Sit and reach test measurements before and after intervention showed significant difference in graston group. In NPRS values there were no statistically significant changes. The graston technique is a simple and effective treatment for people suffering with nonspecific low back pain to build hamstring flexibility and lower torment seriousness, and it tends to be valuable in clinical practice13. Jeong-Hoon Lee collegues directed an examination to research the impacts of graston system on the discomfort and range of motion in patients suffering from low back torment. 30 patients with incessant low back agony took an interest in the investigation (Graston procedure: 15 Control: 15). Before and after a 4-week therapeutic programme, pain was measured using visual analogue pain (VAS). Smart phone was used to measure Lumbar ROM. For VAS and ROM, a significant time-by-group interaction was observed. Both groups showed significant increase in the lumbar ROM. Graston group indicated essentially increment ROM and diminished VAS more than control gathering. These discoveries demonstrate that the Graston technique is successful in pain reduction or may have an increase in the range of motion as a result of this treatment in patients with chronic low back pain14. In 2019 Goris Nazari PT led a precise systematic review to judge the efficacy of delicate tissue mobilization assisted with instruments (IASTM) in additional treatments, or as a test substance in runners or members without furthest point or spinal conditions and in individuals with lower limb, upper limb, and spinal conditions. Nine studies contrasted instrument assisted activation results with other treatments with 43 reported outcomes including function, pain, range of movement and grip strength quality. Six trials showed no clinically significant changes in outcomes between two groups with thirty-six outcomes. After conducting two trials clinically important differences revealed in two outcomes favoring the other treatment group without instrument assisted mobilization of soft tissues15. A randomized clinical trial on the efficacy of mechanical traction in patients with low back pain was led by Julie M Fritz. 120 patients participated in this study with pain in lower back and signs of aggravation in nerve roots. For extension bias approach participants were randomized, with or without the use of mechanical traction system. The primary outcome measure was modified Oswestry questionnaire to measure disability. Statistical analysis was found on intention to treat principles and linear mixed model analysis was used to compare them. This trial gave a methodologically thorough assessment of the adequacy of utilizing traction for patients with low back agony and indications of aggravation of nerve root treatment groups16. Marie-Eve Isner-Horobet conducted a randomized clinical trial in 2016 on high strength traction against low strength traction in lumbar region in patients with sciatica secondary to intervertebral disc protrusion. Patients who received lumbar traction for about fourteen days in sciatica secondary to intervertebral disc prolapse demonstrated improvement in their pain which is of radicular origin, improved status of thier functional impairments and overall improved health and welfare nevertheless of the group of traction force to which they were assigned17. Giovanni E Ferreira collegues led a randomized clinical preliminary on neurodynamic treatment to improve agony and disability in patients with chronic nerve related leg pain. Sixty participants allocated in this study. The experimental group got four neurodynamic treatment sessions. All groups got counsel to remain locked in. There were no significant between-group differences in disabilities and area of symptoms at about a month. At about fourteen days adding neurodynamic treatment to stay dynamic did not improve leg pain and disability 19,20.
Material and Methods
An experimental study (RCT) was conducted in the physiotherapy department of Fatima Memorial Hospital (FMH) located in Lahore, Pakistan. The trial is registered having reference number # IRCT20191130045554N1. The study was approved from ethical review committee of Riphah International University. Convenient sampling technique has been used for the randomization of patients. Twenty patients are recruited to study. The duration of the current study was 6 months. Only male patients aged between 30 to 60 years are recruited to study. Patients diagnosed with sciatica along with radicular pain in lower back with duration of less than 12 weeks after onset and the patients having Pain upon active SLR in 30-70̊ sensitivity 0.6719 specificity 0.2620. Patients were not included in study if they exhibited spinal Fracture, Spinal tumor or any malignancy, Psychiatric Disorder, History of Osteoporosis, Rheumatologic disorders, Pain beyond 70̊ or below 30̊ on active SLR, Positive compression and distraction test of SI joint. And positive gaenslen’s test. Participants were recruited into Group A and Group B by lottery method (without replacement). Each member was approached to draw either A or B cards from a box. Alphabet A will be allocated to Group A and alphabet B will be allocated to B group. Lumbar Traction along with Neural Mobilization was given to Group A participants for 4 weeks, 3 sessions per week. Sustained mechanical lumbar traction was applied on patient with average of 30-45kg for 10 min(18). Garston Technique along with lumber traction and neural mobilization was given to Group B participants for 4 weeks, 3 sessions per week. During 4-weeks the Graston group recieved IASTM (Instrument Assisted Soft Tissue Mobilization) on posterior fascia, sacrum, and lateral rotators of hip and hamstring bilaterally. In the first, subjects were required to kneel directly on the bed. The posterior fascia IASTM was use to stimulate the lumbar posterior muscles i.e., erector spinae (iliocostalis, longissimus), as well as the multifidus. Subjects were instructed to kneel down on the bed for instrument assisted soft tissue mobilization (IASTM) on sacral region. For IASTM of hip lateral rotators, position of the patient is prone kneeling with knee and hip flexion and for IASTM on gluteus Maximus and gluteus medius the preferred position is side lying. In the prone position, IASTM was applied to hamstrings tendon which includes biceps femoris, semitendinosus and semimembranosus. The IASTM treatment was performed for about twenty seconds in a direction parallel to the muscle fibers being treated with the instrument at a 45° angle with instrument. Continuing that, for yet another twenty seconds treat the muscles in a path perpendicular to the muscle fibers with the instrument at 45° angle, for a total treatment period of around forty seconds. Mechanical traction unit was used to apply sustain lumbar traction. Graston instruments of Rocktape Company were used for IASTM. Neural mobilization of sciatic nerve was performed in straight leg raise with dorsiflexion of foot. Data collection tool that were used in this study are numeric pain rating scale having reliability and validity of 0.96 and 0.86-0.9521 respectively and modified oswestry disability index having reliability and validity of 0.91 and 0.7522 respectively.
Data Analysis
After collecting data from defined study setting, data was entered and analyzed at Riphah International University, Lahore by using Statistical Package for the Social Sciences (SPSS) for windows software, version 25. Statistical significance was set at P=0.05. In descriptive Statistics the summary of group measurement are shown by using Frequency tables and Clustered bar charts over time. In Inferential Statistics Normality of the data was assessed using Shapiro Wilk test. Based on p-values parametric and non-parametric tests was decided. Difference between groups was assessed by independent sample T test/ Mann-Whitney U test. Difference within each group was assessed by two-way ANOVA.
Results
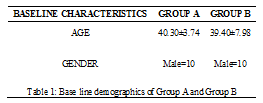
Baseline values of both groups’ sociodemographic data were equivalent on the basis of to mean± std. The mean age of Group A participants was 40.30±3.74 years compared to Group B 39.40±7.98 years.
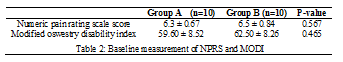
Both groups were similar in NPRS and MODI at baseline treatment values with value of p greater than 0.05. The mean NPRS values for Group A and Group B were 6.3±0.67, and 6.5±0.84 respectively. The mean MODI values for Group A and Group B were 59.60±8.52 and 62.50± 8.26, respectively.
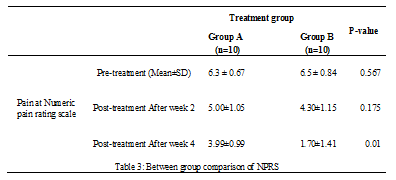
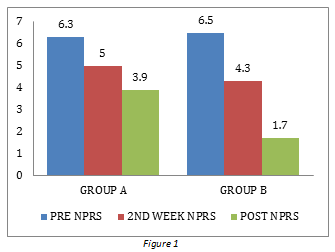
For comparing NPRS pretreatment and post treatment between two groups. Independent T-test was performed and findings showed there was no significant statistically difference between pre-treatment NPRS values of two groups with p value greater than 0.05. In Group B, the NPRS score falls to a greater extent with a mean value of 1.70±1.41 compared with Group A 3.99±0.99 in post-treatment 4th week.
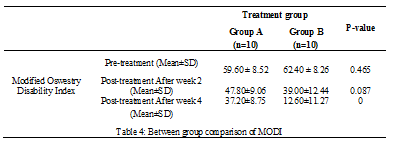
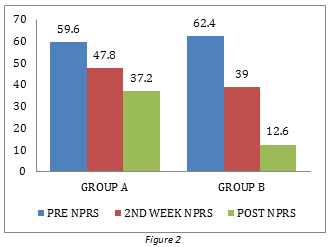
To compare pre& post-treatment MODI between two groups Independent sample t-test was used. Findings demonstrate there was no significant statistically difference between pre-treatment MODI values of two groups with p value greater than 0.05.
MODI score decreases to greater extent in post treatment In Group B, the MODI level falls to a greater extent in the 4th week post-treatment with a mean value of 12.60 ±11.27 than in Group A 37.20±8.75.
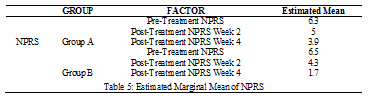
For PRS, the approximate marginal mean was measured in Group A and Group B, respectively. In Group B, the approximate mean was reduced to a greater degree in the 4th week post-treatment than in Group A.
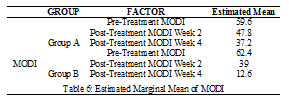
The estimated marginal mean for MODI was evaluated in groups A and B respectively. In Group B, the estimated marginal mean was reduced to a greater extent in the 4th week post-treatment relative to Group A.
Clustered bar graph indicates trend improvement in NPRS from pretreatment to post treatment week 4, which has been steadily improved in both groups but higher in Group B than in Group A.
A progress pattern in MODI from pre-treatment to post-treatment week 4 was shown in the clustered bar chart, which was steadily rising in both groups but higher in Group B compared to Group A.
Discussion
The goal of the current study was to determine the effect of graston instrument soft tissue mobilization on pain and functional disability in patients with sciatic nerve entrapment. Sciatic nerve pain is characterized by low back pain that radiates down towards knee or below knee, paresthesia associated with tingling or numbness and weakness of muscles of foot and leg(1). Sciatic nerve entrapment may occur from pelvis to distal thigh. Most trapping cases occur between greater sciatic tuberosity and ischial tuberosity. At the level of greater sciatic piriformis syndrome caused by piriformis muscle trapping of the sciatic nerve5.
The findings of the current study indicate that both groups at baseline treatment levels of p-value > 0.05 were identical at NPRS and MODI. Between group A and group B the mean value of NPRS was 6.3±0.67 and 6.5±0.84 respectively. The mean MODI values for Group A and Group B were 59.60±8.52 and 62.50± 8.26 respectively.
The current study results show that there was no statistically significant difference between pretreatment NPRS and MODI values of 02 groups with p value > 0.05. In group B, NPRS and MODI decreased to a greater extent in the 4th week post-treatment with mean value 1.70±1.41 and 12.60±11.27 respectively compared with group A 3.99±0.99 and. 37.20±8.75. Intensity of pain and level of disability decreases more in group B because of additional graston technique with base line treatment i.e., Lumbar traction and neural mobilization. A similar study was conducted in patients with low back pain to assess the effects of graston correlate with general exercises. Their results showed that graston technique decreased pain in low back pain patients. Their findings suggest graston technique to treat and rehabilitate patients with chronic low back pain14.
The present study had several limitations. Firstly, no longer follow up was conducted, usually a six to eight weeks or longer intervention period has been used for significant progress. Secondly, sample size was small and lastly the study was limited to male gender. Further research is needed to investigate the long-term effects of graston instrument on pain and disability in patients with sciatica.
Conclusion
This study concluded that Graston technique together with neural mobilization and lumbar traction was effective in reducing pain and impairment in patients with sciatic nerve entrapment, provided that statistically significant differences between two treatment groups were observed. Together with neural mobilization and lumbar traction, the Graston technique considered more superior to neural mobilization along with lumbar traction alone in terms of the aforementioned outcome measures dependent on means.
Reference
- Xiang A, Xu M, Liang Y, Wei J, Liu S. Immediate relief of herniated lumbar disc-related sciatica by ankle acupuncture: A study protocol for a randomized controlled clinical trial. Medicine. 2017 Dec;96(51):e9191.
- Jungen MJ, ter Meulen BC, van Osch T, Weinstein HC, Ostelo RWJG. Inflammatory biomarkers in patients with sciatica: a systematic review. BMC Musculoskeletal Disorders. 2019;20(1):156. doi: 10.1186/s12891-019-2541-0.
- Koes BW, van Tulder MW, Peul WC. Diagnosis and treatment of sciatica. BMJ (Clinical research ed). 2017 Jun 23;334(7607):1313-7.
- Younes M, Béjia I, Aguir Z, Letaief M, Hassen-Zrour S, Touzi M, et al. Prevalence and risk factors of disk-related sciatica in an urban population in Tunisia. Joint Bone Spine. 2016;73(5):538-42.
- Jackson TJ. Endoscopic Sciatic Nerve Decompression in the Prone Position-An Ischial-Based Approach. Arthroscopy techniques. 2016;5(3):e637-42. Epub 2016/09/23. doi: 10.1016/j.eats.2016.02.020. PubMed PMID: 27656390; PubMed Central PMCID: PMCPMC5021545.
- Pinto RZ, Maher CG, Ferreira ML, Ferreira PH, Hancock M, Oliveira VC, et al. Drugs for relief of pain in patients with sciatica: systematic review and meta-analysis. BMJ (Clinical research ed). 2012;344:e497.
- Martin R, Martin HD, Kivlan BR. NERVE ENTRAPMENT IN THE HIP REGION: CURRENT CONCEPTS REVIEW. International journal of sports physical therapy. 2017 Dec;12(7):1163-73.
- Jeong UC, Kim CY, Park YH, Hwang-Bo G, Nam CW. The effects of self-mobilization techniques for the sciatic nerves on physical functions and health of low back pain patients with lower limb radiating pain. Journal of physical therapy science. 2016 Jan;28(1):46-50.
- Cheng Y-H, Hsu C-Y, Lin Y-N. The effect of mechanical traction on low back pain in patients with herniated intervertebral disks: a systemic review and meta-analysis. ClinicalRehabilitation.0(0):0269215519872528.
- Cheatham SW, Lee M, Cain M, Baker R. The efficacy of instrument assisted soft tissue mobilization: a systematic review. The Journal of the Canadian Chiropractic Association. 2016 Sep;60(3):200-11.
- Baker RT, Nasypany A, Seegmiller JG, Baker JG. Instrument-assisted soft tissue mobilization treatment for tissue extensibility dysfunction. International Journal of Athletic Therapy and Training. 2013;18(5):16-21.
- MacDonald N, Baker R, Cheatham SW. THE EFFECTS OF INSTRUMENT ASSISTED SOFT TISSUE MOBILIZATION ON LOWER EXTREMITY MUSCLE PERFORMANCE: A RANDOMIZED CONTROLLED TRIAL. International journal of sports physical therapy. 2016 Dec;11(7):1040-7.
- Kim J, Sung DJ, Lee J. Therapeutic effectiveness of instrument-assisted soft tissue mobilization for soft tissue injury: mechanisms and practical application. Journal of exercise rehabilitation. 2017 Feb;13(1):12-22.
- Moon JH, Jung JH, Won YS, Cho HY. Immediate effects of Graston Technique on hamstring muscle extensibility and pain intensity in patients with nonspecific low back pain. Journal of physical therapy science. 2017 Feb;29(2):224-7.
- Lee JH, Lee DK, Oh JS. The effect of Graston technique on the pain and range of motion in patients with chronic low back pain. Journal of physical therapy science. 2016 Jun;28(6):1852-5.
- Nazari G, Bobos P, MacDermid JC, Birmingham T. The Effectiveness of Instrument-Assisted Soft Tissue Mobilization in Athletes, Participants Without Extremity or Spinal Conditions, and Individuals with Upper Extremity, Lower Extremity, and Spinal Conditions: A Systematic Review. Archives of Physical Medicine and Rehabilitation. 2019;100(9):1726-51.
- Fritz JM, Thackeray A, Childs JD, Brennan GP. A randomized clinical trial of the effectiveness of mechanical traction for sub-groups of patients with low back pain: study methods and rationale. BMC musculoskeletal disorders. 2010 Apr 30;11:81.
- Isner-Horobeti M-E, Dufour SP, Schaeffer M, Sauleau E, Vautravers P, Lecocq J, et al. High-force versus low-force lumbar traction in acute lumbar sciatica due to disc herniation: a preliminary randomized trial. Journal of manipulative and physiological therapeutics. 2016;39(9):645-54.
- Ferreira G, Stieven F, Araujo F, Wiebusch M, Rosa C, Plentz R, et al. Neurodynamic treatment did not improve pain and disability at two weeks in patients with chronic nerve-related leg pain: a randomised trial. Journal of physiotherapy. 2016;62(4):197-202.
- Pourahmadi M, Hesarikia H, Keshtkar A, Zamani H, Bagheri R, Ghanjal A, et al. Effectiveness of Slump Stretching on Low Back Pain: A Systematic Review and Meta-analysis. Pain medicine (Malden, Mass). 2019;20(2):378-96. Epub 2018/12/28. doi: 10.1093/pm/pny208. PubMed PMID: 30590849.
- Rabin A, Gerszten PC, Karausky P, Bunker CH, Potter DM, Welch WC. The sensitivity of the seated straight-leg raise test compared with the supine straight-leg raise test in patients presenting with magnetic resonance imaging evidence of lumbar nerve root compression. Archives of physical medicine and rehabilitation. 2007;88(7):840-3.
- Devillé WL, van der Windt DA, Dzaferagic A, Bezemer P, Bouter LM. The test of Lasegue: systematic review of the accuracy in diagnosing herniated discs. Spine. 2000;25(9):1140-7.
- Ferraz MB, Quaresma M, Aquino L, Atra E, Tugwell P, Goldsmith C. Reliability of pain scales in the assessment of literate and illiterate patients with rheumatoid arthritis. The Journal of rheumatology. 1990;17(8):1022-4.
- Mousavi SJ, Parnianpour M, Mehdian H, Montazeri A, Mobini B. The Oswestry disability index, the Roland-Morris disability questionnaire, and the Quebec back pain disability scale: translation and validation studies of the Iranian versions. Spine. 2006;31(14):E454-E9.
- Harte AA, Baxter GD, Gracey JH. The efficacy of traction for back pain: a systematic review of randomized controlled trials. Archives of Physical Medicine and Rehabilitation. 2003;84(10):1542-53.
The Ziauddin University is on the list of I4OA (https://i4oa.org/) & I4OC (https://i4oc.org/).
![]() This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY 4.0). https://creativecommons.org/licenses/by/4.0/
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY 4.0). https://creativecommons.org/licenses/by/4.0/
Conflict of Interest: The author (s) have no conflict.
[i]Senior Demonstrator FMH Institute of Allied Health Sciences Fatima Memorial Hospital
ORCID ID: 0000-0001-5270-0939
[ii] Professor and Director, Riphah College of Rehabilitation Sciences
ORCID ID: 0000-0002-6682-9896
[iii] Assistant Professor & HOD Physical Therapy Department FMH Physiotherapy Department Fatima Memorial Hospital
ORCID ID: 0000-0002-5287-9665
[iv] Senior Demonstrator FMH Institute of Allied Health Sciences. Fatima Memorial Hospital
ORCID ID: 0000-0003-3514-1287
[v] Assistant Professor Taqwa Institute of Physical Therapy. Health Sciences
ORCID ID: 0000-0001-8250-5827
