ABSTRACT
The pediatric cancer cases diagnosed each year is increasing at a rapid rate. With high health risks and infant mortality associated to pediatric cancer, it is crucial to recognize educational and psychosocial support among patients and caregivers to alleviate care burden. To provide them with intensive supportive care in the initial phase and equipping them to deliver specialized treatment is valuable to the child health. Thus, a qualitative and exploratory study was conducted at a Private-Tertiary Care Hospital in Karachi. Through purposive sampling, participants (N=10) were selected to conduct in-depth interviews. The data was analyzed via Qualitative content analysis method through manual and using NVIVO 11 software. The themes were constructed from the categories emerged from the data codes. The result signifies four themes that indicate stressful experience among family and children with newly diagnosed pediatric cancers substantially require mental health professionals for emotional strength, there is utmost necessity of a multidisciplinary team to increase their health literacy, inadequate educational support due to limited access to resources, and insufficient psychosocial support system with healthcare setting. The findings also highlight that child’s level of understanding of diseases, language barrier, and financial crisis also impede support provision. The initial phase of childhood cancer demands appropriate individualized educational psychosocial interventions, psychological assistance to improve coping responses, and increased exposure of social support groups in assisting patients and families. Formulating new policies, need-focused services, psychoeducation, and future research are discussed.
KEYWORDS
Pediatric cancer, caregiver, education, psychosocial, supportive care, healthcare, children, Pakistan
Bibi Maryam
Aga Khan University Stadium Road Karachi Pakistan
ORCID ID: 0000-0002-1359-1060
Dr. Tazeen Saeed
School of Nursing and Midwifery Aga Khan University Stadium Road Karachi Pakistan
ORCID ID: 0000-0002-8896-8766
Dr. Sadaf Altaf
Aga Khan University Stadium Road Karachi Pakistan
ORCID ID: 0000-0003-0826-1224
Banafsha Ali
Institute of Professional Psychology, Bahria University Karachi Campus
ORCID ID: 0000-0002-7175-8244
[Maryam B, Saed T, Altaf S, et al. Comparing the Needs of Supportive Care for Families and Patients with Pediatric Cancer: A Perspective of Patients, Caregivers and Oncology Health Professionals
Pak.j.rehabil. 2022; 11(1):118-127]
DOI: 10.36283/pjr.zu.11.1/015
INTRODUCTION
Pediatric cancer incidences are substantially rising around the globe. It is the second-highest primary reason of death among 5-14 years children, and the very common types of pediatric cancer are Acute Lymphoblastic Leukemia (ALL), brain tumors, and Neuroblastoma1. About 13,500 cases of cancer in children are diagnosed each year in the United States with a significant decreased survival rate2. Similarly, according to an estimate around 150,000 new cancer cases are reported yearly, with a 60-80% mortality rate in Pakistan3. The rationale of the study is that as the frequency of occurrence of cancer cases is high therefore the need to identify the essential support and education for both patients and caregivers is extremely important and there is also a lack of significant literature from Pakistan on the topic of research.
Concerning the global burden of pediatric cancer, it has been approximated that 13.7 million new cases will be recorded from 2020 to 2050, while most of the children remain undiagnosed, particularly in low middle income countries4. The prevalence and mortality risk of cancer children are apparently higher in low and middle socioeconomic countries, as 90% of these children belong there4,5. Based on an estimate, 22% childhood cancer patient in Pakistan were found to abandon the treatment, while 11% of patients did not receive any treatment, particularly children with brain tumors6. One of the biggest reason being cost of care which is likely to be unmanageable7. Another major factor resulting in treatment abandonment is absence of overall support system, proper education and counseling program regarding child’s diagnosis and treatment plan.
It is emotionally destructing for families to know their child’s cancer diagnosis. It eventually impacts social, emotional, and financial aspect of life as the caregiving process becomes distressing and requires immense assistance8. Nonetheless, providing educative support regarding disease management, home treatment, medication routine, emergency plan, dealing with psychosocial issues, and creating an inclusive and positive environment for a child is vital to the success of treatment. The healthcare providers are responsible to impart knowledge of caregiving measures among caregivers to eliminate the limitations in the overall treatment of disease. Likewise, delivering a structured education program for caregivers demonstrated to increases the understanding of the disease and lead to improved clinical outcome during first-year cancer treatment9.
The overwhelming liability of cancer on families and children entails greater responsibility of healthcare providers to deliver quality supportive care. Indeed, psychological distress emerging from the new diagnosis becomes a prime barrier in understanding complex knowledge of the illness10. For this purpose, the present aim to highlight the provision of psychosocial and educative support for childhood cancer patients and their families and the extent to which they are vulnerable in seeking appropriate assistance, barriers in the pathway, and different areas of healthcare setting that needs to be uplifted in endorsing parental and patients’ socio-emotional and physical wellbeing.
THEORETICAL FRAMEWORK
The aim of the present study is to explore the educational and psychosocial support for caregivers and newly diagnosed oncology patients.
Figure 1
Theoretical Framework: “Continuum of Education in Pediatric Oncology for Newly Diagnosed Families” (11).
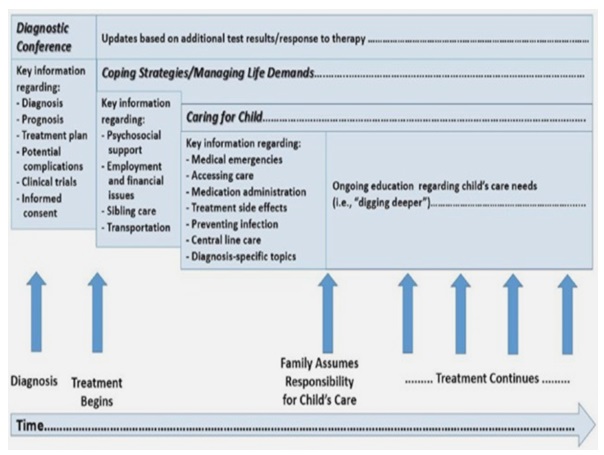
The model “Continuum of Education in Pediatric Oncology for newly Diagnosed Families” is adopted in the study. The framework in Figure 1. clearly depicts that pediatric oncology education is provided on the continuum of care and not just after the initial diagnosis. Throughout the cancer treatment, family and patient are to be provided with psychosocial support corresponding to their needs and financial facilitation. The constant modification in knowledge and associated support is indispensable to assist enhance their coping skills and reduction in overall stress.
METHOD
Study Design
A qualitative exploratory study was conducted to examine the educational and psychological support for families and patients with newly diagnosed pediatric cancers. Medical records, including written and online teaching materials and hospital policies and procedures, were reviewed.
Study Setting
The study was conducted in a private tertiary care hospital in Karachi, Pakistan. Primarily, the research setting was the Pediatric Oncology ward. This private hospital has a separate oncology service line, including Adult and Pediatric daycare oncology setup, inpatient and outpatient services.
Sampling technique
The study subjects of patients were enlisted from the admission and medical records at the hospital and healthcare professionals were selected from oncology department via purposive sampling technique.
Sample size consideration
A total of ten subjects were selected from the hospital. There were four parents, three patients aged 12-18 years, and three health care professionals, including one doctor, nurse, and nurse manager of the oncology department.
Inclusion Criteria
All parents, family members, and children age (12-18 years) with newly diagnosed cancer and receiving treatment were eligible for the study. All the family members and their children with the diagnosis of cancer within two months were included in the study. Besides, healthcare staff of the oncology department also participated in the study.
Exclusion criteria
Children with mental disability caused by the disease were excluded. Newly diagnosed children without any treatment were also excluded.
Data Collection Technique
A total of ten interviews were directed using a semi-structured interview guide, developed with a thorough literature review and employing the “Continuum of education in pediatric oncology for newly diagnosed families” framework11. Further, the data was collected once through telephonic interview due to the Covid-19. Particularly, four in-depth interviews were from parents and three from children aged 12 to 18 years. The rest of the two in-depth interviews were from pediatric oncology Nurse and doctor, and one interview with Oncology Nursing Manager.
Data Analysis
The data was analyzed through the qualitative content analysis method. Data collected from interviews were audio-recorded after taking consent. All the audio-recorded data was transcribed manually after rigorous listening. Afterward, manual coding was prepared for each interview, with software NVIVO 11 as well as manual method was used for the ideas, concepts, and phrases. Then, all the codes were combined, and interrelated codes were grouped. Subsequently, categories were constructed. Finally, all categories were transformed as themes arising from the information.
Ethical Consideration: The study was conducted after Department review committee and the Hospital Ethics Review Committee approval and the registration number for ERC was 2020-2085. The privacy and confidentiality were sustained by conducting telephonic interviews from an uninterrupted setting, the manual and electronic data was protected at all stages of the study by password protection and lock and key system.
Rigor12
criteria of Trustworthiness including credibility, dependability, confirmability and transferability was used to maintain study rigor Credibility was ensured by extensive and continuous literature review and triangulation of data and results by relevant policies and available resources. Conformability was achieved by checking and rechecking data several times and attaining feedback from supervisor throughout the study Dependability of data analysis was thoroughly checked by doing (manually and on Software) Transferability was ensured by explaining the context of the study properly.
RESULTS
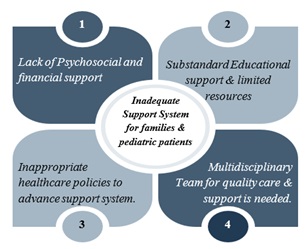
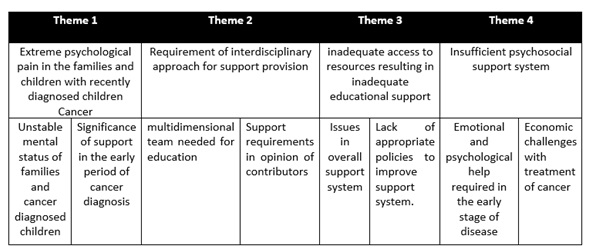
The results gathered from a total of 10 one-on-one consists of four themes, eight categories shown in table 2 and several codes from the data. The summary of the findings is also depicted in figure 2.
Theme 1: Extreme psychological pain in the families and children with recently diagnosed children Cancer
Table 1. Categories Under Four Themes
Category 1: Unstable mental status of families and cancer diagnosed children
The views of health care professionals about mental distress in pediatric cancers were as follow:
“Psychological state of patients and parents during the initial stage is highly sensitive as it is a very shocking news for both”.
According to all the health care professionals, cancer diagnosis is significantly stressful for parents and children. At most, when parents and children were informed that the child is diagnosed with cancer, they get extremely stressed out, depressed, and unable to understand the cause.
Category 2: Significance of support in the early period of cancer diagnosis
Some advice from the doctor was:
“Assuming that only one educative session will be enough to help parents and patient understand their condition would be inappropriate.”
Every parent has different understanding which are influenced by multiple factors such as language barrier and literacy level.
It was found that proper evaluation of needs and delivering requisite information is crucial for the effective process and outcome.
Theme 2: Requirement of interdisciplinary approach for support provision
Category 1: multidimensional team needed for education
The nurse manager claimed: “Those involved in teaching are doctors, nurses and other health care staff like technicians, midwifes and health care attendants”.
Further, the nurse manager mentioned that nutritionist and physiotherapist are also actively involved in teaching.
It suggests that the role of therapist in multidisciplinary team is imperative to assist young children to cope with the treatment stress. They intend to engage these children in different playful and intriguing activities to divert their mind towards positivity.
Category 2: Support requirements in opinion of contributors
The nursing staff expressed: “there should be session, either weekly or monthly, for parents and patients related to disease, diet, and care so that, parents receive adequate teachings and guidance.”
The staff mentioned the need of support in form of sessions and families mentioned support need with the change in patient condition with treatment.
Theme 3: inadequate access to resources resulting in inadequate educational support
Category 1: Issues in overall support system
The oncology fellow stated that “Yes, we have written material available in the ward. But I really feel that it should be more elaborated because every family dynamic is different. My suggestion is that we should have special psychological support and a separate counselor who can assist the patient and the family”.
As suggested by the nurse, the cancer diagnosis equally affects parents and their children. So, psychological support is mandatory for them to handle the stressful situation.
Aside from individual sessions, collective sessions significantly lack in hospital setting. The less usage of appropriate resources such as educational material, motivational videos, support groups, online content, and various application impedes their coping skills as mentioned by manager and staff.
Category 2: Lack of appropriate policies to improve support system.
A nurse mentioned: “In oncology department, pamphlets related to diet plan, preventing infection are missing”.
Also, there was lack of brochures in multiple languages for adequate education as the resources were reviewed.
According to a nurse manager: “I think we need to establish standardized procedures at different national hospitals, specifically conducting counseling sessions.”
Oncology fellow advocated those policies linked with counselling for handling psychological issues is significantly missing along with their inability to reach out to health care professionals during emergency.
Theme 4: Insufficient psychosocial support system
Category 1: Emotional and psychological help required in the early stage of disease
The doctor claimed: “The Doctors and the staff provide social and emotional support to the families”.
A nurse stated, “We provide psychological support as the patients come regularly to the hospital and staff continuously interact with them. This creates a positive relationship among us.
Category 2: Economic challenges with treatment of cancer
The doctor mentioned: “we as care providers provide them with solutions or sometimes help them to sort out their financial issues, and hospital provides financial support for families that are in need.”
Verily, the patients’ family consult doctor and medical staff for financial support, whereby they help by guiding them to available resources. Especially, they discuss about hospital’s welfare system which helps in financial problems.
A specific percentage of welfare is fixed for financial aid. However, families are not very satisfied by the help that further worsen their stress.
DISCUSSION
The present study aims to explore the educational and psychosocial support for pediatric cancer patients and their families by examining their symptomatic verbalization and expression of stressful feelings and need for supportive care. The results depict four major themes that are: experience of stressful feelingsy patients of pediatric cancer and their families, necessity of multidisciplinary team for support provision, limited access to resources leading to inadequate educational support, and insufficient psychosocial support system.
The study reflects that cancer diagnosis lead to stressful outcome for cancer patients and their families. Almost all study subjects denoted that cancer led to excessive worries, sudden shock, panic, and indecision. It has been highlighted that child with newly diagnosed cancer manifest adjustment issues with higher internalizing symptoms, while care providers also present symptoms like depression and anxiety during the first year of their child’s treatment. However, such psychological disturbance tends to decline with time1,13.
This study pertains that the children who can understand their current disease and its severity demonstrated more distress and anxiety as compared to younger children. One of the study implies that parents of children with cancer are at higher risk of post-traumatic stress disorder, especially mothers when told about their child’s diagnosis14.
However, the current study also shows that educational support during initial period of diagnosis and treatment is imperative to build greater understanding of childhood cancer and its related factors. The language barrier and unavailability of translators hinders the procedures of education as well. Consistently, literature infers that since new diagnosis and coexisting treatment is distressing for both children and caregivers, educating them is an essential process to eliminate any irrational thoughts15.
The result shows that within the study setting, nurses, doctors, midwives, technicians, play therapists, nutritionist and physiotherapist were present at the hospital site for treatment. Nonetheless, the oncology team was lacking a psychologist to assist and educate patients and their families related to any psychological concerns. It is crucial to provide psychological support to decrease the vulnerability of patients towards mental health concerns and endorse the caregivers to perform optimal and respond to the stress with relevant coping mechanism.
Another finding suggests that the materials require for the education such as brochures, pamphlet, and printed resources of common side effects of chemotherapy and infection prevention is unavailable. The lack of social support groups, videos, inclusive sessions, and mobile apps for cancer children are inadequate. A study indicates that cancer caregivers who increasingly use online social platform to share health-related experiences have shown enhanced awareness and knowledge, provide recommendation, and stimulate social support system16.
Besides, it was identified that the hospital policies were limited to education only during patients’ stay and when discharged no significant and relevant resources were available to educate them properly as family’s needs are different from one another. To cater such issues educational and vocational support17, building rapport with parents and patients through education, federal and state health policies to avoid conflict, maximizing effective health-related communication, and implementing those policies at hospital setting and examining its efficacy to make necessary revisions is essential18.
In addition, the study recognized counseling, forming support groups, mind diversion treatment and play treatment as crucial constituents of psychosocial help. Though, such services are either limited or missing in the hospital setting.
It has been implied that financial liability caused by the cancer treatment greatly affect their mental health and quality of life19. In that case, health administrations are required to impart greater knowledge of the treatment process yet providing them with adequate facilitation so they can manage their budget and financial difficulties.
With greater exposure to supportive environment in pediatric department, patients and their family can resolve their issues and provide intensive care to their children. Similarly, provision of need-based education, formulating elaborative teaching resources, highlighting psychosocial components, developing institutional guidelines, policy for the inclusion of psychologist as a regular team member, and standardized counseling programs for them can be implicate to address the issues found in the study. Future research should focus on conducting more qualitative studies related to education needs, importance of psychosocial support in pediatric oncology, and significance of written resources for family education at different tertiary care hospital and making comparison, which can help in developing standardized process of oncology support system.
CONCLUSION
Pediatric cancer is a manifestation of great emotional stress with long-term treatment and management commitment. The complexity of the disease and the factors associated to the lack of pediatric cancer support, treatment finances, and appropriate healthcare plan for children makes patients and families anxious and psychologically disturbed. The initial phase of cancer diagnosis is most challenging, where need of support is prominent. The study identified the requirement of special support and care to families and patients with suitable resources, professional psychological assistance, engagement of multiple stakeholders to handle complex medical, psychosocial, and financial issues, and appropriate cancer-related policies to expedite their functioning during early stage of diagnosis.
REFERENCES
- Toledano-Toledano F, Luna D, Moral de la Rubia J, Martínez Valverde S, Bermúdez Morón CA, Salazar García M, et al. Psychosocial Factors Predicting Resilience in Family Caregivers of Children with Cancer: A Cross-Sectional Study. International Journal of Environmental Research and Public Health. 2021;18(2):748.
- Group CsO. Children’s Oncology Group: The world’s childhood cancer experts. What is Cancer? ; 2018.
- Yusuf A. Cancer care in Pakistan. Japanese journal of clinical oncology. 2013;43(8):771-5.
- Atun R, Bhakta N, Denburg A, Frazier AL, Friedrich P, Gupta S, et al. Sustainable care for children with cancer: a Lancet Oncology Commission. The Lancet Oncology. 2020;21(4):e185-e224.
- Bhakta N, Force LM, Allemani C, Atun R, Bray F, Coleman MP, et al. Childhood cancer burden: a review of global estimates. The lancet oncology. 2019;20(1):e42-e53.
- Siddiqui DeF, Ashraf MS, Iftikhar S, Belgaumi AF. Predictors of treatment abandonment for patients with pediatric cancer at Indus Children Cancer Hospital, Karachi, Pakistan. Pediatric blood & cancer. 2018;65(2):e26818.
- Zaidi AA, Ansari TZ, Khan A. The financial burden of cancer: estimates from patients undergoing cancer care in a tertiary care hospital. International journal for equity in health. 2012;11(1):1-6.
- Teixeira RJ, Remondes‐Costa S, Graça Pereira M, Brandão T. The impact of informal cancer caregiving: A literature review on psychophysiological studies. European journal of cancer care. 2019;28(4):e13042.
- De la Maza V, Manriquez M, Castro M, Viveros P, Fernandez M, Vogel E, et al. Impact of a structured educational programme for caregivers of children with cancer on parental knowledge of the disease and paediatric clinical outcomes during the first year of treatment. European Journal of Cancer Care. 2020;29(6):e13294.
- Wilson Smith MG, Sachse K, Perry MT. Road to Home Program: a performance improvement initiative to increase family and nurse satisfaction with the discharge education process for newly diagnosed pediatric oncology patients. Journal of Pediatric Oncology Nursing. 2018;35(5):368-74.
- Landier W, Ahern J, Barakat LP, Bhatia S, Bingen KM, Bondurant PG, et al. Patient/family education for newly diagnosed pediatric oncology patients: Consensus recommendations from a Children’s Oncology Group expert panel. Journal of Pediatric Oncology Nursing. 2016;33(6):422-31.
- Lincoln YS, Guba EA. Naturalist inquiry. Beverly Hills, CA1985.
- Katz LF, Fladeboe K, King K, Gurtovenko K, Kawamura J, Friedman D, et al. Trajectories of child and caregiver psychological adjustment in families of children with cancer. Health Psychology. 2018;37(8):725.
- Masa’deh R, Jarrah S. Post traumatic stress disorder in parents of children with cancer in Jordan. Archives of psychiatric nursing. 2017;31(1):8-12.
- Gunter MD, Duke G. Reducing uncertainty in families dealing with childhood cancers: An integrative literature review. 2018.
- Gage-Bouchard EA, LaValley S, Mollica M, Beaupin LK. Cancer communication on social media: examining how cancer caregivers use Facebook for cancer-related communication. Cancer nursing. 2017;40(4):332-8.
- Fardell JE, Wakefield CE, Patterson P, Lum A, Cohn RJ, Pini SA, et al. Narrative review of the educational, vocational, and financial needs of adolescents and young adults with cancer: recommendations for support and research. Journal of adolescent and young adult oncology. 2018;7(2):143-7.
- Dev DA, Byrd-Williams C, Ramsay S, McBride B, Srivastava D, Murriel A, et al. Engaging parents to promote children’s nutrition and health: providers’ barriers and strategies in head start and child care centers. American Journal of Health Promotion. 2017;31(2):153-62.
- Santacroce SJ, Kneipp SM. Influence of pediatric cancer–related financial burden on parent distress and other stress‐related symptoms. Pediatric blood & cancer. 2020;67(3):e28093.
- Van Schoors M, Caes L, Knoble NB, Goubert L, Verhofstadt LL, Alderfer MA. Systematic review: Associations between family functioning and child adjustment after pediatric cancer diagnosis: A meta-analysis. Journal of pediatric psychology. 2017 Jan 1;42(1):6-18.
- Wolf KM. The Transition from Health to Illness: Best Practices For Education of Parents with Children Newly Diagnosed with Cancer.
- Tang WP, Chan CW, Leung DY, Chan DN. The effects of psychoeducational interventions on caregivers of children with cancer: A meta-analysis of randomized controlled trials. Journal of Child Health Care. 2020 Mar;24(1):123-42.
- Pierce L, Hocking MC, Schwartz LA, Alderfer MA, Kazak AE, Barakat LP. Caregiver distress and patient health‐related quality of life: psychosocial screening during pediatric cancer treatment. Psycho‐oncology. 2017 Oct;26(10):1555-61.
- McCarthy MC, McNeil R, Drew S, Orme L, Sawyer SM. Information needs of adolescent and young adult cancer patients and their parent-carers. Supportive Care in Cancer. 2018 May;26(5):1655-64.
- Haugen MS, Landier W, Mandrell BN, Sullivan J, Schwartz C, Skeens MA, Hockenberry M. Educating families of children newly diagnosed with cancer: Insights of a Delphi panel of expert clinicians from the Children’s Oncology Group. Journal of Pediatric Oncology Nursing. 2016 Nov;33(6):405-13
