Usama Mehmood 1*, Aqsa Tahir2
1Physiotherapist, Department Of Physical Therapy, The University Of Lahore, Pakistan![]()
2Physiotherapist, Department Of Physical Therapy, The University Of Lahore, Pakistan![]()
Abstract
Background and Aim: The majority of people suffered with low back pain (LBP) at least once during their lifetime. As such, LBP is a highly prevalent and costly condition. People respond inappropriately as a result of current or possible risks and establish defensive habits (for example, hyper-vigilance) that aim at avoiding new injuries. A continued reconciling of studies which provide various answers for the same issue will be necessary for treatment decisions. This study is performed to conclude the function of Kinesiophobia and check it on Pain, Disability and Quality of Life in Patients that are suffering from Chronic Low Back Pain: A Systematic Review.
Methodology: A Systematic Review has been conducted. Secondary data collected from Electronic database including PubMed, Medline and Cochrain Library from inception to 2010. Total 554 Article found out of which 10 articles included in the study after excluding the duplicate article, Quality screening through Pedro Scale, and article don’t fulfilling the inclusion criteria of the study. Review completed within 9 months after approval of synopsis.
Results: According to this Review total Sample size was 554 with mean Sample size 130±90, mean Age 46±5 years, Mean of Pain Intensity (VAS 0-10) 6.12±1.5, mean Pain Duration 30±14, mean Kinesiophobia Measures (Tampa Scale of Kinesiophobia 0-68) 37±6.5, mean Disability (Oswestry Disability Index 0-100%) 56±27, mean Quality of Life (SF 36 0-100) 39.17±15.197.
Conclusion: TSK scores showed a statistically significant correlation with Pain, Disability, education level, and SF-36 QOL. As the education level decreases, kinesiophobia scores increase and as kinesiophobia scores increase, Level of disability increases and the quality of life decreases. Patients with kinesiophobia presented greater pain intensity, a greater fear of movement and of performing physical activities and it was also associated with worse quality of life.
Keywords: Pain, disability, kinesiophobia, quality of life, chronic low back pain, pain intensity.
Introduction
The majority of people suffered with low back pain (LBP). They must experience once a time low back pain during their period of life. As such, LBP is a vastly widespread and expensive ailment1. The situation is the 2nd important source of disability in the general populations2. There are also several proven variables (cognitive, biological, physical, and social, mental, occupational) that results in underprivileged prognosis subsequent the start of low back pain3. This helps us to understand why several persons do not heal from an occurrence of lower back pain, often contributing to a plunging slide of detrimental bodily, societal and emotional effects [4]. In this respect, a substantial body of empirical indicates that disability, pain and standard of living are correlated with kinesiophobia5,6. In addition, long-term studies have demonstrated so, an elevated degree of starting point of kinesiophobe predicts adverse deviations in quality of life7, also a meaningful change in handicap plus discomfort8, 9.
A study of kinesiophobia’s prognostic effect on these outcomes will further enhance awareness of persistent LBP processes and thus allow enhanced decision-making in the clinical field [10]. Although kinesiophobia is typically measured through the Tampa Scale for kinesiophobia (TSK), no particular test is available to measure fear of movement11. It induces motor activity changes that impact the efficiency of organizational processes as well as control of pain and pain-related disability12.
The occurrence of kinesiophobia in chronic aching varies from 50% to 70%. This is likely in two ways: direct aversion (e.g., discomfort or trauma) or social education13. Second, pain-related information processing in patients with Chronic LBP may be correlated with how kinesiophobia is viewed. Kinesiophobia first affects how people walk, perhaps to prevent discomfort in the original target14,15. In this respect the greatest evidence has been found that weakness, pain, and standard of living are correlated with kinesiophobia16,17. However, confirmation is contradictory in the intensity of the importance and direction of the results8,18. Clinical decision-making calls for a continuous peaceful coexistence of research findings that can provide different responses to the very same discussion and also provides practitioners and patients with a summary in which uncertainty remains19.
A comprehensive examination of the results will lead to better results than any research has achieved and will make it possible for researchers to gather and analyze all the data from primary studies. The goal of this comprehensive examination would therefore be: investigate the degree to which patient with chronic back pain has connected kinesiophobia with discomfort, incapacity and quality of life. The objective is to determine the “Role of Kinesiophobia on Pain, Disability and Quality of Life in Patients with Chronic Low Back Pain: A Systematic Review”
Methodology
Study Design
Systematic Review
Key Data Bases
An automated search of PubMed, Medline and Cochrane Library will be undertaken from inception to August 2010.
Grey Literature Review
Trial registers, clinical study reports, dissertations and thesis, conference abstracts and proceedings.
Study Selection
Next, names and summaries will be screened. Secondly, the complete text of the manuscripts will be reviewed. Fourth, a decision shall be produced by consent and involvement in the event of any inconsistencies. A short guideline will also be used to direct the collection of the appropriate studies in this review.
Types of Study to be Included: Longitudinal, Cross-sectional and case-control trials.
Duration of study: The analysis will be carried out within nine months of the synopsis acceptance.
Sample selection criteria
In order to decide what experiments can be part of the ongoing clinical analysis, the P.E.C.O.S (P Patient, E- exposure, C-comparator; O- outcome, S-study design) structure will be adopted. Any research must run into the following
Inclusion Criteria
- Observatory trials investigating the potential validity of kinesiophobia in individuals with chronic LBP and their correlations with the results descripted below. (Cross-sectional, case management and longitudinal). When clinical trials only reported reasonably detailed observations from the baseline test, analysis methods among kinesiophobia and result variables stood restricted toward the initial evaluation.
- Studies with individuals with chronic LBP have described constant or episodic pain over 3 months across the lower back in this analysis
- Only research were included in the test kinesiophobia with TSK.
- The gender, nationality and tracking period of respondents (in longitudinal studies) would not be limited.
- Studies of general public, principal, secondary or tertiary treatment seeking patients.
- Would include were only documents available in English.
- Only when a link is identified regarding kinesiophobia and the foregoing results methods: pain, injury either or both quality of life, would research be included.
Exclusion Criteria
- Pain management research, subacute and non-musculoskeletal chronic pain. Research.
- Studies surrounding the diagnosis of significant psychological illnesses with which Chronic LBP is involved.
- Chronical LBP experiments measuring or examining this aspect before surgery or postoperative surgery linked to previous divides.
- Kinesiophobia research trials in persistent LBP people after injury.
- Revisions investigates the impact of kinesiophobia in trial pain model.
- Testing kinesiophobia in a clinical activity or rehabilitation (e.g., in vivo exposure).
- Case papers, editorials, summaries, and medical reviews.
Data extraction
The research information (first reporter, year of publishing), survey volumes, respondent attributes (mean age, pain length, state of pain), tests on kinesiophobia, the outcomes (pain, injury, standard of living), follow-up durations (longitudinal analysis), and the purpose of the study will be extracted. A mail was sent to the original writers if needed to collect more knowledge on observations from a report.
Quality assessment
An altered form of the Newcastle-Ottawa Scale (NOS) assesses the probability of bias of each sample. Four fields are covered in this improved version for bias evaluation risk: research selection of research procedures (selection bias), uncertainty control techniques (performance bias), arithmetical methodologies (detection bias) and contact measures and result measurement (material bias). The four realms consist of seven products. The scores for of component are between 0 (significant risk) and 3 (low risk). The highest score will then be 21 points for each analysis. Qualitative data analysis with a classification scale of five experimental data standards will be conducted20.
Statistical analysis
Research are classified according to results: injury, suffering and quality of life for primary research. Due to participant age, confidence interval, age discomfort, result assessments, a variant of the self-recounted kinesiophobia checklist (e.g. TSK-11 or TSK-17), statistics methodology and nature of the experiments of most research that could be suitable for met analysis, a meta-analysis cannot be conducted. A comprehensive quantitative method will therefore be given (the most appropriate statistical measure with a reliable estimate). We will derive the approximation from the model for certain experiments with many degrees of adaptation for confounders in various models.
Results
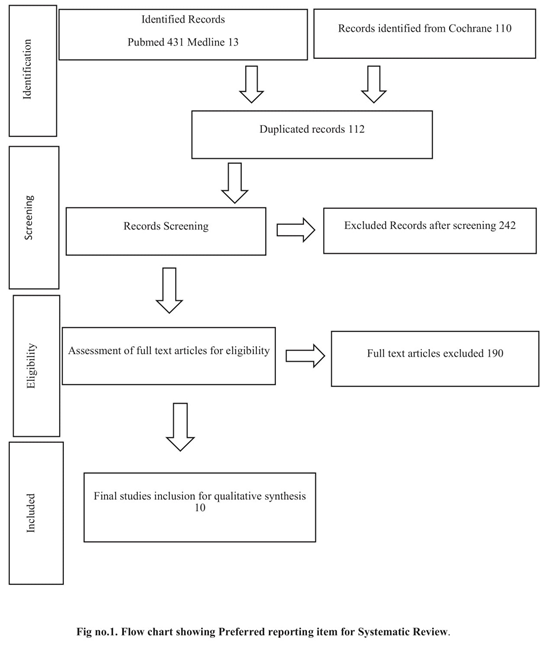
A systematic Review has been conducted among the online databases including PubMed, Medline and Cochrane Library. We found Number of Article 431 from PubMed, 13 from Medline and 110 from Cochrane Library, After initial check we found 112 duplicate Article, Then further Screening has been done and according to this screening 242 Articles were Excluded from the Present Systematic Review because they do not fulfill the inclusion criteria of the study, According to Eligibility Criteria of the Study we have to include only those Articles Which are freely available and the are available in full text. So 190 Articles were not full text Articles so we have excluded these Studies. Then Quality of the studies have been checked by Pedro Scale and Finally 10 Studies were included. Because they fulfil inclusion Criteria, and meets the standards of Quality assessment by Pedro Scale.
Outcome Measures
TSK scores showed a statistically significant correlation with Pain, Disability, education level, and SF-36 QOL.
Data for this Systematic Review has been collected from 2013 to 2020, Among Studies Included, 01 was published in 2020, 02 in 2019, 04 in 2018, and 01 in each including 2015, 3014, 2013. Total Sample size was 1309. Different parameters were recorded including Mean age in years, Intensity of Pain measure in VAS (0-10) Duration of Pain in months, Kinesiophobia was measure with (Tampa Scale of Kinesiophobia 0-68), Disability level was measured by Disability (Oswestry Disability Index 0-100%), Quality of Life was measured in Quality of Life (SF 36 0-100) follow the table 1:
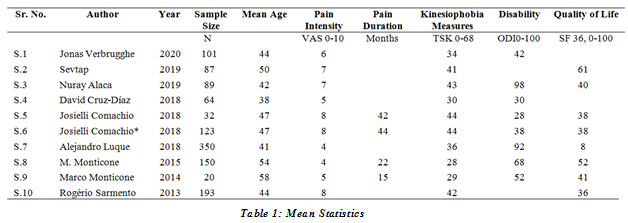
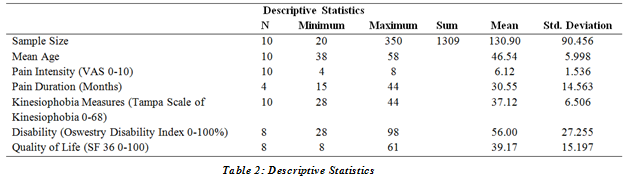
According to this Review total Sample size was 1309 with mean Sample size 130±90 minimum sample size was 20 and maximum was 350, mean Age 46±5 years with minimum Age was 38 and Age was 58, Mean of Pain Intensity (VAS 0-10) 6.12±1.5 with minimum Pain Intensity (VAS 0-10) was 4 and maximum was 8, mean Pain Duration (Months) 30±14 months with minimum Pain Duration (Months) was 15 and maximum Pain Duration (Months) was 44, mean Kinesiophobia Measures (Tampa Scale of Kinesiophobia 0-68) 37±6.5 with minimum Kinesiophobia Measures (Tampa Scale of Kinesiophobia 0-68) was 28 and maximum Kinesiophobia Measures (Tampa Scale of Kinesiophobia 0-68) was 44, mean Disability (Oswestry Disability Index 0-100%) 56±27 with minimum Disability (Oswestry Disability Index 0-100%) was 10 and maximum Disability (Oswestry Disability Index 0-100%) was 98, mean Quality of Life (SF 36 0-100) 39.17±15.197 with minimum Quality of Life (SF 36 0-100) was 8 and maximum was 61, follow the table 2:
Discussion
Data for this Systematic Review has been collected from 2013 to 2020, Among Studies Included, 01 was published in 2020, 02 in 2019, 04 in 2018, and 01 in each including 2015, 3014, 2013. Total Sample size was 1309. Different parameters were recorded including Mean age in years, Intensity of Pain measure in VAS (0-10) Duration of Pain in months, Kinesiophobia was measure with (Tampa Scale of Kinesiophobia 0-68), Disability level was measured by Disability (Oswestry Disability Index 0-100%), Quality of Life was measured in Quality of Life (SF 36 0-100) [21]. According to this Review total Sample size was 1309 with mean Sample size 130±90 minimum sample size was 20 and maximum was 350, mean Age 46±5 years with minimum Age was 38 and Age was 58, Mean of Pain Intensity (VAS 0-10) 6.12±1.5 with minimum Pain Intensity (VAS 0-10) was 4 and maximum was 8, mean Pain Duration (Months) 30±14 months with minimum Pain Duration (Months) was 15 and maximum Pain Duration (Months) was 44, mean Kinesiophobia Measures (Tampa Scale of Kinesiophobia 0-68) 37±6.5 with minimum Kinesiophobia Measures (Tampa Scale of Kinesiophobia 0-68) was 28 and maximum Kinesiophobia Measures (Tampa Scale of Kinesiophobia 0-68) was 44, mean Disability (Oswestry Disability Index 0-100%) 56±27 with minimum Disability (Oswestry Disability Index 0-100%) was 10 and maximum Disability (Oswestry Disability Index 0-100%) was 98, mean Quality of Life (SF 36 0-100) 39.17±15.197 with minimum Quality of Life was 8 and maximum was 6121.
Jonas Verbrugghe et, al. conducted analysis during 2020, the sample size of disability was 101, mean age: 44.2y (SD 1⁄4 9.6); this study showed kinesiophobia (TSK, 17e63) 34.01(6.10); intensity of pain (NPRS, 1e10) 5,67(1,60), discapacitance (Modi, percent), 21.08(10.10), data 101 pe Diagnostic Disability (NSD 1⁄4 9.6)). In the chronic non-specialized low back pain (NSPR, 1e10) The tests were not correlated with discapacity, neurological or pain-related causes. Back muscle mass variability (R2 1 1⁄4 0.44, f 1⁄4 p < 0.01), muscular abdominal strength (R2 1/40 0.68, f 1/2 p < 0.01). Aerobic capacity can only be demonstrated through demographic covariations including age, gender, weight. This is the only explanations that can be found in the following variations. This research demonstrated the absence of biopsychosocial influences to understand the heterogeneity of the abdominal, back and aerobic outcomes in CNSLBP individuals with defined in the current sample. This data help the accurate analysis of the findings of these tests21.
An analysis carried out by Sevtap Gunay Ucurum and. Al, in 2019, the aim of this analysis was for a sample size of 87 patients with mean age (year)50 ±5 TSK scores of 41 (49-45), Rest VAS 4 (2-6) VAS 7 (5-8), SF 36 GH 61(45–75) SF 36 MH 72, (52–80), Median age of 40, (40-59), 2014. The analysis was designed to detect a relation between pain seriousness, kinesiophobia and quality of life for non-specific chrónico-neck patient patients. The average VAS value at rest was 4 (2–6), and during the exercise the median VAS value was 7 (5–8). The average STR ratings were 41, the average SF-36 were 61 and the average SF-36 were 72 and the average SF-36 were 52 to 80. There is a small connexion between the TSK values, ethnicity, degree of education and the total wellbeing SF-36 (r = 0.206, p= 0.023; r = 0.235, p=0.004; r = 0.236 / p = 0.027). Kinesiophobia and the other variables were not related. TSK ratings demonstrated a correlation with the overall health values of ethnicity, education and SF-36. In conclusion, with the amount of education declining, the amount of kinesiophobia rises and the quality of life declines as kinesiophobia grows22.
A 2019 report by Nuray Alaca, Hande Kaba, Ayce Atalay and Roussel N. The goal of this trial was to establish differences in consistently low back pains with sample size 89 and the median age of participants, between seriousness of impairment and avoidance of movement and painful beliefs, was to be assessed by 42.29± 6.05, TKS 43.4±5.72, VAS (rest) 4.72±2.19 VAS (activity) 7.05 ± 1.54, ODI 49.72 18.66, SF 36 (Physical function) 39.83 ± 20. , There is a solid connection with the TKS appraisals, ages (r: 0.227/p < 0.05), natural PBQ evaluations (r: 0.250/p < 0.05). Our examination demonstrated raised degrees of kinesiophobia and comparative uneasiness, paying little heed to injury seriousness. We presume that LBP recuperation medicines ought to give psychological consistence directing that limits dread shirking action and transform negative torment discernments into helpful ones23.
Mostly people affected with musculoskeletal diseases at least for once in their lifetime24. In people with persistent lower-back pain and obesity, kinesiophobia may play a role in increasing pain-related disability and pain intensity25. To identify the hurdles that can influence rehabilitation outcomes, kinesiophobia screening should be addressed in routine clinical practice26.
Conclusion
Kinesiophobia, pain, impairment, and quality of life have been statistically significantly associated. TSK scores reported a significant association with pain, impairment, level of education, and SF-36 QOL. Kinesiophobia scores increase as the level of education decreases, and as kinesiophobia scores grow, the level of impairment rises and the quality of life decreases. Patients with kinesiophobia had a higher degree of pain, a greater fear of movement and physical activity, and a poorer standard of living was also associated.
AUTHORS’ CONTRIBUTION:
The following authors have made substantial contributions to the manuscript as under:
Conception or Design: Usama Mehmood
Acquisition, Analysis or Interpretation of Data: Aqsa Tahir
Manuscript Writing & Approval: Usama Mehmood & Aqsa Tahir
All authors acknowledge their accountability for all facets of the research, ensuring that any concerns regarding the accuracy or integrity of the work are duly investigated and resolved.
ACKNOWLEDGEMENTS: We thanks all the participants in this study.
INFORMED CONSENT: Written Informed Consent was taken from each patient.
CONFLICT OF INTEREST: The author (s) have no conflict of interest regarding any of the activity perform by PJR.
FUNDING STATEMENTS: None declared
ETHICS STATEMENTS: The study has been approved by the Ethical Board of University of Lahore, Pakistan.
References
- Emerson AJ, Hegedus T, Mani R, Baxter GDJPTR. Chronic musculoskeletal pain. Discordant management conversations: the influencing factor of polarized politics. 2020;25(1):7-20.
- Arsh A, Idrees S, Zafar N, Amin B, Ahad SJPM, Rehabilitationsmedizin, Kurortmedizin. Neck Pain & Disability among School Teachers and its Association with Gender, Body Mass Index, Classes per Week and Method of Lecture Delivery. 2020;30(03):180-3.
- Bento TPF, dos Santos Genebra CV, Maciel NM, Cornelio GP, Simeão SFAP, de Vitta A. Low back pain and some associated factors: is there any difference between genders? Brazilian Journal of Physical Therapy. 2020;24(1):79-87.
- Pate JW, Hancock MJ, Hush JM, Gray K, Pounder M, Pacey V. Prognostic factors for pain and functional disability in children and adolescents with persisting pain: A systematic review and meta‐ European Journal of Pain. 2020;24(4):722-41.
- Oskay D, Tuna Z, DÜZGÜN İ, ELBASAN B, Yakut Y, Tufan A. Relationship between kinesiophobia and pain, quality of life, functional status, disease activity, mobility, and depression in patients with ankylosing spondylitis. Turkish journal of medical sciences. 2017;47(5):1340-7.
- Meints SM, Mawla I, Napadow V, Kong J, Gerber J, Chan S-T, et al. The relationship between catastrophizing and altered pain sensitivity in patients with chronic low back pain. Pain. 2019;160(4):833.
- Wong WS, Chow YF, Chen PP, Wong S, Fielding R. A longitudinal analysis on pain treatment satisfaction among Chinese patients with chronic pain: predictors and association with medical adherence, disability, and quality of life. Quality of Life Research. 2015;24(9):2087-97.
- Helminen E-E, Sinikallio SH, Valjakka AL, Väisänen-Rouvali RH, Arokoski JP. Determinants of pain and functioning in knee osteoarthritis: a one-year prospective study. Clinical rehabilitation. 2016;30(9):890-900.
- Van Den Houte M, Luyckx K, Van Oudenhove L, Bogaerts K, Van Diest I, De Bie J, et al. Differentiating progress in a clinical group of fibromyalgia patients during and following a multicomponent treatment program. Journal of Psychosomatic Research. 2017;98:47-54.
- Tagliaferri SD, Miller CT, Owen PJ, Mitchell UH, Brisby H, Fitzgibbon B, et al. Domains of chronic low back pain and assessing treatment effectiveness: A clinical perspective. Pain Practice. 2020;20(2):211-25.
- Vibe Fersum K, Smith A, Kvåle A, Skouen JS, O’Sullivan P. Cognitive functional therapy in patients with non‐specific chronic low back pain—a randomized controlled trial 3‐year follow‐ European Journal of Pain. 2019;23(8):1416-24.
- Karos K, Meulders A, Gatzounis R, Seelen HA, Geers RP, Vlaeyen JW. Fear of pain changes movement: Motor behaviour following the acquisition of pain‐related fear. European journal of pain. 2017;21(8):1432-42.
- Meier ML, Stämpfli P, Vrana A, Humphreys BK, Seifritz E, Hotz-Boendermaker S. Fear avoidance beliefs in back pain-free subjects are reflected by amygdala-cingulate responses. Frontiers in human neuroscience. 2015;9:424.
- Malfliet A, Van Oosterwijck J, Meeus M, Cagnie B, Danneels L, Dolphens M, et al. Kinesiophobia and maladaptive coping strategies prevent improvements in pain catastrophizing following pain neuroscience education in fibromyalgia/chronic fatigue syndrome: An explorative study. Physiotherapy theory and practice. 2017;33(8):653-60.
- Alaca N, Kaba H, Atalay AJJob, rehabilitation m. Associations between the severity of disability level and fear of movement and pain beliefs in patients with chronic low back pain. 2020;33(5):785-91.
- Altuğ F, Ünal A, Kilavuz G, Kavlak E, Çitişli V, Cavlak U. Investigation of the relationship between kinesiophobia, physical activity level and quality of life in patients with chronic low back pain 1. Journal of back and musculoskeletal rehabilitation. 2016;29(3):527-31.
- Gunay Ucurum SJJob, rehabilitation m. The relationship between pain severity, kinesiophobia, and quality of life in patients with non-specific chronic neck pain. 2019;32(5):677-83.
- Schmelz M, Mantyh P, Malfait A-M, Farrar J, Yaksh T, Tive L, et al. Nerve growth factor antibody for the treatment of osteoarthritis pain and chronic low-back pain: mechanism of action in the context of efficacy and safety. Pain. 2019;160(10):2210.
- Tu Y, Jung M, Gollub RL, Napadow V, Gerber J, Ortiz A, et al. Abnormal medial prefrontal cortex functional connectivity and its association with clinical symptoms in chronic low back pain. Pain. 2019;160(6):1308-18.
- Peterson J, Welch V, Losos M, Tugwell PJ. The Newcastle-Ottawa scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa: Ottawa Hospital Research Institute. 2011;2(1):1-2.
- Comachio J, Magalhães MO, Marques AP. A cross-sectional study of associations between kinesiophobia, pain, disability, and quality of life in patients with chronic low back pain. Advances in Rheumatology. 2018;58.
- Cruz-Díaz D, Romeu M, Velasco-González C, Martínez-Amat A, Hita-Contreras F. The effectiveness of 12 weeks of Pilates intervention on disability, pain and kinesiophobia in patients with chronic low back pain: a randomized controlled trial. Clinical rehabilitation. 2018;32(9):1249-57.
- Verbrugghe J, Agten A, Stevens S, Eijnde BO, Vandenabeele F, Roussel N, et al. Disability, kinesiophobia, perceived stress, and pain are not associated with trunk muscle strength or aerobic capacity in chronic nonspecific low back pain. Physical Therapy in Sport. 2020.
- Luque-Suarez A, Martinez-Calderon J, Falla D. Role of kinesiophobia on pain, disability and quality of life in people suffering from chronic musculoskeletal pain.
- Varallo G, Giusti EM, Scarpina F, Cattivelli R, Capodaglio P, Castelnuovo G. The association of kinesiophobia and pain catastrophizing with pain-related disability and pain intensity in obesity and chronic lower-back pain. Brain Sciences. 2021 Jan;11(1):11.
- Asiri F, Reddy RS, Tedla JS, ALMohiza MA, Alshahrani MS, Govindappa SC, Sangadala DR. Kinesiophobia and its correlations with pain, proprioception, and functional performance among individuals with chronic neck pain. PloS one. 2021 Jul 8;16(7):e0254262.
The Ziauddin University is on the list of I4OA, I4OC, and JISC.
This is an open- access article distributed under the terms of the Creative Commons Attribution License (CC BY 4.0).
