ABSTRACT
BACKGROUND AND AIM
Quadratus lumborum trigger points developed in low back pain. The aim of this study was to compare Reciprocal Inhibition with Ischemic Pressure on the Trigger Point of Quadratus Lumborum muscle in Low Back Pain.
METHODOLOGY
A 6 month randomized controlled trial was conducted. Non probability Convenience sampling was used to select a sample 50 participants having low back pain with Quadratus lamborum trigger points placed into group1 and group 2 by lottery method. Group 1 was treated with reciprocal inhibition and ischemic pressure along with conventional therapy and group 2 was treated with ischemic pressure along with conventional therapy. The data collection tools were Numeric pain rating scale and Goniometer. Data was analyzed by statistical package for social science 21. Independent t-test used for between comparison analysis and Paired t-test was used for within analysis.
RESULTS The numeric pain rating scale mean difference in group 1 and group 2 was 4.72±0.12, 5.13±0.13 respectively. The Quadratus lamborum muscle length mean difference in group 1 and group 2 was 8.95±1.67, 5.34±1.25 respectively.
CONCLUSION
The addition of reciprocal inhibition with ischemic pressure showed significant results.
KEY WORDS
reciprocal Inhibition, ischemic pressure, quadratus lumborum, Back Pain, Myofascial Trigger Point Pain, Articular Goniometry, range of motion
Muhammad Sanaullah
Senior Lecturer RCR&AHS Riphah International University Lahore
HOD/Associate Professor Department of Rehabilitation Sciences
ORCID ID:0000-0001-8315-4256
Abdul Ghafoor Sajjad
HOD/Associate Professor
Department of Rehabilitation Sciences
Shifa Tameer e Millat University Islamabad.
ORCID ID:0000-0002-4797-975X
Muhammad Atif Javed
Senior Lecturer RCR&AHS Riphah International University LahoreCampus
ORCID ID:0000-0003-2099-632X
Muhammad Faheem Afzal
Assistant professor Rehabilitation Department PSRD College of Rehabilitation Sciences.
ORCID ID:0000-0003-2549-6850
[Sanaullah M, Sajjad AG, Javed MA, et al. Effect Of Reciprocal Inhibition with Ischemic Pressure on the Trigger Point of Quadratus Lumborum Muscle in Low Back Pain
Pak.j.rehabil. 2022; 11(1):99-106]
DOI: 10.36283/pjr.zu.11.1/013
INTRODUCTION
The area of low back pain is between gluteal fold and costal margin1. The classification of low back pain according to time period is acute, subacute and chronic and according to cause is specific and non-specific2. The risk factors of low back can be age, educational status, psychological issues, job satisfaction, occupational factors and obesity3. Low back pain is one of the main cause of disability4.
The stability of lower back is mainly depends upon the muscles in that region. These are called core stabilizers. Among these muscles quadratus lamborum is responsible for extension, flexion and side bending of lumber region5. Quadratus lamborum is also involved in lower back stability but this muscle is overlooked6.
Trigger points are tender region in taut band of skeletal muscles. They are multiple foci present in trigger zone7. In American population it was found that 44 million people having low back pain also had myofascial trigger point8. In another study researcher found that 30 percent patient having low back pain also had myofascial trigger point9. 55% musculoskeletal pain is cause by myofascial pathologies. Overuse of muscle cause myofascial trigger points10. In lower back instability the stablizers work beyond their limits. As quadratus lamborum is also a stabilizer of lower back so triggers point can develop in quadratus muscle11.
There are many Diagnostic criteria for myofascial trigger points. According to Simmons a patient had trigger point if he met five major criteria and one minor criteria. The major criteria in Simmons study were localized spontaneous pain, altered sensation in trigger point area, the involved muscle should contain taut band, localized tenderness and decrease in range of motion. The Minor criteria included spontaneous pain and twitch response on pressure and pain relieved by stretching12.
Treatment of myofascial trigger point include Medicine interventions, psychotherapy, behavioral therapy, chiropractic and physiotherapy. Dry needling, wet needling13. In Physiotherapist there are multiple interventions which are used such as modalities, manual therapy and muscle energy techniques14.
Post isometric relaxation (PIR) and post facilitation stretch (PFS) are included in muscle energy technique. In PIR technique the hypertonic muscle lengthen to barrier where resistance is encounter. The patient will apply force on therapist hand. When patient relax his muscle Therapist will lengthen the muscle to next resistance. Stretching in this stage is contraindicated. In PFS technique patient will exert maximum force on therapist hand in mind range. Therapist will apply stretch after patient relax. In reciprocal inhibition therapist place the patient affected muscle in mid-range and guided to contract maximally either isotonic or isometric pattern. When patient stop contraction he will be instructed to inhale and exhale at the same time therapist will lengthen the muscle to new barrier15. If we add reciprocal inhibition with ischemic pressure there will be increase in range of motion and pain will decrease in myofascial trigger point of quadratus lumborum in low back pain.
METHODOLOGY
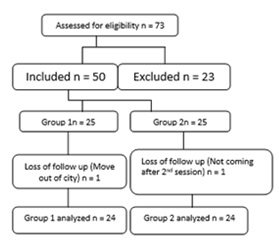
Data was collected from Riphah Rehabilitation department in Pakistan Railway General Hospital Rawalpindi. It was randomized control trial. 50 patients of low back pain having trigger point of Quadratus lumborum were included in the study by Non-probability convenient sample technique and randomly assigned in two groups using lottery method. Statistician was blinding in this study. (Group 1=25 and Group 2=25). Physical therapist assesses the patients having Low back pain with quadratus lumborum involvement, Twitch response in muscle and taut band on palpation were included (using Simmons diagnostic criteria). Patients having acute injury, prolapsed inter vertebral disc and recent surgery were excluded. Data was collected through Numeric pain rating scale (NPRS) for pain and Goniometry for the length of Quadrates lumborum muscle. In NPRS patient was instructed to tick the number in given scale, 10 indicated unbearable pain and 0 indicate no pain16. The length of quadrates lumborum muscle length was measured when patients were in standing position and side flexion5. A total of 73 patients 23 were excluded. Out of 50 patients 25 patients assigned to each group. One patient from group1 and one patient from group 2 were dropped out. 24 patients in each groups were present for further study. Measurements were taken before the 1st visit and at the end of last session. Each patient was treated for 4 consecutive sessions.
Group 1 was treated TENS was applied for 10 min having frequency 100Hz and duty cycle 250µs17. Hot pack was applied for 10 min18. Ischemic pressure was applied on trigger point in prone lying up to tolerance of patient for 20 to 60 seconds and repeat for 3 to 5 times. (19) For Stretching of quadratus lumborum (QL) patient was placed in position as lying supine, head and legs moved in banana position opposite to affected QL. After 20 seconds of maintaining banana position patient will move back to resting position. The procedure was repeated 5 to 6 times. Reciprocal inhibition for QL was performed in supine position. Patient asked to place his hands behind the neck. Therapist was standing behind the patient, while bending trunk opposite from involved QL therapist hold opposite shoulder for 10 seconds and repeat for 5 times. In Group 2 TENS, hot pack, ischemic pressure and Stretching of quadratus lumborum protocol were applied and their protocol was same as in group 1.
Data was analyzed by statistical package for social science 21. Shapiro-wilk test was used to assess normality. As data was normally distributed so Independent t-test used for between comparison analysis and Paired t-test was used for within group analysis.
CONSORT DIAGRAM
ETHICAL CONSIDERATION
The ERC of Riphah international university approved the research and Pakistan Railway General Hospital allow to conduct the study in their setting with ref No RIPHAH/RCRS/REC/00166. The consent was taken from patients.
RESULTS
The mean age of group 1 was 44.5±13.5, and group 2 was 42.1±9.9, the male participant in group 1 were 91.7% and in group 2 were 66.7%, the female participant in group 1were 8.3% and in group 2 were 33.3%. In group 1 87.5% participant were railway employ, in group 2 66.7% were house wives. (Table I)
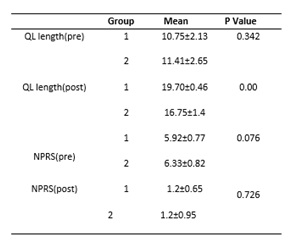
Quadratus lamborum muscle length and numeric pain rating scale were compared between groups (Table II). Group 1 was treated with reciprocal inhibition in addition to baseline treatment. The pre QLML mean was 10.75±2.13 the post QLML mean was 19.70±0.46 and mean difference was 8.95±1.67. The pre NPRS was 5.91±0.77 and post NPRS was 1.20±0.65 and mean difference was 4.71±0.12.
The Group 2 was treated with baseline treatment and the pre QLML mean was 11.41±2.65the post QLML mean was 16.75±1.4and mean difference was 2.34±1.25. The pre NPRS was 6.3±0.81and post NPRS was 1.29±0.95 and mean difference was 5.01±0.14. When between groups analysis was performed the P value of QLML before treatment was 0.342 and after treatment was 0.00. There was no significant improvement in NPRS (p=0.726).
Table I: Demographic Data of all 48 patients.
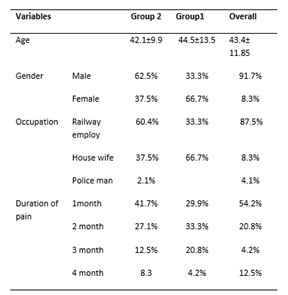
Table II: Changes in Muscle Length and Pain between Group Comparisons.
DISCUSSION
There was significant improvement (p<0.05) in NPRS and QLML in both groups. The mean difference for QLML in group 1 was 8.95±1.67 and in group 2 was 2.34±1.2. The mean difference of NPRS in groups 1 was 4.71±0.12 and in group 2 was 5.01±0.14. When both groups were compared the p value of QLML was <0.001 and of NPRS was 0.726. Results showed that when reciprocal inhibition added with ischemic pressure there will be increase in the QLML.
G.Yatheendra Kumar et.al in 2015 compare MET with Ischemic pressure for Trp of trapezius muscle. The mean difference of VAS for ischemic compression was 4.4 and for MET was 0.38. The mean difference of ROM for ischemic compression was 11 and for MET was 14.6. In this study we combine reciprocal inhibition with ischemic compression the mean difference for NPRS was 4.72 and for ROM was 8.95. If we compare with previous study the improvement in pain and ROM was almost same20.
Amit V. Nagrale et al in 2010 compare MET with integrated with neuromuscular inhibition technique (INIT) the mean difference of VAS in MET group was 0.93 and in INIT group was 1.18. The mean difference of ROM in MET group was 1.6 and in INIT group was 3.73. In our study we combine reciprocal inhibition with ischemic compression the mean difference for NPRS was 4.72 and for ROM was 8.95. the result showed that if we add MET with ischemic pressure there will be more improvement in pain and ROM instead of MET alone used in previous study21.
Rabia noor et.al in 2016 combine MET with strain-counter strain (SCS) for TrP of trapezius muscles. The mean difference of VAS was 4.5. In this study, the combination of reciprocal inhibition and ischemic compression shows the mean difference for NPRS was 4.72.the result showed that there will be same effects if we add MET with ischemic pressure or SCS22.
Hugh Gemmell et.al in 2008 conducted a study to compare ischemic pressure (IC) with trigger point release (TrP release) on trapezius muscle. The mean difference of VAS in TrP release group was 1.67 and in IC group was 1.83. The MD of ROM in TrP release group was 5.5 and in IC group was 0.2. The results show that there was no significant difference between ischemic pressures and trigger point release. By comparing with this study results showed that by adding MET with ischemic pressure give better results than ischemic pressure alone23.
Kostopoulos, D, et.al. Studied the effect of ischemic pressure and passive stretch on trapezius muscle trP. The results showed that ischemic pressure was more significant than passive stretch and when these two techniques were combined there were more significant results for pot treatment reading (2.45) in VAS. Cesar fernandaz et.al in 2005 conduct a systemic review about effect of ischemic pressure (IP) on trigger point along with other techniques like modalities, exercise and stretching. They concluded that combining IP with other techniques give better results. An article in that review showed the post treatment mean of pain was 2.46 when combining IP with Hot pack, TENS and active ROM. In current study IP was combined with hot pack, TENS and stretching. By comparing the mean of post treatment pain score with current study (1.2) there was more improvement in pain as compare to previous studies 24,25.
Rickards, L.D. in 2006 conducted a systemic review of non-invasive treatment effects on myofascial trigger points (mTrP). He concluded that TENS was also effective for mTrP. He also concluded that ischemic pressure and traditional thigh massage are equally significant. Results showed that Ischemic pressure and sustained stretch gives better results than active ROM exercises 26.
CONCLUSION
Ischemic pressure had effect on myofascial trigger points. When reciprocal inhibition added with ischemic pressure there will be significant improvement in pain and range of motion for myofascial trigger point in low back pain.
AKNOWLEDMENT
I am very thankful to my supervisor Abdul Ghafoor Sajjad. The cooperation of Riphah Rehabilitation department in Pakistan Railway General Hospital Rawalpindi to allow me for data collection.
REFERENCE
- Raja MP. A Comparative Study on Abdominal Strengthening Exercise with Interferential Therapy versus Back Strengthening Exercise with Interferential Therapy in Acute Low Back Pain.2020:19-4.
- Hall H. Low Back Patterns of Pain: Classification Based on Clinical Presentation. Handbook of Spine Technology. 2021:3-25.
- Balagué F, Mannion AF, Pellisé F, Cedraschi C. Non-specific low back pain. The lancet. 2012 Feb 4; 379(9814):482-91.
- Mescouto K, Olson RE, Hodges PW, Setchell J. A critical review of the biopsychosocial model of low back pain care: time for a new approach? Disability and Rehabilitation. 2020 Nov 18:1-5.
- Phillips S, Mercer S, Bogduk N. Anatomy and biomechanics of quadratus lumborum. Proceedings of the Institution of Mechanical Engineers, Part H: Journal of Engineering in Medicine. 2008 Feb 1; 222(2):151-9.
- Giamberardino MA, Affaitati G, Fabrizio A, Costantini R. Myofascial pain syndromes and their evaluation. Best practice & research Clinical rheumatology. 2011 Apr 1; 25(2):185-98.
- Jiménez-Sánchez C, Gómez-Soriano J, Bravo-Esteban E, Mayoral-del Moral O, Herrero-Gállego P, Ortiz-Lucas M. The effect of dry needling of myofascial trigger points on muscle stiffness and motoneuron excitability in healthy subjects. Acupuncture in Medicine. 2021 Jul 20:09645284211027579.
- Gerwin RD. Myofascial pain syndrome. InMuscle pain: diagnosis and treatment 2010 (pp. 15-83). Springer, Berlin, Heidelberg.
- Nikam DP, Varadharajulu DG. Effect of Variants of Positional Release Technique vs. Ischemic Compression Technique on trigger point in Myofascial Pain Syndrome: A randomized controlled trial. (2021). Int. J. Life Sci. Pharma Res.; 11(2):L54-57.
- Lucas KR. The effects of latent myofascial trigger points on muscle activation patterns during scapular plane elevation. Melbourne. RMIT University, School of Health Sciences (Dissertation). 2007 Mar.
- Giamberardino MA, Affaitati G, Fabrizio A, Costantini R. Myofascial pain syndromes and their evaluation. Best practice & research Clinical rheumatology. 2011 Apr 1; 25(2):185-98.
- Gross JM, Fetto J, Rosen E. Musculoskeletal examination. John Wiley & Sons; 2015 Jun 29.
- Nasb M, Qun X, Ruckmal Withanage C, Lingfeng X, Hong C. Dry cupping, ischemic compression, or their combination for the treatment of trigger points: a pilot randomized trial. The Journal of Alternative and Complementary Medicine. 2020 Jan 1; 26(1):44-50.
- Li L, Stoop R, Clijsen R, Hohenauer E, Fernández-de-Las-Peñas C, Huang Q, Barbero M. Criteria Used for the Diagnosis of Myofascial Trigger Points in Clinical Trials on Physical Therapy: Updated Systematic Review. The Clinical Journal of Pain. 2020 Dec 22; 36(12):955-67.
- Chaitow L, Crenshaw K. Muscle energy techniques. Elsevier Health Sciences; 2006.
- Young IA, Dunning J, Butts R, Mourad F, Cleland JA. Reliability, construct validity, and responsiveness of the neck disability index and numeric pain rating scale in patients with mechanical neck pain without upper extremity symptoms. Physiotherapy theory and practice. 2019 Dec 2; 35(12):1328-35.
- Dias LV, Cordeiro MA, de Sales RS, dos Santos MM, Korelo RI, Vojciechowski AS. Immediate analgesic effect of transcutaneous electrical nerve stimulation (TENS) and interferential current (IFC) on chronic low back pain: Randomised placebo-controlled trial. Journal of Bodywork and Movement Therapies. 2021 Jul 1; 27:181-90.
- Metgud SC, Monteiro SS, Heggannavar A, D’Silva PV. Effect of integrated neuromuscular inhibition technique on trigger points in patients with nonspecific low back pain: Randomized controlled trial. Indian Journal of Physical Therapy and Research. 2020 Jul 1; 2(2):99.
- Togha M, Bahrpeyma F, Jafari M, Nasiri A. A sonographic comparison of the effect of dry needling and ischemic compression on the active trigger point of the sternocleidomastoid muscle associated with cervicogenic headache: A randomized trial. Journal of back and musculoskeletal rehabilitation. 2020 Jan 1; 33(5):749-59.
- Kumar GY, Sneha P, Sivajyothi N. Effectiveness of Muscle energy technique, Ischaemic compression and Strain counterstrain on Upper Trapezius Trigger Points: A comparative study. International journal of physical education, sports and Health. 2015; 1(3):22-6.
- Nagrale AV, Glynn P, Joshi A, Ramteke G. The efficacy of an integrated neuromuscular inhibition technique on upper trapezius trigger points in subjects with non-specific neck pain: a randomized controlled trial. Journal of Manual & Manipulative Therapy. 2010 Mar 1; 18(1):37-43.
- Manzoor A, Anwar N, Haider R, Saghir M, Javed MA. Comparison of effectiveness of muscle energy technique with Mulligan mobilization in patients with non-specific neck pain. JPMA. The Journal of the Pakistan Medical Association. 2021 Mar 5; 71(6):1532-24.
- Gemmell H, Miller P, Nordstrom H. Immediate effect of ischaemic compression and trigger point pressure release on neck pain and upper trapezius trigger points: A randomised controlled trial. Clinical Chiropractic. 2008 Mar 1; 11(1):30-6.
- Kostopoulos D, Nelson Jr AJ, Ingber RS, Larkin RW. Reduction of spontaneous electrical activity and pain perception of trigger points in the upper trapezius muscle through trigger point compression and passive stretching. Journal of musculoskeletal pain. 2008 Jan 1; 16(4):266-78.
- De las Peñas CF, Campo MS, Carnero JF, Page JC. Manual therapies in myofascial trigger point treatment: a systematic review. Journal of bodywork and movement therapies. 2005 Jan 1; 9(1):27-34.
- Rickards LD. The effectiveness of non-invasive treatments for active myofascial trigger point pain: a systematic review of the literature. International journal of osteopathic medicine. 2006 Dec 1; 9(4):120-36.
