Syeda Anum Riaz 1*, Muhammad Usman2
1*Incharge Physiotherapist, DPT, Rabia Moon Memorial Institute of Neurosciences (Trust), Pakistan![]()
2Senior Lecturer, Bahria University College of Physical Therapy Bahria University Health Sciences, Pakistan![]()
ABSTRACT
Objective: To determine the effect of static stretching of hamstring muscle on the non-specific low back pain.
Methodology: A Quasi-Experimental study was conducted in Rabia Moon Institute of Neurology which total 30 participants were included through non-probability purposive sampling. Thirty participants were selected who fulfilled our inclusion criteria, they were divided into two groups; group A or treatment group received conventional physiotherapy treatment as well a static stretching exercise protocol for 5 days. Group B or control group received conventional physiotherapy treatment only. VAS (Visual analog scale) and Oswestry Disability questionnaire, SFGD (Standing Finger to ground Distance,) PSLR (passive straight leg raise) for both legs were measured pre- and post-treatment.
Result: A total of 30 patients aged 20-55 were included in the study. Mean age of the participants was found to be 37.88 years. The difference in means of all the assessment parameters pre and post-treatment for both groups were analyzed through paired t-test. There was a significant improvement in VAS, SFGD, Passive Straight leg Raise PSLR (right leg), PSLR (left leg) and level of disability pre- and post-treatment in the treatment group.
Conclusion: This present study concluded that static stretching of hamstrings is effective in decreasing non-specific low back pain.
Keywords: Oswestry disability index questionnaire, nonspecific back pain, static hamstrings stretching, altered lumbo-pelvic rhythm, posture, passive straight leg raise.
Introduction
Almost everyone will have low back pain (LBP) at some point in their lives. The disorder, which has an impact on daily functioning, can be divided into two categories: non-specific low back pain and specific low back pain. In 1990, 377.5 million people worldwide have LBP at any given moment; by 2017, this number had risen to 577.0 million. Females had a higher age-standardized prevalence of LBP than males’ did2.
Ethnic, community and financial homogeneity is not a feature of an underdeveloped country like Pakistan. The genetic diversity, differences in social makeup and difference in economic conditions between privileged and underprivileged nations that may trigger the difference in prevalence of low back pain is debatable. In general; the incidence of 8–30 days of (moderate) nonspecific low back pain in a year reported to be 13.2%4. There is a high prevalence of self-reported non-specific low-back pain in urban compared to rural populations, which is 39.3% and 31.3% respectively, according to a cross-sectional study done in 2018 and 2019 respectively to find out the different risk factors for developing mechanical chronic LBP in the rural and urban societies of Pakistan5,6.
Muscle tightness or stiffness below the costal margin up to the top of the inferior gluteal folds is referred to as low back discomfort. It may or may not be accompanied by sciatica or leg discomfort. Non-specific low back pain is defined as symptoms without a clear-cut explanation, also known as low back pain with no recognized aetiology. A specific somatic cause is identified in only 15% to 20% of patients, Only 15% to 20% of patients have a particular somatic cause identified; non-specific LBP is diagnosed by ruling out all diseases, and it refers to a symptom or, at its worst, a syndrome rather than a diagnosis. 90% of people with low back pain have non-specific causes for their symptoms10.
Numerous studies have shown a connection between low back discomfort and the flexibility of the hamstring muscles. Except for the short head of the bicep femoris, which attaches distally below the knee to the medial surface of the proximal tibia (semimembranosus and semitendinosus) and the lateral side of the head of the fibula, hamstring muscles attach proximally to the ischial tuberosity (biceps femoris). It is a knee flexor and a hip extensor muscle. The erector spinae, which runs close to the spine and aids in posture, core stabilization, and spinal movement, are the muscles that connect the top section of the pelvis to the spine. Hamstrings that are too tight start to restrict pelvic movement. Therefore, if the Therefore, restricted pelvic movement will result in tense back muscles, which may cause low back pain13.
Decreased hamstring extensibility causes decrease in lumbar lordotic curve due to increased posterior pelvic tilt and therefore causes low back pain, it also reduces pelvic mobility and distorted lumbo-pelvic rhythm. It has been proposed that a decrease in flexibility in hamstrings will put undue pressure on lumber extensor muscles so as to maintain the pelvic motion, which will eventually lead to the development of low back pain. Increasing hamstring flexibility will increase the movement of the pelvis, which will in turn seize tension off low back; serving to decrease pain in back15.
Lumbo-pelvic rhythm is required for the motion of bending over to touch one’s toes with straight knees. Lumbar flexion and anterior pelvic tilting at the hip joint make up the first portion of the forward bending. A posterior pelvic tilt at the hip joint, followed by lumbar spine extension, simulates a restoration to the upright position. The first movement of the pelvis delays lumbar extension until the trunk has been elevated high enough to shorten the moment arm, which lessens the strain on the erector spinae16. A person may lose rhythm and be unable to touch her toes if there is a restriction in movement at the hip or lumbar spine. Hypermobility of one section due to motion restriction17.
Decreased extensibility of hamstring is known as both standing finger to ground distance of greater than 0 cm and a supine hip flexion leg lift angle of <80º18. pSLR is used to measure hamstring flexibility. pSLR, is a standard test and has been demonstrated to have a reliability of 0.9719. Tight hamstring is a common finding in people with low back pain. Literature lacks the evidence whether static stretching o hamstring done in order to improve hamstring length has a positive impact on reducing low back pain or not. Since the pelvis serves as the foundation of the spine and the hamstrings have their origin in the pelvis, tension in this muscle may affect how the pelvis sits. As a result, low back discomfort may develop if the hamstrings are too weak or rigid to maintain pelvic control. This study focused on whether static hamstring stretching helps people with low back pain. The study was aimed to find out the effect of static stretching of hamstrings on non-specific low back pain.
Methodology
A Quasi-Experimental study was conducted in Rabia Moon Institute of Neurology where total 30 participants were included through non-probability purposive sampling20. All participants were divided into two groups. Group A consist of 15 participants in which we gave conventional physiotherapy treatment along with static hamstring stretching on other hand group B contained participants who were given a conventional physical therapy treatment only for low back pain. Each participant of both groups performed for 5 days a week for 4 weeks.
Pre and post assessment of each participant in both groups were done through using inclinometer, Visual analog scale (VAS), Oswestry Disability questionnaire (OSI) and Standing Finger to ground Distance (SFGD).
The subject was positioned supine on a plinth with a pillow under their head, their arms at their sides, their trunk in neutral posture with no lateral rotation or flexion, and their hips in a neutral position. Then, the test leg’s tibial tuberosity of the participant was immediately marked with an adhesive marker. When the participant initially reported feeling either stretched out or uncomfortable, that was used to establish the PSLR movement’s end point.
For SFGD test the participants were asked to stand behind a line with their feet shoulder width a part in order to measure standing finger to ground distance. The subject was then asked to bend forward to touch the ground with fingers keeping the knee extended. The researcher measured the distance from the tip of the subject’s finger and the ground with a handheld ruler. Three readings were recorded to allow an average of the readings to be calculated.
Scoring Method for Oswestry Disability Questionnaire:
For each subdivision the total possible score is 5: if the first statement is marked the section score = 0; if the last statement is marked, it = 5. If all 10 sections are filled the score is calculated as follows:
- Example: 16 (total scored)
- 50 (total possible score) x 100 = 32%
- If one section is missed or not relevant the score is calculated:
16 (total scored)
45 (total possible score) x 100 = 35.5%
Least detectable change (90% confidence): 10% points (change of less than this may be attributable to error in the measurement). SPSS version 20.0 was used for data analysis. All continuous variables were reported as Mean and Standard Deviation. Normality of data was checked by using Kolmogorov Smirnov test. The data was found to be normally distributed. To know the significance between two groups independent sample t test was applied. Pre & Post comparison was checked through Paired sample t test. P-value ≤ 0.05 considered to be statistically significant.
Stretching Protocol
The active static stretching exercises were performed in the following order with holding duration of 30 seconds. 3 sets of each exercise were performed with 30 seconds of rest between sets. The exercises were performed 5 days for 4 week.
- Unilateral standing hamstring stretch (performed on both legs);
- Bilateral stretching while sitting in a stool/chair;
- Unilateral stretching while lying supine (performed on both legs);
- Bilateral standing hamstring stretch21.

Inclusion Criteria
Housewives aged between 20 to 55 years with non-specific low back pain and having Passive Straight Leg Raise (PSLR) angle < 80 degrees and Standing Finger to Ground Distance (SFGD) greater than 0 cm were included in present study.
Exclusion Criteria
Participants having non-mechanical pain (unrelated to time or activity), having any previous history of carcinoma, steroids, prolapsed intervertebral disc (PIVD), structural Spinal deformity, wide spread neurological symptoms, radiating pain to foot or toes, numbness and paresthesia along the nerve distribution were excluded from the study.
Results
A total of 30 participants aged 20-55 were included in the study. Mean age of the participants was found to be 37.88 years. Pre and post assessment of control and treatment group were separately analyzed.
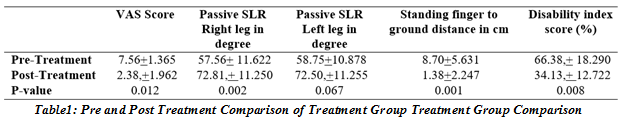
In treatment group, VAS pre score was 7.56 + 1.365 and VAS post score was 2.38 + 1.962 with significant P-value 0.012. Passive Straight Leg Raise (SLR) Right leg was found to be 57.56+ 11.622 degrees in pre session and 72.81+ 11.250 degrees in post session with significant P-value of 0.002. Passive SLR Left leg was observed to be 58.75 + 10.878 degrees in pre assessment and 72.50 + 11.255 degrees in post assessment with not significant p-value of 0.067. Standing finger to ground distance was found to be 8.70 + 5.631 cm in pre-treatment and 1.38 + 2.247 cm in post-
treatment with significant p-value of 0.001. Disability index was pre assessed as 66.38+ 18.290 and post-treatment was 34.13+ 12.722 with significant p-value of 0.008, see Table 1.
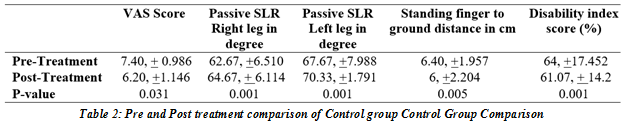
In control group, VAS pre score was 7.40 + 0.986 and VAS post score was 6.20 +1.146 with significant P-value 0.031. Passive SLR Right leg was found to be 62.67 +6.510 degrees in pre session and 64.67 + 6.114 degrees in post session with significant P-value of 0.001. Passive SLR Left leg was observed 67.67 +7.988 degrees in pre assessment and 70.33 +1.791degrees in post assessment with significant p-value of 0.001. Standing finger to ground distance was found 6.40 +1.957 cm in pre-treatment and 6.0 +2.204 cm in post-treatment with significant p-value of 0.005. Disability index was pre assessed as 64.0 +17.452 and post-treatment was 61.07 + 14.2 with significant p-value of 0.001, see Table 2.
Discussion
This study sought to determine the impact of static hamstring stretching on generalized low back pain. This study was quantitative and focused on women. Standing finger to ground distance of more than 0 cm and PSLR of less than 80° are both indicators of reduced hamstring flexibility. This study demonstrated that static hamstring stretching raised PSLR and dramatically decreased SFGD, indicating increased hamstring flexibility. The VAS scores and degree of disability had also decreased, according to this study.
Hamstring extensibility has been suggested as a risk factor for accidents, non-specific low back pain, and alterations in lumbo-pelvic rhythm, making it an essential variable. Hamstring flexibility is diminished in low back pain patients22. Hamstring tightness could be one of the reasons of the Low back pain can become chronic if hamstring tightness is not treated, and it may be one of the causes of developing low back pain.
The Oswestry Disability Questionnaire was utilised to measure functional disability caused by low back pain, while a visual analogue scale was used to measure pain in the current investigation. The visual analogue scale is a trustworthy instrument for both acute and chronic pain. (Hall, 2002) According to a pain rating scale, our study indicated that the treatment group that followed a stretching programme for five days experienced a considerable reduction in pain. It’s possible that the combined effects of conventional physiotherapy treatment and the stretching procedure used in this study contributed to the intra-group reduction in VAS scores. 48 patients with chronic low back pain were randomly assigned to three groups by Marchand et al (TENS, placebo and control). They discovered a 43% reduction in pain intensity on the VAS in the TENS group and a 17% reduction in the placebo group when they compared TENS with placebo. These observed results are consistent with those of Pratik A. et al., who found that Mulligan’s two-legged rotation technique and short wave diathermy had a combined impact to reduce pain as measured by the VAS scale23,24. Same observations were noted in present study as lowering the disability index by 32%, Oswestry Disability scores also demonstrate a significant decline in the degree of disability in present study.
In a study, Pratik A. et al. found that the Modified Oswestry Disability Questionnaire’s Disability scores had significantly decreased, indicating a decrease in the severity of the disability. Additionally, our study showed an increase in the standing finger-to-ground distance. All of the individuals had a finger-to-ground distance of more than 0 cm at the outset. Their standing finger to ground distance dramatically decreased after following the stretching regimen for 5 days, improving hamstring flexibility25.
Our study also demonstrated improvements in standing finger to ground distance. At the beginning all the participants had a finger to ground distance greater than 0 cm. After performing stretching protocol for 5days their standing finger to ground distance significantly decreased which shows improvements in hamstring flexibility. According to Sarah Bellew’s research there is a correlation between less pelvic rotation and a smaller range of forward bending and less hamstring flexibility. According to that study, forward bending is a motion used in daily tasks like lifting something up off the ground. Enhancing hamstring flexibility in people with low back pain may enable more pelvic motion around the hips during forward bending, which relieves pressure on the spine’s and legs’ posterior components thus reduce pain26. Farooqi S. et al. et al. conducted research on university students with non-specific low back pain to test hamstring flexibility retention with sit-and-reach boxes. The study’s findings revealed that after a sit and reach box training regimen of four weeks, most candidates’ flexibility significantly improved on their fifth attempt. After a stretching session, flexibility gains were maintained for two weeks27. Flexibility improvements are kept for at least two weeks. Additionally, it gave the idea that gaining a significant increase in flexibility only required 2 sets, each consisting of 3 repeats of the sit-and-reach test27,28.
Conclusion
The present study concluded that static stretching of hamstring is effective in reducing non-specific low back pain and increasing the extensibility of hamstring among housewives.
Limitations of the study
- The study was single centered.
- Small sample size.
- Only females were included.
Strength of the study
- Generalized to single muscle work
- Limited work done locally as far as our best knowledge.
Recommendations
- Large sample size with both genders.
- Can be multi centered.
AUTHORS’ CONTRIBUTION:
The following authors have made substantial contributions to the manuscript as under:
Conception or Design: Syeda Anum Riaz, Muhammad Usman
Acquisition, Analysis or Interpretation of Data: Muhammad Usman
Manuscript Writing & Approval: Syeda Anum Riaz
All authors acknowledge their accountability for all facets of the research, ensuring that any concerns regarding the accuracy or integrity of the work are duly investigated and resolved.
ACKNOWLEDGEMENTS: We thanks all the participants in this study.
INFORMED CONSENT: Written Informed Consent was taken from each patient.
CONFLICT OF INTEREST: The author (s) have no conflict of interest regarding any of the activity perform by PJR.
FUNDING STATEMENTS: None declared
ETHICS STATEMENTS: The study has been approved by the Ethical Board of Rabia Moon Institute of Neurology.
References
- Okereke S, Gregory M. DVT pathway audit. Clinical Radiology. 2020 Dec 1;75:e14.
- Wu A, March L, Zheng X, Huang J, Wang X, Zhao J, Blyth FM, Smith E, Buchbinder R, Hoy D.
- Global low back pain prevalence and years lived with disability from 1990 to 2017: estimates from the Global Burden of Disease Study 2017. Annals of translational medicine. 2020 Mar;8(6).
- Ijaz M, Akram M, Ahmad SR, Mirza K, Ali Nadeem F, Thygerson SM. Risk Factors Associated with the Prevalence of Upper and Lower Back Pain in Male Underground Coal Miners in Punjab, Pakistan. International Journal of Environmental Research and Public Health. 2020 Jan;17(11):4102.
- Wong CK, Mak RY, Kwok TS, Tsang JS, Leung MY, Funabashi M, Macedo LG, Dennett L, Wong AY. Prevalence, incidence, and factors associated with non-specific chronic low back pain in community-dwelling older adults aged 60 years and older: a systematic review and meta-analysis. The journal of pain. 2021 Aug 24.
- Grabovac I, Dorner TE. Association between low back pain and various everyday performances. Wiener klinische Wochenschrift. 2019 Nov;131(21):541-9.
- Waseem M, Karimi H, Gilani SA, Hassan D. Treatment of disability associated with chronic non-specific low back pain using core stabilization exercises in Pakistani population. Journal of Back and Musculoskeletal Rehabilitation. 2019 Jan 1;32(1):149-54.
- Napoli A, Alfieri G, Scipione R, Andrani F, Leonardi A, Catalano C. Pulsed radiofrequency for low-back pain and sciatica. Expert Review of Medical Devices. 2020 Feb 1;17(2):83-6.
- Skorupska E. Muscle atrophy measurement as assessment method for low back pain patients. Muscle Atrophy. 2018:437-61.
- Urits I, Burshtein A, Sharma M, Testa L, Gold PA, Orhurhu V, Viswanath O, Jones MR, Sidransky MA, Spektor B, Kaye AD. Low back pain, a comprehensive review: pathophysiology, diagnosis, and treatment. Current pain and headache reports. 2019 Mar;23(3):1-0.
- Hashem LE, Roffey DM, Alfasi AM, Papineau GD, Wai DC, Phan P, Kingwell SP, Wai EK. Exploration of the inter-relationships between obesity, physical inactivity, inflammation, and low back pain. Spine. 2018 Sep 1;43(17):1218-24.
- Vatandoost S, Sheikhhoseini R, Akhbari B, Salavati M, Pourahmadi M, Farhang M, O’Sullivan K. Altered muscle strength and flexibility among a subgroup of women with chronic nonspecific low back pain: Cross-sectional case-control study. Physiotherapy Theory and Practice. 2022 Feb 23:1-9.
- Kim B, Yim J. Core stability and hip exercises improve physical function and activity in patients with non-specific low back pain: a randomized controlled trial. The Tohoku journal of experimental medicine. 2020;251(3):193-206.
- Shamsi M, Mirzaei M, Khabiri SS. Universal goniometer and electro-goniometer intra-examiner reliability in measuring the knee range of motion during active knee extension test in patients with chronic low back pain with short hamstring muscle. BMC Sports Science, Medicine and Rehabilitation. 2019 Dec;11(1):1-5.
- Zawadka M, Skublewska-Paszkowska M, Gawda P, Lukasik E, Smolka J, Jablonski M. What factors can affect lumbopelvic flexion-extension motion in the sagittal plane?: A literature review. Human movement science. 2018 Apr 1;58:205-18.
- Gaur VV, Kapoor AA, Phansopkar PA. Short term effects of muscle energy technique vs. active release technique in improving hamstring flexibility and pain in patients with acute anterior cruciate ligament (ACL) tear-a randomized control trial. J Evol Med Dent Sci. 2021 Jan 18;10(3):137-42.
- Ballard MT, Drury C, Bazrgari B. Changes in Lumbo-Pelvic Coordination of Individuals With and Without Low Back Pain When Wearing a Hip Orthosis. Frontiers in Sports and Active Living. 2020 Jul 16;2:90.
- Lathuilière S, Mesejo P, Alameda-Pineda X, Horaud R. A comprehensive analysis of deep regression. IEEE transactions on pattern analysis and machine intelligence. 2019 Apr 11;42(9):2065-81.
- Hansberger BL, Loutsch R, Hancock C, Bonser R, Zeigel A, Baker RT. Evaluating the relationship between clinical assessments of apparent hamstring tightness: a correlational analysis. International Journal of Sports Physical Therapy. 2019 Apr;14(2):253.
- Santonja-Medina F, Santonja-Renedo S, Cejudo A, Ayala F, Ferrer V, Pastor A, Collazo-Diéguez M, Rodríguez-Ferrán O, Andújar P, Sainz de Baranda P. Straight Leg Raise Test: Influence of Lumbosant© and Assistant Examiner in Hip, Pelvis Tilt and Lumbar Lordosis. Symmetry. 2020 Jun;12(6):927.
- Bansal D, Asrar MM, Pharm M, Ghai B, Pushpendra D. Prevalence and impact of low back pain in a community-based population in northern India. Pain Physician. 2020;23(4):E389.
- Kim B, Yim J. Core stability and hip exercises improve physical function and activity in patients with non-specific low back pain: a randomized controlled trial. The Tohoku journal of experimental medicine. 2020;251(3):193-206.
- Cejudo A, Centenera-Centenera JM, Santonja-Medina F. The Potential Role of Hamstring Extensibility on Sagittal Pelvic Tilt, Sagittal Spinal Curves and Recurrent Low Back Pain in Team Sports Players: A Gender Perspective Analysis. International Journal of Environmental Research and Public Health. 2021 Jan;18(16):8654.
- Choi YJ, Sim HP, Lee JY. The Comparison of Effects Mulligan’s Technique Applied to Shortened Hamstring. The Journal of Korean Academy of Orthopedic Manual Physical Therapy. 2018;24(1):7-14.
- Razzaq M, Bhatti ZM, Nawaz U, Ghani HM. Comparative Effects of Mulligan’s Two Leg Rotation Technique and Muscle Energy Technique on Hamstring Flexibility. Pakistan Journal of Medical & Health Sciences. 2022 May 26;16(05):102-.
- Waseem M, Karimi H, Gilani SA, Hassan D. Treatment of disability associated with chronic non-specific low back pain using core stabilization exercises in Pakistani population. Journal of back and musculoskeletal rehabilitation. 2019;32(1):149-54.
- Garcia MC, Lennon A, Bazett-Jones DM, Ford KR, Long JT, Taylor-Haas JA. Influence of hamstring flexibility on running kinematics in adolescent long-distance runners. Gait & Posture. 2022 Mar 1;93:107-12.
- Sumaira Imran Farooqui, Zulekha Saleem, Ashbeel John Edgar, Shahida Abbass. Assessment of hamstring flexibility retention through sit-and-reach box in university students with nonspecific low back pain. 2020];5(1):31-8.
The Ziauddin University is on the list of I4OA, I4OC, and JISC.
This is an open- access article distributed under the terms of the Creative Commons Attribution License (CC BY 4.0).
