Hafiza Javeria1*, Danish Rasool2, Dr. Ucksy Mallick3
1*Senior Lecturer, ZCRS, Ziauddin University, Karachi, Pakistan![]()
2Assistant Professor, ZCRS, Ziauddin University, Karachi, Pakistan![]()
3Ashfaq Memorial Hospital, Karachi, Pakistan![]()
Abstract
Objective: This systematic review and meta-analysis was conducted to determine the impact of IASTM on musculoskeletal soft tissue injuries.
Materials and Methods: In order to find terms like “instrument,” “assisted,” “soft tissue dysfunction AND wrist, back, elbow, knee, ankle and foot”, “interventions AND IASTM,” studies from conception to December 2021 were systematically analyzed across seven electronic databases: Medline, PubMed, Cochrane Library, Google Scholar, Scopus, PEDro, and Web of Science. The inclusion criteria for the systematic review were thus met by (n=14) randomized controlled studies.
Results: IASTM treatments are associated with both short and long-term pain reduction and improved functioning. IASTM was discovered to have a short-term favorable effect on the functioning of patients with soft tissue injuries.
Conclusion: It was established that IASTM had a short-term positive impact on the functionality of individuals with soft tissue injuries in different body regions. Future researches should focus on acquiring information about long-term effects using credible evidence.
Keywords: Instrument assisted soft tissue mobilization, soft tissue injuries, pain management, function, myofascial release, range of motion.
Introduction
Soft tissue injuries are a prevalent and major source of morbidity in both the general public and sportsmen1. The bulk of these disorders are caused by muscle-tendon overload, or when ligaments are torn as a result of excessive exercise or improper training practices2. Contusion, sprains, strains, tendinitis, and stress injuries are by far the most prevalent soft injuries among athletes and non-athletes3 while ankle sprains being the most common. In addition to it, Achilles tendon rupture, tendinopathies, plantar fascia and retro-calcaneal bursitis are also prominent causes of ankle discomfort that can lead to subsequent problems4, 5.
Manual therapy comprises a vast range of treatments that may be divided into many major categories, such as manipulation, mobilization, muscle energy techniques etc. Whereas, static stretching and soft tissue mobilization are the two most popular manual therapy techniques used by therapists in the care of acute and chronic ankle and foot soft tissue injuries6. Despite this, several studies have shown joint mobilization and manipulation as an effective treatment for ankle and foot soft tissue injuries along with the PRICE (Protection, Rest, Ice, Compression, and Elevation) strengthening, proprioceptive and functional exercise as an adjunct7,8. Furthermore, American Physical Therapy Association (APTA) is actively developing evidence-based practice guidelines for clinicians dealing with musculoskeletal conditions for operative management9.
According to recent studies, Instrument-Assisted Soft Tissue Mobilization (IASTM) is a new and highly trained myofascial technique that has gained favor in modern decades for treating soft-tissue ailments10. IASTM method involves utilizing an instrument to eradicate scar tissue that has developed in soft tissues and stimulating fibroblasts to help in the healing process. This strategy not only relieves pain but also aids in the application of deep pressure for a bigger effect by covering a broader region11. This allows clinicians to get a more limited and thorough reach of tissues. Furthermore, IASTM may improve patients’ function, and reduce discomfort in the short term after acute and chronic soft tissue injuries12. Moreover, it can also be used to treat non-pathological diseases such as muscle tightness, DOMS (Delayed Onset Muscle Soreness), as it affects flexibility and range of motion13-14. Such advantages might be useful in sports recuperation and athletic training.
IASTM’s popularity has also resulted in a growing corpus of studies on its efficacy15. Higher-level controlled studies have recently been published, with researchers exploring the effects of IASTM on musculoskeletal pathologies16,21. Its exact effects on soft tissue injuries, on the other hand, remain uncertain. This is due to the fact that the conclusions and key outcomes of pertinent research papers have been shown to vary. Despite the fact that numerous studies have examined the advantages of IASTM in treating neck pain as well as other conditions, research on the treatment of soft issue injuries to the ankle and foot has been limited or non-existent. The consequences of combining this method with other tactics are unclear at this time. Taking into mind the aforementioned scientific void, this review investigated the existing studies to determine the impact of IASTM as a skilled intervention to improve soft tissue function and joint ROM after an injury.
Methodology
Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines were followed for conducting this review22.
Search Strategies
The studies were systematically analyzed from their inception until December 2021 using seven electronic databases: MEDLINE, PubMed, Cochrane Library, Google Scholar, Scopus, PEDro, and Web of Science. On the basis of publication dates and language, filters were used. The authors used Medical Subject Headings (MeSH) to locate synonyms for words like “instrument,” “assisted,” “soft-tissue dysfunction AND wrist, back, elbow, knee, ankle and foot,” “interventions AND IASTM,” “IASTM NOT Gua Sha,” and “IASTM NOT ASTYM” in their searches. The terms “Gua Sha” and “ASTYM” were not included in this search. These treatments are similar to IASTM, but they have different administration, and explanations for the treatment, as well as the outcome metrics.
Eligibility Criteria
The effectiveness of IASTM technique for patients with soft tissue injuries in different regions of the body was assessed. To select titles, the abbreviation ‘PICO’ i.e. Patients/Problem, Interventions/Exposure, Comparisons, and Outcomes was employed. Therefore, in patients with soft tissue injuries of the wrist, back, elbow, knee, ankle and foot, the results of IASTM treatments were contrasted with those of other interventions such as rest, ice, cryotherapy, early mobilization, and progressive resistance exercises. Experimental studies that included subjects of any age with clinically determined soft tissue injuries and were published in English after peer review were acceptable. Case reports, case series, clinical comments, dissertations, conference posters, abstracts, and studies that used clinically unsuitable outcome measures for the disease being treated were excluded. Despite the fact that certain therapies may be difficult to comprehend, the review committee determined that the lack of literature justified their inclusion.
Assessment of Risk of Bias
The publications were analyzed to rule out systematic errors using the Cochrane Manual for Systematic Review of Interventions under domains of selection bias, performance bias, detection bias, attrition bias and reporting bias to predict high, low or unknown risks.
Quantitative Analysis
The analysis was carried out using the statistical software named MedCalc-version 18.11.3. The assumptions of heterogeneity and Standardized Mean Difference (SMD) across groups with pooled S.D. were examined using a random effect model with a 95% Confidence Interval. Cohen’s rule of thumb categories was used to classify the effect size as small = 0.2 to 0.5, medium = 0.5 to 0.8, and large = ≥0.8. The degree of study heterogeneity was determined using I2 statistics, with a significant value of p<0.05.
Outcome Measures
Individual functional markers of the ankle joint, such as the patient’s pain perception, range of motion and overall function, were employed as outcome measures for reporting the IASTM treatments’ effectiveness.
Results
The systematic search yielded a total of (n=189) studies, of which (n=139) were chosen after careful consideration of the titles and abstracts’ relevance to the review’s topic. Articles that appeared in multiple search engines were deleted (n=50), while studies that included IASTM as a therapeutic component survived (n=39). Furthermore, (n=20) papers were excluded because only (n=14) publications met the inclusion criteria for the review as shown in (Figure-1).
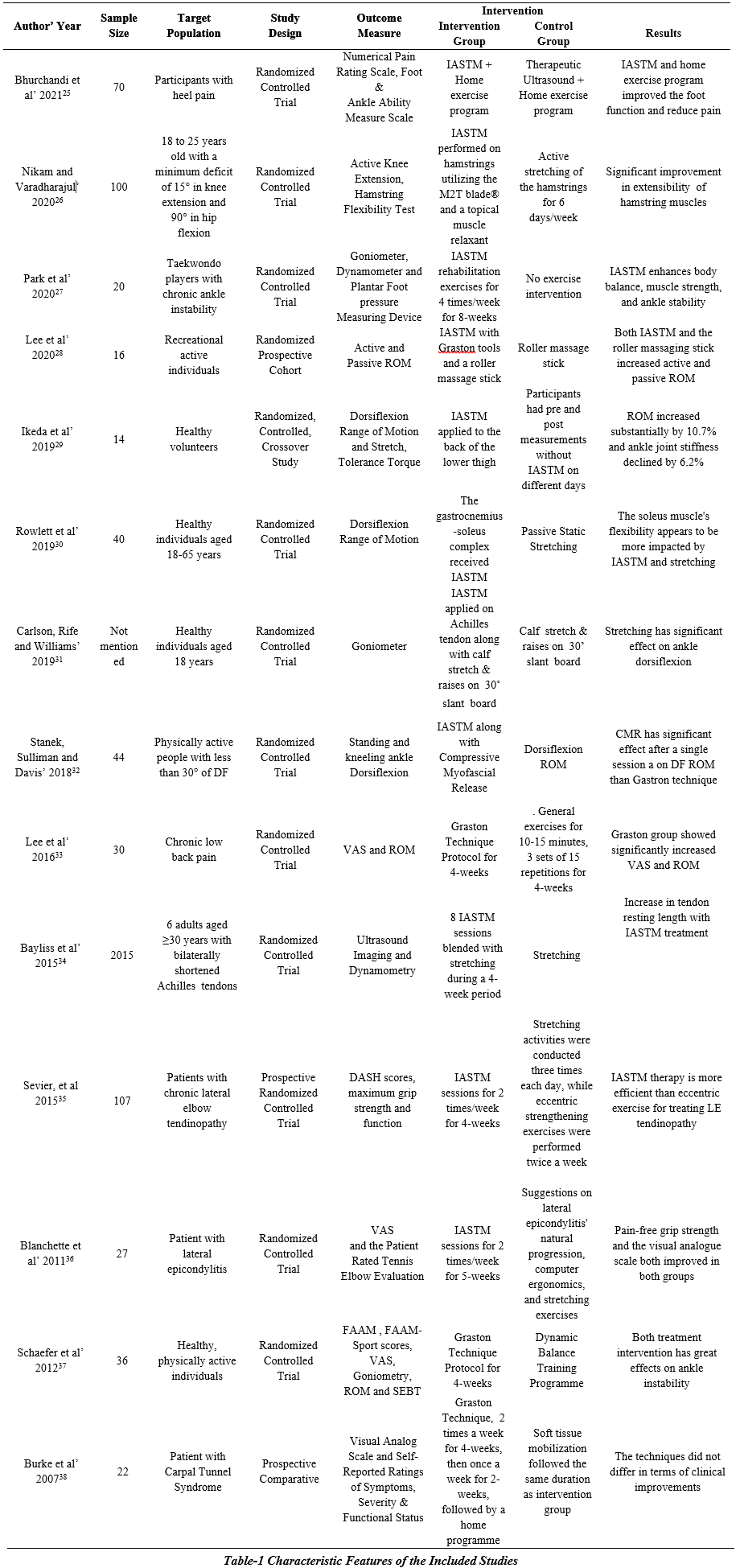
As shown in Table-2, 14 studies employed randomized controlled trials. Participants were divided into the intervention and control groups in practically all of the trials. Despite certain similarities, there are undoubtedly substantial discrepancies that have affected the study’s conclusions. The diagnostic criteria (examination), the outcome evaluation, and the finding that neither arm (intervention or control) produced any differences at baseline were shared by both trials. The FAAM, VAS, and goniometer were usually employed in studies for ROM reasons, with the exception of one study that used the SEBT for balance. The intervention, which lasted between 4 and 8 weeks, had a significant impact. The proportion of women in the studies was much greater than the proportion of males. Furthermore, the number of participants varied between studies. Lastly, in certain studies, the frequency of re-evaluation was low, and some studies did not re-evaluate at all.
Meta-Analysis
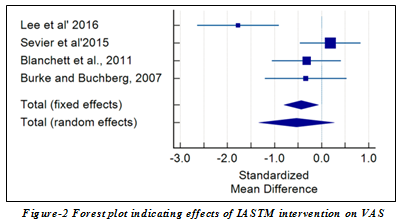
Visual Analog Scale: In (n=8) randomized controlled trials, the IASTM intervention showed a significant reduction in pain. According to the Cohen rule of thumb, the pool effects of IASTM intervention in terms of SMD had an impact of 0.533 in a random effect model (Table-2), indicating that it had a moderate impact on pain relief. Additionally, the forest plot was employed to depict the pool effects in the random effect model at a 95% Confidence Level (Estimation of heterogeneity: Q=13.9576, I2=78.51%) in Figure-2.
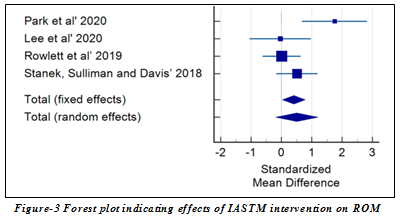
Rom: The pooled effects of IASTM management in (n=8) trials showed a significant improvement in ROM in terms of SMD with an impact of 0.507 in a random effect model which by Cohen’s rule of thumb denotes a moderate effect of IASTM in enhancing ROM (Table-3). The forest plot depicted the pool effects in the random effect model at 95% Confidence Interval (Estimation of heterogeneity: Q=9.5718 and I2=68.66%) in Figure-3.
Synthesized Findings
In cases of ankle and soft tissue injuries, the IASTM has been shown to lessen chronic pain, boost functioning, increase range of motion, and improve gait pattern. Bhurchandi et al.25 demonstrated that IASTM had a short and long-term impact on heel pain. According to Nikam and Varadharajulu26, IASTM utilizing the M2T blade in combination with a topical muscle tissue relaxant like Volteran had much superior outcomes in the muscles of recreational runners. Ikeda et al.29 showed that IASTM effectively decreased ankle joint stiffness and improved dorsiflexion range of motion. Peak passive torque and muscular stiffness, however, remained constant. In repeated evaluations of controls, every factor remained the same. In the study by Rowlett et al.30 one session of IASTM or stretching enhanced ankle dorsiflexion range of motion in WBLT and MRP2. There were no noticeable changes found in MRP1. Improvements in range of motion assessed with the knee flexed suggest that IASTM and stretching tend to have a bigger impact on soleus muscle flexibility. The use of self-stretching to empower patients appeared to be acceptable and beneficial because there were no clinically significant differences between both the intervention groups in weight-bearing circumstances. To increase dorsiflexion range of motion, more research is needed on the advantages of stretching paired with IASTM. The combined impact of tissue flossing and IASTM on ankle dorsiflexion is described by Carlson et al.31 According to the study; IASTM reduces the risk of injury, improves flexibility and range of motion after surgery, and improves leaping mechanics.
Stanek and colleagues32 investigated the dorsiflexion deficits, and compressive myofascial release improved ankle dorsiflexion after just one session. It was suggested that clinicians should investigate CMR as a treatment option for patients with mobility deficits. According to Bayliss et al.34 IASTM appears to be a successful approach for changing the material properties of the shortened, healthy Achilles tendon. More study is needed to establish if the modifications produced have an impact on injury risk in injured tendons. Participants in the 4-week treatment programme of the Dynamic-Balance-Training Program aided with Graston Instrument-Assisted Soft-Tissue Mobilization for chronic ankle instability by Schaefer et al.37 showed improvement in it. IASTM rehabilitation exercises improved ankle joint mobility, isokinetic muscle strength, and balance in individuals with persistent ankle instability, according to Park et al.27 For the VAS and ROM; there was a significant time-by-group interaction. The Graston group’s discomfort decreased considerably after the intervention, according to a post hoc paired t-test. Both groups’ lumbar range of motion improved significantly after the intervention in patient with chronic lower back patients according to Lee et al.33 although the roller massaging stick is less expensive than the IASTM. Lee et al.28 claimed that both the IASTM and the roller massaging stick were similarly useful in hamstring range of motion both immediately and over time. IASTM therapy has been shown to be a successful therapeutic alternative for individuals with lateral epicondylitis tendinopathy, as both a primary treatment and after an eccentric exercise regime has failed, according to Sevier et al’s research35 According to Blanchette et al.36 both the IASTM and the natural history approach are impacted in patients with lateral epicondylitis. Burke et al.38 claimed that IASTM and soft tissue mobilization in carpal tunnel syndrome increased wrist strength or its motion, and nerve conduction latencies.
Risk of Bias across Studies
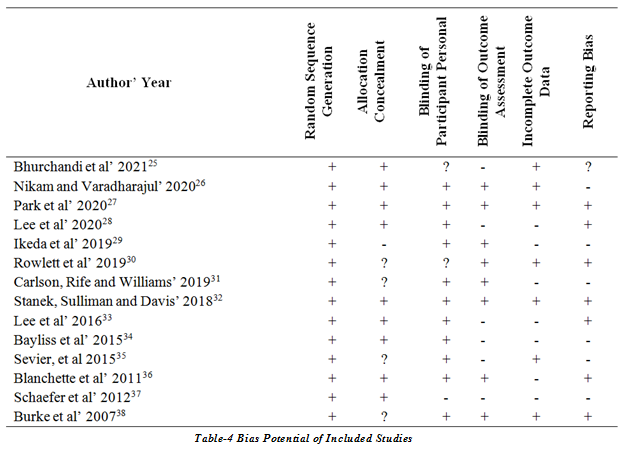
As stated in Table-4, the Cochrane Risk of Bias Tool was used to estimate the potential for bias premised on the author’s assessment for each trial that was included.
Selection Bias
Random Sequence Generation
All studies showed lower risk of bias.
Allocation Concealment
In contrast to one study29 that indicated a significant risk of bias, allocation concealment in nine studies25,26,27,28,32,33,34,36,37 revealed a low risk of bias. Four studies contained unidentified bias risks30,31,35,38.
Performance Bias
Blinding of Participants and Personnel
Participants in eleven trials were blinded, demonstrating the low risk of bias26,27,28,29,31,32,33,34,35,36,38. One study37 revealed a high risk of bias, while the bias in the other two25,30 trials was uncertain.
Detection Bias
Blinding of Outcome Assessment
Blinding of outcome assessment in eight researches 26,27,29,30,31,32,36,38indicated minimal bias risk, while in six studies 25,28,33,34,35,37 substantial biasness was evident.
Attrition Bias
Incomplete Outcome Data
Incomplete outcome data of seven studies 25,26,27,30,32,35,38 showed low risk whereas high biasness is observed in seven studies 28,29,31,33,34,36,37.
Reporting Bias
Selective Reporting
Reporting bias is low in seven studies27,28,30,32,33,36,38, high is six26,29,31,34,35,37 and unknown in one study25.
Discussion
This review included extensive literature searches and evaluations. The characteristics of the study were then gathered and examined in order to gauge the accuracy of the findings. IASTM techniques were recommended as potent therapeutic approaches for treating soft-tissue injuries based on recent studies. Our results indicate that all studies included in this systematic review used an IASTM approach, either alone or in conjunction with another therapy strategy, which was common to all patients in each study. The results of this review indicate that IASTM treatments are associated with both short and long-term improvements in functioning and pain relief.
Bhurchandi et al.25 discovered in their investigation that IASTM was superior to therapeutic ultrasound in reducing heel pain and enhancing general functionality. The results show that combining one of the two techniques with exercise training can eventually lead to improved functionality and pain relief. According to Nikam and Varadharajulu, IASTM combined with the use of a topical muscle relaxant may be helpful in addressing tissue extensibility insufficiency of the hamstrings in recreational runners26. Additionally; IASTM has a considerable and perceptible impact on soft tissues when combined with stretching exercises. According to Park et al.27 persistent ankle instability in taekwondo players improved range of motion, isokinetic muscular strength, and balance. IASTM and the roller massaging stick both demonstrated statistically significant improvements in active and passive ROM following a single treatment, according to Lee et al.28 Ikeda et al.29 discovered that after just one IASTM treatment, joint stiffness decreased and ankle dorsiflexion increased without changing the mechanical as well as neurological characteristics of the treated muscles.
Stretching and IASTM are both advised by Rowlett et al.30 who found no clinically significant differences between the treatment and control groups. The soleus muscle’s flexibility is improved by IASTM and stretching, as evidenced by an increase in range of motion when the knee is flexed. Therefore, it seems appropriate and beneficial to empower patients with weight-bearing ailments through self-stretching. Carlson and colleagues31 emphasized that the danger of injury is decreased following IASTM while improve ankle dorsiflexion leaping mechanics and increase post-surgery flexibility and range of motion, while the author did not differentiate between the particular advantages of both IASTM and tissue flossing. Only Stanek et al.32 used CMR rather than IASTM to detect an improvement in ankle dorsiflexion. Patients with reduced dorsiflexion experienced an improvement in it after just one session of CMR. Clinicians ought to look into CMR as a potential therapy for dorsiflexion-deficient patients. Lee et al.33 suggested the significant improvement in ROM and decrease in pain by using IASTM in chronic lower back pain patient. IASTM therapy increased tendon resting length, according to Bayliss et al.32 In the six patients studied thus far, there was no statistical advantage of IASTM in terms of performance on the lunge test. Sevier et al.35 have shown effectiveness of IASTM and eccentric exercises in tendinopathy patients. Blanchette et al.36 also suggest the effect of IASTM on pain in tendinitis patient. Schaefer and colleagues37 reported that IASTM therapy for chronic ankle instability increased FAAM, FAAM Sport, ROM, and SEBT in both sides but lowered VAS. Burke et al.38 noted that IASTM had a positive impact on the progression of carpal tunnel syndromes by enhancing wrist strength, wrist motion, and nerve conduction latencies.
This systematic review has a number of evident flaws. Only studies written in English were included, with the opportunity to access the entire text. A further constraining factor is the modest number of empirical researches that met the requirements for inclusion, as well as the challenge of finding high-quality studies with a minimal risk across all evaluation parameters. Because IASTM therapy impacts such a large proportion of the population, it’s critical to investigate long-term results. Another issue is that much of the study focuses on short-term therapies. Numerous studies failed to adequately describe the intervention, and some of the results did not properly indicate the risk. Furthermore, several of the publications do not provide a clear path to therapy and include low-quality research. No review study that chronicles emerging trends in enhancing functional activities, range of motion, and discomfort has, as far as the author is aware, been published anywhere in the world. Therefore, the researchers will have to investigate at clinical studies that significantly affected range of motion, flexibility and range of motion if they were to avoid bias and come up with reliable results.
Conclusion
It was established that IASTM had a short-term positive impact on the functionality of individuals with soft tissue injuries. Despite the fact that several of the papers were of low or ambiguous quality. The research on the long-term advantages of IASTM was not properly equipped due to the research design to allow for the establishment of robust and scalable conclusions. Last but not least, future study should focus on acquiring information on long-term consequences using credible evidence.
AUTHORS’ CONTRIBUTION:
The following authors have made substantial contributions to the manuscript as under:
Conception or Design: Hafiza Javeria, Danish Rasool, Dr. Ucksy Mallick
Acquisition, Analysis or Interpretation of Data: Hafiza Javeria, Danish Rasool, Dr. Ucksy Mallick
Manuscript Writing & Approval: Hafiza Javeria, Danish Rasool, Dr. Ucksy Mallick
All authors acknowledge their accountability for all facets of the research, ensuring that any concerns regarding the accuracy or integrity of the work are duly investigated and resolved.
ACKNOWLEDGEMENTS: We appreciate all participants.
INFORMED CONSENT: NIL
CONFLICT OF INTEREST: NIL
FUNDING STATEMENTS: None declared
ETHICS STATEMENTS: NIL
References
- Van der Worp MP, van der Horst N, de Wijer A, Backx FJ, Nijhuis-van der Sanden MW. Iliotibial band syndrome in runners. Sports medicine. 2012 Nov;42(11):969-92.
- Hart LE. Exercise and soft tissue injury. Baillière’s clinical rheumatology. 1994 Feb 1;8(1):137-48.
- Liu SH, Nguyen TM. Ankle sprains and other soft tissue injuries. Current opinion in rheumatology. 1999 Mar 1;11(2):132-7.
- Simpson MR, Howard TM. Tendinopathies of the foot and ankle. American family physician. 2009 Nov 15;80(10):1107-14.
- Narváez JA, Narváez J, Ortega R, Aguilera C, Sánchez A, Andía E. Painful heel: MR imaging findings. Radiographics. 2000 Mar;20(2):333-52.
- Watson AD, Anderson RB, Davis WH. Comparison of results of retrocalcaneal decompression for retrocalcaneal bursitis and insertional Achilles tendinosis with calcific spur. Foot & ankle international. 2000 Aug;21(8):638-42.
- Clar C, Tsertsvadze A, Hundt GL, Clarke A, Sutcliffe P. Clinical effectiveness of manual therapy for the management of musculoskeletal and non-musculoskeletal conditions: systematic review and update of UK evidence report. Chiropractic & manual therapies. 2014 Dec 1;22(1):12
- Slaven EJ, Mathers J. Management of chronic ankle pain using joint mobilization and ASTYM® treatment: a case report. Journal of Manual & Manipulative Therapy. 2011 May 1;19(2):108-12.
- Osborne MD, Rizzo TD. Prevention and treatment of ankle sprain in athletes. Sports Medicine. 2003 Dec;33(15):1145-50.
- Erden A, Şenocak E, Kalaycıoğlu A, Aktürk A. Effectiveness of instrument assisted soft tissue mobilization in myofascial pain syndrome: preliminary results of a randomized controlled trial. Sports Medicine Journal/Medicina Sportivâ. 2020 Jan 1;16(1).
- Martin RL, Davenport TE, Reischl SF, McPoil TG, Matheson JW, Wukich DK, McDonough CM, Altman RD, Beattie P, Cornwall M, Davis I. Heel pain—plantar fasciitis: revision 2014. Journal of Orthopaedic & Sports Physical Therapy. 2014 Nov;44(11):A1-33.
- Garrett TR, Neibert PJ. Graston Technique® as a Treatment for Patients with Chronic Plantar Heel Pain. Clinical Practice in Athletic Training. 2019 Nov 1;2(3):35-47
- Cheatham SW, Baker R, Kreiswirth E. Instrument assisted soft-tissue mobilization: a commentary on clinical practice guidelines for rehabilitation professionals. International journal of sports physical therapy. 2019 Jul;14(4):67
- Gamboa, A.J., Craft, D.R., Matos, J.A., Flink, T.S. and Mokris, R.L., 2019. Functional movement analysis before and after instrument-assisted soft tissue mobilization. International journal of exercise science, 12(3), p.46
- Kim J, Sung DJ, Lee J. Therapeutic effectiveness of instrument-assisted soft tissue mobilization for soft tissue injury: mechanisms and practical application. Journal of exercise rehabilitation. 2017 Feb;13(1):12.
- Looney B, Srokose T, Fernández-de-las-Peñas C, Cleland JA. Graston instrument soft tissue mobilization and home stretching for the management of plantar heel pain: a case series. Journal of manipulative and physiological therapeutics. 2011 Feb 1;34(2):138-42.
- Blanchette MA, Normand MC. Augmented soft tissue mobilization vs natural history in the treatment of lateral epicondylitis: a pilot study. Journal of manipulative and physiological therapeutics. 2011 Feb 1;34(2):123-30.
- Henry P, Panwitz B, Wilson JK. Treatment of a bilateral total knee replacement using augmented soft tissue mobilization. Physical Therapy Case Reports. 1999;2:27-30.
- Lambert M, Hitchcock R, Lavallee K, Hayford E, Morazzini R, Wallace A, Conroy D, Cleland J. The effects of instrument-assisted soft tissue mobilization compared to other interventions on pain and function: a systematic review. Physical Therapy Reviews. 2017 Mar 4;22(1-2):76-85.
- Laudner K, Compton BD, McLoda TA, Walters CM. Acute effects of instrument assisted soft tissue mobilization for improving posterior shoulder range of motion in collegiate baseball players. International journal of sports physical therapy. 2014 Feb;9(1):1.
- Davies CC, Brockopp D, Moe K. Astym therapy improves function and range of motion following mastectomy. Breast Cancer: Targets and Therapy. 2016;8:39.
- Sillevis R, Shamus E, Mouttet B. The Management of Plantar Fasciitis with a Musculoskeletal Ultrasound Imaging Guided Approach for Instrument Assisted Soft Tissue Mobilization in a Runner: A Case Report. International journal of sports physical therapy. 2020 Apr;15(2):274.
- Chughtai M, Mont MA, Cherian C, Cherian JJ, Elmallah RD, Naziri Q, Harwin SF, Bhave A. A novel, nonoperative treatment demonstrates success for stiff total knee arthroplasty after failure of conventional therapy. The journal of knee surgery. 2016 Apr;29(03):188-93.
- Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group*. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Annals of internal medicine. 2009 Aug 18;151(4):264-9.
- Bhurchandi, S., Sinha, R.K. and Phansopkar, P., 2021. Efficacy of Instrument Assisted Soft-Tissue Mobilization in patients with heel pain: An Experimental study.
- Nikam PP, Varadharajulu G. Effect of Pharmacotherapy-Combined Instrument-Assisted Soft Tissue Mobilization on Tissue Extensibility Dysfunction in Recreational Runners–A Randomized Controlled Trial. Journal of Evolution of Medical and Dental Sciences. 2020 Aug 31;9(35):2531-6.
- Park JH, Rhyu HS, Rhi SY. The effects of instrument-assisted soft tissue mobilization rehabilitation exercise on range of motion, isokinetic strength, and balance in chronic ankle instability taekwondo players. Journal of exercise rehabilitation. 2020 Dec;16(6):516.
- Lee J, Young A, Erb NJ, Herzog VW. Acute and residual effects of IASTM and roller massage stick on hamstring range of motion. Journal of allied health. 2020 Feb 27;49(1):51E-5E.
- Ikeda N, Otsuka S, Kawanishi Y, Kawakami Y. Effects of instrument-assisted soft tissue mobilization on musculoskeletal properties. Medicine and science in sports and exercise. 2019 Oct;51(10):2166.
- Rowlett CA, Hanney WJ, Pabian PS, McArthur JH, Rothschild CE, Kolber MJ. Efficacy of instrument-assisted soft tissue mobilization in comparison to gastrocnemius-soleus stretching for dorsiflexion range of motion: A randomized controlled trial. Journal of bodywork and movement therapies. 2019 Apr 1;23(2):233-40.
- Carlson S, Rife G, Williams Z. Comparing the Effects of Tissue Flossing and Instrument Assisted Soft Tissue Mobilization on Ankle Dorsiflexion.2019.
- Stanek J, Sullivan T, Davis S. Comparison of compressive myofascial release and the Graston Technique for improving ankle-dorsiflexion range of motion. Journal of athletic training. 2018 Feb;53(2):160-7.
- Lee JH, Lee DK, Oh JS. The effect of Graston technique on the pain and range of motion in patients with chronic low back pain. Journal of physical therapy science. 2016;28(6):1852-5.
- Bayliss AJ, Crandall T, Farmer DL, Warden SJ. Instrument-assisted soft tissue mobilization alters material and mechanical properties in healthy, shortened Achilles tendons. J Orthop Sports Phys Ther. 2015 Jan;45:24.
- Sevier TL, Stegink-Jansen CW. Astym treatment vs. eccentric exercise for lateral elbow tendinopathy: a randomized controlled clinical trial. PeerJ. 2015 May 19;3:e967.
- Blanchette MA, Normand MC. Augmented soft tissue mobilization vs natural history in the treatment of lateral.
The Ziauddin University is on the list of I4OA, I4OC, and JISC.
This is an open- access article distributed under the terms of the Creative Commons Attribution License (CC BY 4.0).
