ABSTRACT
OBJECTIVE
To find out adhesive capsulitis patients in diabetes mellitus patients.
STUDY DESIGN
Cross-sectional study.
STUDY SETTINGS & PARTICIPANTS
Patients with diabetes mellitus from Ziauddin university hospital Clifton Karachi were included. 325 diabetic patients in which 81 patients were diagnosed with adhesive capsulitis.
SAMPLE SIZE
A Sample size of 325 patients was selected.
SUBJECTS
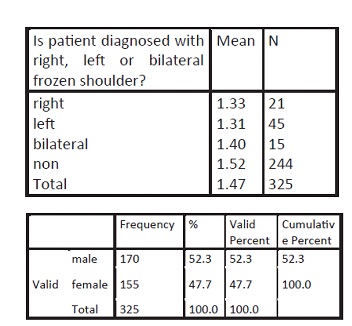
170 men and 155 women aged between 40 to 79 years were selected.
RESULT
Frequency of shoulder adhesive capsulitis was 24.9% among diabetic subjects.
CONCLUSION
Adhesive capsulitis are under recognized in adult diabetic patients occurring in 18% of the cases. Physicians should consider examining the periarticular region of the joints in the hands and shoulders whenever a diabetic patient presents with musculoskeletal symptoms.
Key Words
Diabetes Mellitus Manifestations, Adhesive Capsulitis, Frequency, Pain, Stiffness.
Shakeel Ahmad
Senior Physiotherapist
Department of Physiotherapy
Ziauddin Hospital
Dr. Mohammad Sohail Rafi
Assistant Professor
Orthopedic and Spinal Surgery
Ziauddin Hospital
Iqbal Ahmed Siddiqui
Incharge
Department of Physiotherapy
Ziauddin Hospital
Khurram Hamidi
Assistant Manager
Department of Physiotherapy
Ziauddin Hospital
Nabiha Mujahid Faruq
Senior Physiotherapist
Department of Physiotherapy
Ziauddin Hospital
[Ahmad S, Rafi MS, Siddiqui IA, Hamidi K, Faruq NM. The Frequency of Adhesive Capsulitis in Diabetes Mellitus Patients. Pak. j. rehabil. 2012;1(2):33-37]
INTRODUCTION
Adhesive capsulitis, or frozen shoulder, has been reported round about 20% of diabetic patients. This term refers to a stiffened shoulder joint usually caused by thickening and contraction of the capsule which results in a substantial decrease in capsular volume capacity. Patients complain shoulder stiffness with decreased ROM and pain though the pain of this conditions in diabetic patient is usually less than that of the general population.
Adhesive capsulitis, frozen shoulder, shoulder periarthritis, or alliterative bursitis is the most disabling of the common musculoskeletal problems. There is gradual limitation of shoulder movement, especially lateral rotation and abduction. The thickened joint capsule is closely applied and adherent to the humerus head, due to which there is too much limitation in range of motion of shoulder joint. The exact origins of adhesive capsulitis are not determined but still it has been related with several other conditions, such as trauma to shoulder, other conditions such as respiratory and cerebral. Usually, adhesive capsulitis have three distinct phases: painful, adhesive, and resolution phases. Adhesive capsulitis appears at a younger age in patients with diabetes and is usually less painful, although it responds less well to treatment and lasts longer1.
The estimated prevalence is 11–30% in diabetic patients and 2–10% in nondiabetics8–11. Adhesive capsulitis is associated with the duration of diabetes and age1. A higher prevalence of frozen shoulder (20–29%) has been reported in diabetes mellitus (DM) patients. However, the outcome of these patients has only been studied previously in Western countries. None have been documented in Asia. Adhesive capsulitis of the shoulder (frozen shoulder) is characterized by a gradual increase in pain and stiffness. This condition has three stages lasting up to one to three years and does not recur in the same shoulder. The etiology of frozen shoulder is yet to be discovered and excellent results of manipulation under anesthesia (MUA) have been reported by many authors but few have focused on patients with DM. Hence, in this study, we compared the objective improvement in range of motion and the subjective improvement in function after MUA in patients with and without non-insulin dependent DM2.
The estimated prevalence of adhesive capsulitis (AC) is 11%–30% in diabetes; they are considerably greater than those have no diabetes. AC has been associated with the duration of diabetes and age with diabetics experiencing significantly greater pain and dysfunction3.
DM is considered as an epidemic in the modern world and much of its morbidity and mortality is related to micro and macro vascular problems or disorder. It is also linked with other disorders of the hand and shoulder that can be very incapacitating and significantly compromise their quality of life 12, 13. Musculoskeletal (MSK) complications of DM are the most common endocrine disorder. These have been usually poorly recognized and poorly treated compared with other conditions, such as neuropathy, retinopathy, and nephropathy. These are, some of the etiology of disability, involve not only the joints, but also the bones and other tissues. An Interview Survey was done in 2004 by national health survey and they determined that 58% of diabetic patients would have functional disability. The percentage of diabetic patients with functional disability will increase as diabetic patients ‘number increases, and therefore makes a great burden on common health problem. Current studies show that the prevalence of MSK manifestations in the hands and shoulders in patients with type 1 or type 2 diabetes is 30%. These manifestations are closely linked to age prolonged disease duration and vascular complications in the form of retinopathy4.
The decreased ROM is worst in abduction and lateral rotation. Medial rotation is affected least. It seems to be twice as common in diabetic patients. Therapy is largely conservative and minimizing progress of the adhesions mobilization of the shoulder which include gentle stretching and range of motion exercises, and the use of analgesics and/ or intra-particular injections7. The relation between DM and AC has been shown in previous few studies. Bridgman reviewed the medical records of 800 diabetic subjects and found evidence of per arthritis in 10.8%, compared with 2.3% in a control group of 600 non-diabetic subjects4. Pal et al found shoulder capsulitis in 20.4% of insulin dependent and in 18.3% of non-insulin dependent diabetes patients and in 5.3% of normal subjects5. In a study of 824 type II diabetic and 320 control subjects shoulder capsulitis was observed in 31.8% and 10.3% of subjects, respectively6. Bilateral involvement of shoulder capsulitis was more common in diabetic (10%) than in the control subjects (3%). 16 Diabetic shoulder capsulitis seems to appear at a younger age, may be less painful, responds less well to treatment, and lasts longer than non-diabetic shoulder capsulitis6. A high frequency of other hand syndromes, such as limited joint mobility, has been found among diabetic patients with shoulder capsulitis. The association between limited joint mobility and micro vascular complications of diabetes has been well documented, but there are also two studies showing an association between shoulder capsulitis and retinopathy. However, no association between shoulder capsulitis and diabetic neuropathy has been found. The purpose of this study was to investigate the prevalence of shoulder capsulitis and its association to the diabetic complications in diabetic subjects. (10) Adhesive capsulitis has an incidence of 3–5% in the general population and up to 20% in those with DM. This is one of the most common MSK disorder seen in orthopedics. Though some practitioners suggest AC as a self-limiting disorder that resolves in 1–3 years, other studies report ranges of between 20 and 50% of patients with adhesive caspulitis which suffer long-term ROM deficits that may last up to 10 years. The typical patient that develops adhesive capsulitis is a female in her 5th to 7th decade of life. There is generally no preference for handedness and adhesive capsulitis rarely occurs simultaneously bilaterally however, others have reported that it can occur sequentially bilaterally in up to 40–50% of patients. Adhesive capsulitis is commonly associated with other systemic and non-systemic conditions. By far the most common is the co-morbid condition of diabetes mellitus, with an incidence of 10–36 %8.
MATERIAL AND METHOD
This was an observational study in which diabetic patients coming to clinic for their routine checkup were enrolled along with age and gender matched controls. Data was analyzed on SPSS 20. Demographic data regarding the age, sex, type and duration of diabetes was noted. The inclusion criteria for subjects were symptomatic shoulder problems with diabetes mellitus in age between 40 to 79. The exclusion criteria were; (1) any neurological conditions affecting shoulder. (2) Any pathology other than AC. (3) any Surgery of head, neck or upper limb.
After the diabetic history of subjects was confirmed from the medical chart, patients were examined and assessed for pain and restriction of range of motion in their shoulder. Elderly diabetic subjects with pain and/or restriction of range of motion were referred to the orthopedic surgeon for diagnosis. Pain of the patient was recorded using the visual analogue scale (VAS). 170 men and 155 women aged between 40 to 79 years were selected. Prevalence of shoulder Adhesive capsulitis was 24.9% in diabetic subjects. We included 325 diabetic patients in which 81 patients were diagnosed with adhesive capsulitis.
Patients who were diagnosed with adhesive Capsulitis
STATISTICAL ANALYSIS AND RESULT
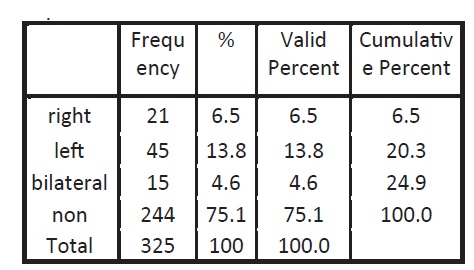
Total 325 diabetic patients were recruited in this study. In the diabetic group, there were 170 males (52.3%) and 155 females (47.7S %). The prevalence of adhesive capsulitits in different age groups, according diagnosis gender right and left shoulder was calculated. Prevalence of shoulder Adhesive capsulitis was 24.9% in diabetic subjects.
Patient diagnosed with right, left or bilateral frozen shoulder
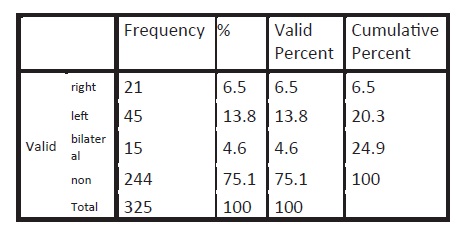
We included 325 diabetic patients in which 81 patients were diagnosed with adhesive capsulitis. Twenty one (21) patients were having right, forty five (45) were left and fifteen (15) were having bilateral involment. As prevalence in international study=30% and n=z2 p (1-p)/d2 at 95% confidence of interval z=1.96-95% n=3.8416 (0.3) (1-0.3)/ (0.05)2. n=325 325 subjects had 177 males (52.3%) and 155 females (47.7%) only 81% patients (24.9%) had adhesive capsulitis (2.96%) with shoulder abnormality. Shoulder abnormalities were more frequent than hand abnormalities with capsulitis affecting 23 (10.9%) and tendonitis 20(9.5%) diabetic patients. When the frequency of frozen shoulder was identified, it is noted that although diabetic patients have a high frequency of adhesive capsulitis compared to nondiabetic.
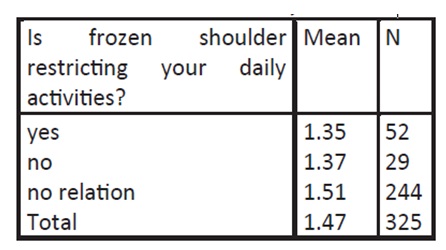
Mean of patients whose frozen shoulder restrict their daily activities
Patient diagnosed with right, left or bilateral frozen shoulder
DISCUSSION
Musculoskeletal disorders of the hand and shoulder occur more commonly in diabetic patients. In our study, these syndromes were about 4 times more frequent in diabetic than nondiabetic patients. While we did not assess the presence of diabetic cheiropathy, (diabetes specific changes) we observed increased rates of adhesive capsulitis of the shoulder.
Our study showed three important findings. First, the frequency of adhesive capsulitis in DM was 24.9%. Adhesive capsulitis is a chronic disabling condition associated with pain, which require long-term management in the form of physiotherapy and repeated injections. Unfortunately, the treatment is more prolonged in DM patients, and surgery may be required if the condition is not
treated early14. There is strong evidence that the development of one complication predisposes to the development of another. An important relation was found between AC and other musculoskeletal disorder of diabetes, which is more in carpal tunnel syndrome, tenosynovitis, and decrease joint mobility. A Japanese group assessed 302 DM patients in a case control study and established a significant relation between different types of complications, especially tenosynovitis and limited joint mobility15.
In this study, we have observed a significant relation of shoulder involvement with Type 2 DM. We found a weak but positive relationship between advancing age and duration of diabetes with upper limb musculoskeletal abnormalities in our diabetic subjects in accordance with international data13. No relation was proved between upper limb MSK abnormalities and degree increase glycemia. However, considering the complications of diabetes, presence of any one of these was only established with CTS and/or adhesive capsulitis. This is an interesting observation since many studies found a strong correlation between these variables while it is refuted by others9.
A study done in US confirmed the incidence of adhesive capsulitis being two to four times higher in diabetics than in the general population and the prevalence of diabetes in patients with adhesive capsulitis was shown at 38.6%. Cagliero in his study identified a frequency of 12% capsulitis in diabetic patients and although the duration of diabetes was shorter in our study, it is comparable to our study with a frequency of 11%. Both studies showed a predisposition of rheumatic complications in the female sex. Other studies done in UK, Australia and India show much higher frequencies of capsulitis ranging between 23–30%10,23.
Musculoskeletal disorders are common in type 1 and 2 diabetic subjects, and examination of shoulders as well as the skeleton, should be included in the evaluation of patients with DM 20,21. Most musculoskeletal complications seem to be associated with the duration of DM and appear in diabetic patients of younger age than their counterparts in the general population 22,25. Musculoskeletal disorders in these patients are probably related to the long-term glycogenic control of diabetes. There was no direct relation could be proven with the metabolic control of the disease18. Shoulder capsulitis is common in type 1 and type 2 diabetic patients. It is associated with age in type 1 and 2 diabetic patients and with the duration of diabetes in type 1 patients. Noninsulin dependent diabetics also have an increased incidence of frozen shoulder, but not as those use insulins. All patients were type 2 diabetics and hence cannot compare. 42% prevalence was noted in female diabetic patients. Several authors have confirmed increased prevalence of diabetic AC in females. There should be regular physical therapy treatment programme19. Adhesive capsulitis are present in about 24.9% of diabetic patients though not commonly recognized as a complication of DM. Often patient presentation is delay, and sometime this late information may create other problem. Usually there is no trauma with the gradual progression of pain and decrease range of motion. The key point is loss of both passive and active ROM without degeneration on X-ray. A combination treatment is commonly helpful for the patient afflicted with frozen shoulder such as drug therapy and surgical intervention. Other factors such as comorbid factors can have a great act in length and amount of recovery. It is recommended that diabetic patients should always be screened for the presence of rheumatic complications since early recognition lessens the chances of non-reversible damage24. Regular physical therapy program must be the cornerstone of diabetic management along with diet and pharmacotherapy.
CONCLUSION
This is highly recommended that diabetes patients should always be screened for the presence of rheumatic complications since early recognition lessens the chances of irreversible damage.
REFERENCE
- Smith L, Burnet SP, McNe JD. Musculoskeletal manifestations of diabetes mellitus. Br J Sports Med 2003;37:30–35
- JP, Huang TF, Hsiao-Li Ma, Hung S, Chen TS, and CL Liu. Manipulation under anesthesia for frozen shoulder in patients with and without non-insulin dependent diabetes mellitus, Published online 2010;34(8):1227-32.
- Gupta S, Raja K, Manikandan N. Impact of adhesive capsulitis on quality of life in elderly subjects with diabetes: A cross sectional study. Int J Diabetes Dev Ctries 2008;28(4):125-9
- Atta MS. Musculoskeletal manifestations in diabetic patients at a tertiary center. Libyan J Med 2012;7
- Wyatt LH, Ferrance RJ. The musculoskeletal effects of diabetes mellitus. 2006;50(1)43-50.
- International Diabetic Federation Diabetes [online] 2006 [cited 2010 July 18]
- Ramchurn N, Mashamba C, Leitch E, Arutchelvam V, Narayanan K, Weaver J, et al: Upper limb musculoskeletal abnormalities and poor metabolic control in diabetes. Eur J Intern Med. 2009;20(7):718-21
- Kidwai SS, Wahid L, Siddiqi SA, Khan RM, Ghauri I, Sheikh I. Upper limb musculoskeletal abnormalities in type 2 diabetic patients in low socioeconomic strata in Pakistan, BMC Res Notes 2012;6:16
- Manske RC , Prohaska D, Diagnosis and management of adhesive capsulitis, Curr Rev Musculoskeletal Med 2008;1:180-9
- Arkkila PET, Kantola IM, Viikari JSA, Ronnemaa T. Shoulder capsulitis in type I and II diabetic patients: association with diabetic complications and related diseases. Ann Rheum Dis 1996;55:907-14
- Qidwai W, Ashfaq T: Imminent Epidemic of Diabetes Mellitus in Pakistan: Issues and challenges for Health Care Providers. JLUMHS 2010;9:112
- Schiavon F, Circhetta C, Dani L: The diabetic hand. Reumatismo 2004;56:139–42
- Gamstedt A, Holm-Glad J, Ohlson CG, Sundstrom M. Hand abnormalities are strongly associated with the duration of diabetes mellitus. J Intern Med 1993;234(2):189-93
- International Diabetes Federation: Diabetes Atlas. 3rd edition. Brussels, Belgium: International Diabetes Federation 2006;23(5)
- Thomas SJ, McDougall C, Brown ID, et al. Prevalence of symptoms and signs of shoulder problems in people with diabetes mellitus. J Shoulder Elbow Surg 2007;16:748–51.
- International Diabetic Federation Diabetes [online] 2006 [cited 2010 July 18]
- Arkkila PE, Gautier JF: Musculoskeletal disorders in diabetes mellitus: an Update. Best Pract Res Clin Rheumatol 2003;17:945–70
- Douloumpakas I, Pyrpasopoulou A, Triantafyllou A, Sampanis CH, Aslanidis S. Prevalence of musculoskeletal disorders in patients with type 2 diabetes mellitus: a pilot study, Hippokratia 2007;11(4):216-18
- Harrington JM, Carter JT, Birrell L, Gompertz D: Surveillance case definitions for work related upper limb pain syndromes. Occur Environ Med 1998;55:264-71
- Aydeniz A, Gursoy S, Guney E. Which musculoskeletal manifestation is most seen in type 2 diabetics? J Int Med Res 2008;36(3):505-11
- Cagliero E, Apruzzese W, Perlmutter GS, Nathan DM. Musculoskeletal disorders of the hand and shoulder in patients with diabetes mellitus. Am J Med 2002;112(6):487-90
- Thomas SJ, McDougall C, Brown ID, Jaberoo MC, Stearns A, Ashraf R, et al. Prevalence of symptoms and signs of shoulder problems in people with diabetes mellitus. J Shoulder Elbow Surg 2007;16(6):748–51
- Crispin J, Alcocer-Varela J. Rheumatologic manifestations of diabetes mellitus Am J Med. 2003;114(9):753–57
- Kim RP, Edelman SV, Kim DD. Musculoskeletal complications of diabetes mellitus. Clinical Diabetes 2001;19(3):132-35
- Tighe CB, Oakley WS Jr. The prevalence of a diabetic condition and adhesive capsulitis of the shoulder. South Med J 2008;101(6):591-95
