Umair Khalid1*, Khuram Chaudry2, Hina Khuram3
1*Clinical Director, Jag One Physical Therapist Brooklyn, New York![]()
2Freelancer, Physical Therapist Ontario, Canada![]()
3Physiotherapist, The Mc Causland Hospital Ontario, Canada![]()
Abstract
Objective: Diabetes is more prevalent mainly in Asian population, but the incidence proportion and likelihood are still unknown due to lack of evidence and proper research, therefore in this research paper the main aim is to assess the relative risk of diabetes mellitus in obese people in Pakistan.
Methodology: A case control study was conducted on 233 participants including diabetic and non-diabetic. The participants were approached from different clinics and hospitals from Nov 2021 to April 2022 using convenient sampling technique. Participants’ age, body mass index and weight category were measured. The odds and relative risk ratio were calculated for diabetic patients in obese people.
Results: It was found that among the obese population, the odds of having diabetes were 3.85 times greater than that of non-obese adults whereas relative risk was also found to 2.17 times higher than that of non-obese population with the p-value <0.05.
Conclusions: The prevalence of obesity is higher in diabetic population as compared to non-diabetic individuals. This increases the chances of developing diabetes in obese population as compared to the individuals with normal weight.
Keywords: Diabetes, obesity, odds ratio, risk, body mass index, prevalence.
Introduction
United Nations and the World Health Organization (WHO) focused on diabetes as a major global health concern in view of the enormous worldwide epidemic1,2. The International Diabetes Federation IDF estimates that over 415 million people had diabetes globally in 2015, and that figure is predicted to increase to 640 million by 20403. Despite the fact that more than 12% of global health expenditure was allocated to addressing the condition and its effects in the same year 2015, diabetes was responsible for an estimated 5.0 million deaths3. According to the reports of Centers for Disease Control and Prevention, 8.7% of the US population, or 28.7 million persons of all ages had diabetes4. As of today, there are differences that are maintained among different ethnic groups around the world, it is recorded lower among whites as compared to black or Hispanic groups. According to a report, the indicator of diabetes mellitus disorder has not significantly changed among black groups5.
Earlier 2018, the only prior national diabetes survey in Pakistan from 1999 (published in 2007), using the oral glucose tolerance test, found a prevalence of type 2 diabetes of 11%6. The IDF reported in its Atlas 5th edition regarding the prevalence for Pakistan to be 6.8% in between aged group of 20–79 years, but healthcare professionals with local insight always believed this to be an underestimate. Subsequently, there were conflicting findings with prevalence ranging from7.2% to 19.21% in different regions of the country7,8.
Along with an increase in life expectancy due to tremendous progress in multifactorial cardiovascular risk management and successful revascularization therapy for people with diabetes, the global obesity epidemic has emerged as a critical factor in the rise of diabetes incidence in addition to the general growth and ageing of the world’s population. These developments have also contributed to the expansion of the global diabetes population8,9. A report shows that the current trend of the world population’s BMI is rising from 20.1%, suggesting that diabetes mellitus disease may rise due to an increase in obesity or the fact that 85.1% of the population will suffer from type 2 diabetes malleitus10.
It was discovered that having a high body mass index (BMI) enhanced a diabetic’s risk for significant complications. Diabetes can have long-term complications like retinopathy, which can cause blindness; nephropathy, which can cause renal failure; peripheral neuropathy, which can cause foot ulcers, amputations, and Charcot’s joints, and autonomic neuropathy, which can cause symptoms in the gastrointestinal, genitourinary, and cardiovascular systems as well as sexual dysfunction11. In addition to other health issues, people with diabetes are more likely to develop peripheral arterial, cerebrovascular, and atherosclerotic cardiovascular diseases. High blood pressure and issues with lipoprotein metabolism are often associated with diabetes12.
Diabetes mellitus type 2 is increasing in prevalence among people worldwide for a variety of causes, including ongoing imbalances in dietary patterns, food components, and environmental, physiological, behavioral, social, and economic factors13-14. Even though diabetes mellitus and obesity are related, and the world population continues to have a high rate of diabetes, people are
becoming more and more addicted to fast food and other goods that include sugar and other components that contribute to fat15-16. A study conducted in Spain17 to estimate the prevalence of obesity and its association with other health related condition including diabetes and hypertension, they found prevalence of obesity and diabetes to be 18.4% and 7.6% along with significant association, however, odds and relative risk ratio was not calculated. While a study18 contrary to this believes, stating that obesity is not the cause of type 2 Diabetes Mellitus DM, but the resistance developed through T2DM predisposed to diabetes before they become obese. This debate yet not cleared in literature with evidence of odds ratio and relative risk of DM among obese population and no study has been discovered to be conducted in Pakistan that analyses the risk of diabetes, particularly in those who are obese. Therefore, research in Pakistan is needed to identify the population at risk in order to promote awareness of obesity as a risk factor for diabetes, to offer guidance, and prevent future generations.
Methodology
Study Design and Sampling Technique
A case control study was conducted on diabetic and non-diabetic individuals during the period of Nov 2021 to April 2022 in different clinics and hospitals of Karachi, Pakistan. A total of 230 participants were enrolled in the study using non-probability convenience sampling technique. Peak visiting hours of participants was considered to avoid any inconvenience, mismanagement, or inefficiency in the data gathering procedure.
Study Participants and Selection Criteria
Participants both male and female with age group of 20 to 60 years, who were already diagnosed with type II Diabetes mellitus through their Diabetologists were included in the study as case groups where as for the control group individuals who do not have diabetes mellitus type II were included with same age group. Participants who were pregnant or those who refused to be a part of study were excluded from study.
Procedure
Following the recruitment of participants, written informed consent was taken with a brief introduction of research study and its advantages and disadvantages. A questionnaire was given to them, comprised of 14 statements related to the symptoms and severity of diabetes they are suffering. Individuals who are unable to read or write, assistance was provided to them by data collector and their preferred answer was marked on the questionnaire. Following the collection of filled questionnaire, participant’s weight and height was measured using stadiometer and their BMI was calculated.
Data Analysis Strategy
Data was entered on SPSS version 20. Descriptive statistics including mean and standard deviation were used to demonstrate numerical variable and for categorical variable frequency and percentage was calculated. Odds and relative risk ratio were calculated for diabetic individuals with obesity.
Ethical Considerations
The data was kept confidential and the participants were provided with full autonomy to take part in the research. Further, all the causation of harm was avoided to the participant throughout the study. The study was performed with the ethical standard of Helsinki Declaration.
Results
A total of 233 participants, out of which 95 (40.8%) were diabetic and 138 (59.2%) were non-diabetic. Overall male was 51.5 % of the participants and female were 48.5% whereas in diabetic group, 55.8% were male and 44.2% were female and in non-diabetic group, female were found at greater proportion 56.5%. The mean age of the participants was 38.27±12.9 and BMI was 26.5±5.4. In diabetic group, most of the participants were from obese category, however in non-diabetic group, normal weight was more prevalent, described in Table 1.
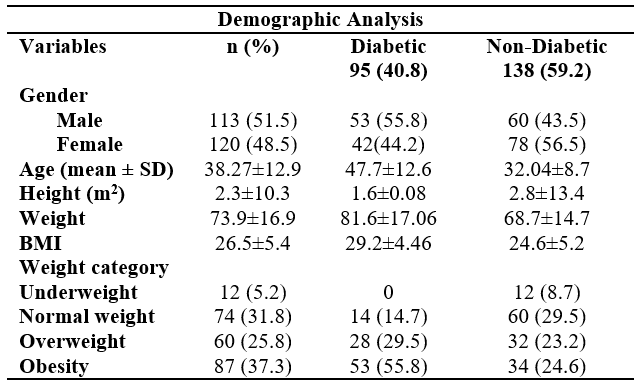
Table 1: Participants clinical characteristics
The prevalence of diabetes among the population was estimated to be 40.7% and the prevalence of obesity was reported to be 37.3% among the population. In diabetic group, the prevalence of obesity was found to be 55.7% whereas in non-diabetic group, it was found to be 24.6%. Relative risk and Odds ratio of developing diabetes was also estimated among the obese population as compare to non-obese population and it was observed that among the obese population, the odds of having diabetes were 3.85 times greater than that of non-obese adults and relative risk was also found 2.17 times higher than that of non-obese population and that too were statistically significantly with the p-value <0.05 at 95% of CI. It was revealed from the analysis that out of total number of 233 participants, n=53 of the participants were found to be both obese and diabetic whereas n=34 were found to be obese only and n= 42 were identified as only diabetic with no obesity, suggesting that risk of diabetes increased in the presence of obesity as illustrated in table 2.
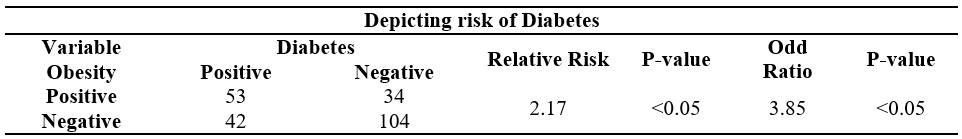
Table 2: Depicting risk of Diabetes
Discussion
In this research, we discovered that 40.8% of the population had diabetes, with gender-specific prevalence rates for men and females of 55.8% and 44.2%, respectively. Despite the fact that both genders’ lifetime risk of diabetes is closely correlated with BMI, men’s incremental absolute risk increases between overweight and obese persons are greater than those between normal weight and overweight adults. These outcomes are in line with the findings that those with BMIs below 30 kg/m2 clearly have greater mortality risks19,20. Recent studies of national diabetes trends also show that those with a BMI under 30 kg/m2 have experienced the vast bulk of the secular rise in diabetes21. The relative risk in our research was likewise discovered to be 2.17 times significantly greater (p<0.05) than that of the non-obese group, at 95% of confidence interval. Previously a meta-analysis conducted in which 18 of the studies were pooled and according to this, those who are obese have a 7 times greater chance of developing diabetes than people who are of normal weight. Those who were overweight had a 3 times increased chance of developing diabetes than those who were of normal weight. Also the overall relative risk was higher than for obese men22. According to a study23, obesity is more strongly associated with type 2 diabetes than an unhealthy lifestyle, with obese people having a >8-fold increased chance of developing the disease. Another study conducted in India has found that obese persons had a moderately association with type 2 diabetes mellitus and a strongly positive association with hypertension24.
According to a study, people with a BMI over 40 have higher odds of being diagnosed with diabetes (7.37 OR; 95% CI, 6.39–8.5), hypertension (6.39 OR; 95% CI, 5.67–7.16), and hypercholesterolemia (1.88 OR; 1.67–2.13)25. The increased influx of glucose is thought to be responsible for the pathophysiology of obesity. The potential to increase subcutaneous adipose tissue mass, particularly in the gluteal-femoral region, may allow persons who are overweight or obese to be at far lower risk than anticipated when faced with excessive energy intake26.
Individual lifestyle changes should be required to lower the risk of diabetes occurrence in obese people. To combat the obesity epidemics, a variety of strategies have been put forward, often advising a variety of food and/or physical exercise with behavioral support. At least temporarily, there are many methods for stopping the development of pre-diabetes to diabetes in obese people, including dietary and activity changes, pharmacological treatments, and other therapies. At least two meta-analyses have shown that a large weight reduction is the most efficient way to stop the development of pre-diabetes to diabetes during obesity27.
The case control study design was strength of our study that evaluated the difference in healthy individuals and obese population depicting risk in both group of peoples. The limitation of this study is small sample size, could have been done on larger sample size to avoid recall bias in the result. Future studies should find relative risk with respect to each weight category and with incorporation of lifestyle in predicting the odds and relative risk ratio.
Conclusion
The study concluded that the prevalence of obesity is higher in diabetic population as compared to non-diabetic individuals. This increases the chance of developing diabetes as compared to normal weight individuals. The risk of having obesity related complications like diabetes is also increasing which may lead to mortality and morbidity. Thus the risk stratification may help us identified the level of damage that obesity may cause. This will help in preventive care for the population. In order to reduce the risk of obesity and diabetes among the people, individual lifestyle modification should be required immediately that includes changes in diet, sleeping habits, exercises, and other therapies.
AUTHORS’ CONTRIBUTION:
The following authors have made substantial contributions to the manuscript as under:
Conception or Design: Umair Khalid
Acquisition, Analysis or Interpretation of Data: Hina Khuram
Manuscript Writing & Approval: Khuram chaudry
All authors acknowledge their accountability for all facets of the research, ensuring that any concerns regarding the accuracy or integrity of the work are duly investigated and resolved.
ACKNOWLEDGEMENTS: We would like to offer our special thanks to all the participants and their families for their support in conducting this research study
INFORMED CONSENT: Written Informed Consent was taken from each patient.
CONFLICT OF INTEREST: The author (s) have no conflict of interest regarding any of the activity perform by PJR.
FUNDING STATEMENTS: None declared
ETHICS STATEMENTS: Before starting the data collection ethical consideration was taken via written and verbal
consent by the participant.
Reference
- Standl E, Khunti K, Hansen TB, Schnell O. The global epidemics of diabetes in the 21st century: Current situation and perspectives. Eur J Prev Cardiol. 2019 Dec 1;26(2_suppl):7-14.
- Khan MA, Hashim MJ, King JK, Govender RD, Mustafa H, Al Kaabi J. Epidemiology of type 2 diabetes–global burden of disease and forecasted trends. J Epidemiol Glob Health. 2020 Mar;10(1):107.
- Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, Colagiuri S, Guariguata L, Motala AA, Ogurtsova K, Shaw JE. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas. Diabetes research and clinical practice. 2019 Nov 1;157:107843.
- Centers for Disease Control and Prevention [Internet]. CDC. 2022 [cited 7 September 2022]. Available from: https://www.cdc.gov/diabetes/data/statistics-report/diagnosed-diabetes.html
- Haw JS, Shah M, Turbow S, Egeolu M, Umpierrez G. Diabetes complications in racial and ethnic minority populations in the USA. Curr Diab Rep . 2021 Jan;21(1):1-8.
- Aamir AH, Ul-Haq Z, Mahar SA, Qureshi FM, Ahmad I, Jawa A, Sheikh A, Raza A, Fazid S, Jadoon Z, Ishtiaq O. Diabetes Prevalence Survey of Pakistan (DPS-PAK): prevalence of type 2 diabetes mellitus and prediabetes using HbA1c: a population-based survey from Pakistan. BMJ open. 2019 Feb 1;9(2):e025300.
- Meo SA, Zia I, Bukhari IA, Arain SA. Type 2 diabetes mellitus in Pakistan: Current prevalence and future forecast. J Pak Med Assoc. 2016 Dec 1;66(12):1637-42.
- Harding JL, Pavkov ME, Magliano DJ, Shaw JE, Gregg EW. Global trends in diabetes complications: a review of current evidence. Diabetologia. 2019 Jan;62(1):3-16.
- Newman JD, Schwartzbard AZ, Weintraub HS, Goldberg IJ, Berger JS. Primary prevention of cardiovascular disease in diabetes mellitus. J Am Coll Cardiol. 2017 Aug 15;70(7):883-93.
- Aamir, A.H., Ul-Haq, Z., Fazid, S., Shah, B.H., Raza, A., Jawa, A., Mahar, S.A., Ahmad, I., Qureshi, F.M. and Heald, A.H., 2020. Type 2 diabetes prevalence in Pakistan: what is driving this? Clues from subgroup analysis of normal weight individuals in diabetes prevalence survey of Pakistan. Cardiovasc Endocrinol Metab., 9(4), p.159.
- American Diabetes Association, 2019. 11. Microvascular complications and foot care: standards of medical care in diabetes—2019. Diabetes Care, 42(Supplement_1), pp.S124-S138.
- EL-Ashmawy HM, Omar RE, Almazouq FM, Ahmed AM. Possible Role of Fatty Acid Binding Protein in Type 2 Diabetes and Peripheral Artery Disease. Egypt J Hosp Med. 2022 Oct 1;89(1):4270-2.
- Sami W, Ansari T, Butt NS, Ab Hamid MR. Effect of diet on type 2 diabetes mellitus: A review. Int J Health Sci. 2017 Apr;11(2):65.
- Rajput SA, Ashraff S, Siddiqui M. Diet and Management of Type II Diabetes Mellitus in the United Kingdom: A Narrative Review. Diabetology. 2022 Feb 7;3(1):72-8.
- Jung CH, Son JW, Kang S, Kim WJ, Kim HS, Kim HS, Seo M, Shin HJ, Lee SS, Jeong SJ, Cho Y. Diabetes fact sheets in Korea, 2020: an appraisal of current status. Diabetes Metab J. 2021 Jan 13;45(1):1-0.
- Chobot A, Górowska‐Kowolik K, Sokołowska M, Jarosz‐Chobot P. Obesity and diabetes—Not only a simple link between two epidemics. Diabetes/metabolism research and reviews. 2018 Oct;34(7):e3042.
- Ramón-Arbués E, Martínez-Abadía B, Gracia-Tabuenca T, Yuste-Gran C, Pellicer-García B, Juárez-Vela R, Guerrero-Portillo S, Sáez-Guinoa M. Prevalence of overweight/obesity and its association with diabetes, hypertension, dyslipidemia and metabolic syndrome: a cross-sectional study of a sample of workers in Aragón, Spain. Nutr Hosp. 2019;36(1):51-9.
- Malone JI, Hansen BC. Does obesity cause type 2 diabetes mellitus (T2DM)? Or is it the opposite?. Pediatr Diabetes. 2019;20(1):5-9.
- Zucker I, Zloof Y, Bardugo A, Tsur AM, Lutski M, Cohen Y, Cukierman-Yaffe T, Minsky N, Derazne E, Tzur D, Melzer Cohen C. Obesity in late adolescence and incident type 1 diabetes in young adulthood. Diabetologia. 2022 Jun 5:1-0.
- Fruh SM. Obesity: Risk factors, complications, and strategies for sustainable long‐term weight management. J Am Assoc Nurse Pract. 2017 Oct;29(S1):S3-14.
- Mathur P, Leburu S, Kulothungan V. Prevalence, awareness, treatment and control of diabetes in India from the countrywide National NCD Monitoring Survey (NNMS). Public health frontier. 2022 Mar 14:205.
- Abdullah A, Peeters A, de Courten M, Stoelwinder J. The magnitude of association between overweight and obesity and the risk of diabetes: a meta-analysis of prospective cohort studies. Diabetes Res Clin Pract. 2010 Sep 1;89(3):309-19.
- Schnurr TM, Jakupović H, Carrasquilla GD, Ängquist L, Grarup N, Sørensen TI, Tjønneland A, Overvad K, Pedersen O, Hansen T, Kilpeläinen TO. Obesity, unfavourable lifestyle and genetic risk of type 2 diabetes: a case-cohort study. Diabetologia. 2020 Jul;63(7):1324-32.
- Babu GR, Murthy GV, Ana Y, Patel P, Deepa R, Neelon SE, Kinra S, Reddy KS. Association of obesity with hypertension and type 2 diabetes mellitus in India: A meta-analysis of observational studies. World J Diabetes. 2018 Jan 1;9(1):40.
- Glovaci D, Fan W, Wong ND. Epidemiology of diabetes mellitus and cardiovascular disease. Curr Cardiol Rep.2019 Apr;21(4):1-8.
- Piché ME, Tchernof A, Després JP. Obesity phenotypes, diabetes, and cardiovascular diseases. Circ Res. 2020;126(11):1477-500.
- La Sala L, Pontiroli AE. Prevention of diabetes and cardiovascular disease in obesity. Int J Mol Sci. 2020 Oct 31;21(21):8178.
The Ziauddin University is on the list of I4OA, I4OC, and JISC.
This is an open- access article distributed under the terms of the Creative Commons Attribution License (CC BY 4.0).
